Infectious Diseases & Pandemics
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

J. Michael Mcginnis, Md, Ma, Mpp
J. MICHAEL MCGINNIS, MD, MA, MPP National Academy of Medicine, the National Academies, 500 Fifth Street NW, Washington DC 20001, (202) 334-3963, [email protected] Highlights: Michael McGinnis is a physician and epidemiologist who lives and works in Washington DC. Through his writing, government service, and work in philanthropy, he has been a long-time contributor to national and international field leadership in health, health care, and health policy. He currently serves at the National Academy of Medicine (NAM), where he is the Leonard D. Schaeffer Executive Officer, Senior Scholar, and Executive Director of the NAM’s Leadership Consortium for public and private collaboration on behalf of a continuously learning health system. Previously, he served as founding Director, respectively, of the Robert Wood Johnson Foundation’s (RWJF) Health Group, the World Health Organization’s Office for Health Reconstruction in Bosnia, the federal Office of Research Integrity (interim), and the federal Office of Disease Prevention and Health Promotion. In a tenure unusual for political and policy posts, he held continuous appointment through the Carter, Reagan, Bush and Clinton Administrations at the Department of Health and Human Services, with policy responsibilities for disease prevention and health promotion (1977-1995). Programs and policies conceived and launched at his initiative include the Healthy People process establishing national health goals and objectives (1979-present), the U.S. Preventive Services Task Force (1984-present), the Dietary Guidelines for Americans (with USDA, 1980- present), the multi-level Public Health Functions Steering Group and the Ten Essential Services of Public Health (1994-present), the RWJF Active Living family of programs (2000-present), the RWJF Young Epidemiology Scholars Program (2001-2012), the RWJF Health and Society Scholars Program (2002-2017), and the current Learning Health System initiative of the NAM. -

(ITFDE) October 22, 2019
Summary of the Thirtieth Meeting of the International Task Force for Disease Eradication (ITFDE) October 22, 2019 The 30th Meeting of the International Task Force for Disease Eradication (ITFDE) was convened at The Carter Center in Atlanta, GA, USA from 8:30 am to 5:00 pm on October 22, 2019 to discuss the potential for eradication of measles and rubella. The Task Force members are Dr. Stephen Blount, The Carter Center (Chair); Dr. Peter Figueroa, The University of the West Indies, Jamaica; Dr. Donald Hopkins, The Carter Center; Dr. Fernando Lavadenz, The World Bank; Dr. Mwelecele Malecela, World Health Organization (WHO); Professor David Molyneux, Liverpool School of Tropical Medicine; Dr. Ana Morice, Independent Consultant; Dr. Stefan Peterson, UNICEF; Dr. David Ross, The Task Force for Global Health; Dr. William Schluter, Centers for Disease Control and Prevention (CDC); Dr. Nilanthi de Silva, University of Kelaniya, Sri Lanka/WHO Strategic and Technical Advisory Group for Neglected Tropical Diseases (STAG-NTDs); Dr. Dean Sienko, The Carter Center; Dr. Laurence Slutsker, PATH; Dr. Jordan Tappero, Bill & Melinda Gates Foundation; Dr. Ricardo Thompson, National Institute of Health (Mozambique); and Dr. Dyann Wirth, Harvard School of Public Health. Eleven Task Force members (Blount, Figueroa, Hopkins, Morice, Ross, Sienko, de Silva, Slutsker, Tappero, Thompson, Wirth) participated in this meeting; three were represented by an alternate (Drs. Fatima Barry for Lavadenz, Steve Cochi for Schluter, Yodit Sahlemariam for Peterson). Presenters included Drs. Sunil Bahl, WHO/SEARO; Amanda Cohn, CDC; Matthew Hanson, Bill & Melinda Gates Foundation; Alan Hinman, The Task Force for Global Health; Mark Jit, London School of Tropical Medicine & Hygiene; Ann Lindstrand, WHO/Geneva; Balcha Masresha, WHO/AFRO; Patrick O’Connor, WHO/Europe; and Desiree Pastor, Pan American Health Organization (WHO/PAHO). -

