TAUC X-Ray Training Compendium
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Medical Policy Ultrasound Accelerated Fracture Healing Device
Medical Policy Ultrasound Accelerated Fracture Healing Device Table of Contents Policy: Commercial Coding Information Information Pertaining to All Policies Policy: Medicare Description References Authorization Information Policy History Policy Number: 497 BCBSA Reference Number: 1.01.05 Related Policies Electrical Stimulation of the Spine as an Adjunct to Spinal Fusion Procedures