THE SURGEON GENERAL and the BULLY PULPIT Michael Stobbe a Dissertation Submitted to the Faculty of the University of North Carol
THE SURGEON GENERAL AND THE BULLY PULPIT Michael Stobbe A dissertation submitted to the faculty of the University of North Carolina at Chapel Hill in partial fulfillment of the requirements for the degree of Doctor of Public Health in the Department of Health Policy and Administration, School of Public Health Chapel Hill 2008 Approved by: Ned Brooks Jonathan Oberlander Tom Ricketts Karl Stark Bryan Weiner ABSTRACT MIKE STOBBE: The Surgeon General and the Bully Pulpit (Under the direction of Ned Brooks) This project looks at the role of the U.S. Surgeon General in influencing public opinion and public health policy. I examined historical changes in the administrative powers of the Surgeon General, to explain what factors affect how a Surgeon General utilizes the office’s “bully pulpit,” and assess changes in the political environment and in who oversees the Surgeon General that may affect the Surgeon General’s future ability to influence public opinion and health. This research involved collecting and analyzing the opinions of journalists and key informants such as current and former government health officials. I also studied public documents, transcripts of earlier interviews and other materials. ii TABLE OF CONTENTS LIST OF TABLES.................................................................................................................v Chapter 1. INTRODUCTION ...............................................................................................1 Background/Overview .........................................................................................1 -

THE SURGEON GENERAL and the BULLY PULPIT Michael Stobbe a Dissertation Submitted to the Faculty of the University of North Carol
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Carolina Digital Repository THE SURGEON GENERAL AND THE BULLY PULPIT Michael Stobbe A dissertation submitted to the faculty of the University of North Carolina at Chapel Hill in partial fulfillment of the requirements for the degree of Doctor of Public Health in the Department of Health Policy and Administration, School of Public Health Chapel Hill 2008 Approved by: Ned Brooks Jonathan Oberlander Tom Ricketts Karl Stark Bryan Weiner ABSTRACT MIKE STOBBE: The Surgeon General and the Bully Pulpit (Under the direction of Ned Brooks) This project looks at the role of the U.S. Surgeon General in influencing public opinion and public health policy. I examined historical changes in the administrative powers of the Surgeon General, to explain what factors affect how a Surgeon General utilizes the office’s “bully pulpit,” and assess changes in the political environment and in who oversees the Surgeon General that may affect the Surgeon General’s future ability to influence public opinion and health. This research involved collecting and analyzing the opinions of journalists and key informants such as current and former government health officials. I also studied public documents, transcripts of earlier interviews and other materials. ii TABLE OF CONTENTS LIST OF TABLES.................................................................................................................v Chapter 1. INTRODUCTION ...............................................................................................1 -

Distribution Agreement in Presenting This Thesis Or Dissertation As A
Distribution Agreement In presenting this thesis or dissertation as a partial fulfillment of the requirements for an advanced degree from Emory University, I hereby grant to Emory University and its agents the non-exclusive license to archive, make accessible, and display my thesis or dissertation in whole or in part in all forms of media, now or hereafter known, including display on the world wide web. I understand that I may select some access restrictions as part of the online submission of this thesis or dissertation. I retain all ownership rights to the copyright of the thesis or dissertation. I also retain the right to use in future works (such as articles or books) all or part of this thesis or dissertation. Signature: _____________________________ ______________ Anita L. Renahan-White Date Faith and the Public's Health By Anita L. Renahan-White Master of Divinity Candler School of Theology ___________________________________________ [Thesis Advisor's signature] Dr. John Blevins Committee Chair ___________________________________________ [Member's signature] Dr. Steven J. Kraftchick Director of General and Advanced Studies ___________________________________________ [Member's signature] Dr. Emmanuel Lartey Committee Member Faith and the Public's Health By Anita L. Renahan-White MPH Emory University 1993 Thesis Committee Chair: John Blevins, ThD An abstract of A thesis submitted to the Faculty of the Candler School of Theology in partial fulfillment of the requirements for the degree of Master of Divinity 2012 Abstract Faith and the Public's Health By Anita L. Renahan-White In the following thesis "Faith and the Public's Health," I detail findings from research and interviews I conducted from March 2011 through February 2012. -
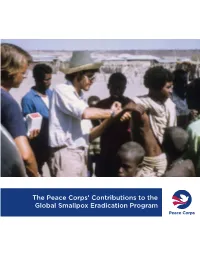
The Peace Corps' Contributions to the Global Smallpox Eradication Program
The Peace Corps’ Contributions to the Global Smallpox Eradication Program About the Office of Strategic Information, Research, and Planning (OSIRP) It is the mission of OSIRP to advance evidence-based management at the Peace Corps by guiding agency strategic planning; monitoring and evaluating agency-level performance and programs; conducting research to generate new insights in the fields of international development, cultural exchange, and Volunteer service; enhancing the stewardship and governance of agency data; and helping to shape agency engagement on high-level, governmentwide initiatives. Front Cover: Peace Corps Volunteers Robert Steinglass and Doug Arbuckle administering the smallpox vaccine in Mille, Ethiopia, in 1974. Photo: Steinglass, personal collection. ii Dedication This report is dedicated to the memory of Dr. Donald Ainslie “D. A.” Henderson (September 7, 1928—August 19, 2016), a seminal figure in the field of smallpox eradication. The Peace Corps is deeply appreciative of having had the opportunity to correspond with Dr. Henderson about the contributions of Peace Corps Volunteers and returned Volunteers within the context of the global eradication program. His charismatic leadership, tireless energy, and unflagging devotion to this program inspired countless public health workers around the world, including many of the returned Peace Corps Volunteers interviewed for this report. iii Acknowledgments In 1806, approximately 10 years after Dr. Edward Jenner conducted the first documented experiment with smallpox vaccination, laying the foundations of modern medicine, President Thomas Jefferson wrote to the English physician and scientist. Jefferson acknowledged the importance of this discovery, extending “a portion of the tribute of gratitude due to you from the whole human family. -

Seamus Heaney Exhibit Is Tribute to Friend of Emory Emory Photo Video
Welcome to spring semester SPECIAL ISSUE Online all the time at news.emory.edu JANUARY 21, 2014 ATHLETICS BEARDEN EXHIBIT Oxford’s organic farm 2 Eagle teams ‘Black Odyssey’ return strong draws scholars, Spring break alternatives 5 for 2014. faculty and local Calendar highlights 6-7 Page 3 celebrities. Page 12 Founders Week 11 University Course expands 11 Seamus Heaney exhibit is tribute to friend of Emory Emory Photo Video Nobel Prize-winning poet Seamus Heaney had a long relationship with Emory, having presented the inaugural Richard Ellmann Lectures. By MAUREEN MCGAVIN beginning at 6 p.m. with W. Ronald Schuchard, Emory profes- were part of an old bench from Carysfort College in Dublin, sor emeritus of English, as toastmaster. where Heaney taught in the 1970s. “Seamus Heaney: The Music of What Happens,” opening Geraldine Higgins, director of Emory’s Irish studies pro- There will also be a custom-built media space where people Saturday, Feb. 22, will be Emory’s first major exhibition cel- gram, curated the exhibition, choosing the title from a line can listen to recordings of Heaney and other distinguished writ- ebrating the life of the late Irish poet and Nobel Prize winner. in the Heaney poem “Song:” “The finest music of all is the ers, artists and well-known figures, including Irish actor Liam Heaney had a special connection to Emory beginning music of what happens.” Neeson and novelist Sir Salman Rushdie, reading his poems. with his first reading in March 1981. He delivered the inau- The exhibition will showcase Heaney’s poems and drafts A large kite will be at the center of the exhibition, suspended gural Richard Ellmann Lectures in Modern Literature in showing his handwritten revisions, rare publications, and over the spiral staircase in the gallery that descends to the lower 1988, donated his lecture notes to Emory’s Manuscript, artists’ books containing his poetry. -

Proquest Dissertations
'RANDOM MURDER BY TECHNOLOGY': THE ROLE OF SCIENTIFIC AND BIOMEDICAL EXPERTS IN THE ANTI-NUCLEAR MOVEMENT, 1969 - 1992 LISA A. RUMIEL A DISSERTATION SUBMITTED TO THE FACULTY OF GRADUATE STUDIES IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY GRADUATE PROGRAM IN HISTORY YORK UNIVERSITY, TORONTO, ONTARIO AUGUST 2009 Library and Archives Bibliotheque et 1*1 Canada Archives Canada Published Heritage Direction du Branch Patrimoine de I'edition 395 Wellington Street 395, rue Wellington OttawaONK1A0N4 Ottawa ON K1A 0N4 Canada Canada Your file Votre reference ISBN: 978-0-494-54104-3 Our file Notre r6f6rence ISBN: 978-0-494-54104-3 NOTICE: AVIS: The author has granted a non L'auteur a accorde une licence non exclusive exclusive license allowing Library and permettant a la Bibliotheque et Archives Archives Canada to reproduce, Canada de reproduire, publier, archiver, publish, archive, preserve, conserve, sauvegarder, conserver, transmettre au public communicate to the public by par telecommunication ou par I'lnternet, preter, telecommunication or on the Internet, distribuer et vendre des theses partout dans le loan, distribute and sell theses monde, a des fins commerciales ou autres, sur worldwide, for commercial or non support microforme, papier, electronique et/ou commercial purposes, in microform, autres formats. paper, electronic and/or any other formats. The author retains copyright L'auteur conserve la propriete du droit d'auteur ownership and moral rights in this et des droits moraux qui protege cette these. Ni thesis. Neither the thesis nor la these ni des extraits substantiels de celle-ci substantial extracts from it may be ne doivent etre imprimes ou autrement printed or otherwise reproduced reproduits sans son autorisation. -

Controlling Onchocerciasis (River Blindness) in Sub-Saharan Africa
Case 7 Controlling Onchocerciasis (River Blindness) in Sub-Saharan Africa Geographic area: Sub-Saharan Africa Health condition: In west African countries in 974, nearly 2 million of the area’s 20 million inhabit- ants were infected with onchocerciasis, and approximately 200,000 were blind. Global importance of the health condition: Onchocerciasis, or river blindness, afflicts approximately 42 mil- lion people worldwide, with well over 99 percent of its victims in sub-Saharan Africa. An estimated 600,000 people are blind, and an additional .5 million Africans are visually impaired due to onchocerciasis. Intervention or program: The Onchocerciasis Control Program (OCP) was launched in 974 in west African countries. Weekly aerial spraying with environmentally safe insecticides helped control the dis- ease vector—blackflies that bred in fast-moving waterways, thereby halting transmission of the disease. In 995, a second program, the African Programme for Onchocerciasis Control (APOC), was established to control the disease in 9 central, east, and southern African countries. Through a broad international partnership and the participation of 5,000 remote, rural communities, APOC and OCP distributed a drug donated by Merck & Co., Inc., Mectizan (ivermectin), to more than 45 million people in sub-Saharan Africa in 2005. The drug prevents and alleviates the symptoms of the disease with one annual dose. Cost-effectiveness: OCP operated with an annual cost of less than $ per protected person. Commit- ments from 27 donors during the 28-year project totaled $600 million. The annual return on investment was calculated to be about 20 percent, primarily attributable to increased agricultural output; about $3.7 billion will be generated from improved labor and agricultural productivity. -

Disease Strategy Debated
MONDAY, MARCH 20, 2006 To Conquer, or Control? Disease Strategy Debated By DONALD G. McNEIL Jr and CELIA W. DUGGER Other Likely Candidates for Eradication There is a heroic allure to ridding the planet of a horrible disease forever. DISEASE EST. CASES TRANSMISSION BREAKING THE CYCLE Louis Pasteur is famous as the inventor of the vaccine. Jonas Salk is synonymous Guinea worm 12,000 Worm larvae in water Filter or treat pond water. with the one he created to combat polio. fleas swallowed by Dig deep wells so they do In the medical community, doctors like humans. Worms can not get contaminated. Donald A. Henderson and William Foege grow three feet long. are honored as the conquerors of smallpox. Lymphatic 120 million Mosquitoes carry juvenile Deworming pills kill Though the dream of eradication filariasis (1996) worms. Adult worm nests juvenile worms, but victims continues to animate scientists, doctors swell legs and scrotums, must be treated annually and public health officials, the history crippling victims. for 6 years. is at best rocky. In the past century, erad- ication efforts failed against hookworm, yellow fever and malaria. Today the struggling drive against polio has raised new questions about whether eradication of any disease is achievable, and, if so, whether the cost in terms of effort and dollars would be worth it, given all the A woman with other diseases that need attention. lymphatic filariasis The latest push began in 1993, when in Haiti. the International Task Force for Disease Eric S. Lesser for The New York Times Eradication, a panel of experts, was convened in Atlanta by the Centers for Measles 30 million Virus spread by Vaccine delivered Disease Control and Prevention, Emory annual cases; coughing, sneezing by injection. -

Worldwide Smallpox Eradication, 1957–67
Med. Hist. (2020), vol. 64(1), pp. 71–93. c The Authors 2019. Published by Cambridge University Press 2019 This is an Open Access article, distributed under the terms of the Creative Commons Attribution licence (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted re-use, distribution, and reproduction in any medium, provided the original work is properly cited. doi:10.1017/mdh.2019.77 Re-assessing the Foundations: Worldwide Smallpox Eradication, 1957–67 SANJOY BHATTACHARYA 1* and CARLOS EDUARDO D’AVILA PEREIRA CAMPANI 2 1Centre for Global Health Histories, Department of History, University of York, York YO10 5DD, UK 2Department of Health Sciences, University of York, York YO10 5DD, UK Abstract: An expansive, worldwide smallpox eradication programme (SEP) was announced by the World Health Assembly in 1958, leading this decision-making body to instruct the World Health Organization Headquarters in Geneva to work with WHO regional offices to engage and draw in national governments to ensure success. Tabled by the Soviet Union’s representative and passed by a majority vote by member states, the announcement was subject to intense diplomatic negotiations. This led to the formation, expansion and reshaping of an ambitious and complex campaign that cut across continents and countries. This article examines these inter-twining international, regional and national processes, and challenges long-standing historiographical assumptions about the fight against smallpox only gathering strength from the mid-1960s onwards, after the start of a US-supported programme in western Africa. The evidence presented here suggests a far more complex picture. It shows that although the SEP’s structures grew slowly between 1958 and 1967, a worldwide eradication programme resulted from international negotiations made possible through gains during this period. -

Religious Conviction and the Boston Inoculation Controversy of 1721
W&M ScholarWorks Undergraduate Honors Theses Theses, Dissertations, & Master Projects 5-2011 Religious Conviction and The Boston Inoculation Controversy of 1721 Anna E. Storm College of William and Mary Follow this and additional works at: https://scholarworks.wm.edu/honorstheses Part of the History Commons Recommended Citation Storm, Anna E., "Religious Conviction and The Boston Inoculation Controversy of 1721" (2011). Undergraduate Honors Theses. Paper 400. https://scholarworks.wm.edu/honorstheses/400 This Honors Thesis is brought to you for free and open access by the Theses, Dissertations, & Master Projects at W&M ScholarWorks. It has been accepted for inclusion in Undergraduate Honors Theses by an authorized administrator of W&M ScholarWorks. For more information, please contact [email protected]. Religious Conviction and The Boston Inoculation Controversy of 1721 A thesis submitted in partial fulfillment of the requirement for the degree of Bachelors of Arts in History from The College of William and Mary Anna Storm Accepted for _________________________________ (Honors, High Honors, Highest Honors) __________________________ Paul Mapp, Director __________________________ Chandos Brown __________________________ Randolph Coleman Williamsburg, VA April 25, 2011 2 Introduction “Ultimately, society must recognize that science is not a democracy in which the side with the most votes or the loudest voices gets to decide what is right.”1 This quote is part of a larger article, “The Age-Old Struggle against the Antivaccinationists,” published on January 13, 2011 in the New England Journal of Medicine. Written by Gregory A Poland, M.D., and Robert M. Jacobson, M.D., the article discusses the problem of “antivaccinationists,” or people who use fear to deter society from vaccinating themselves and their families.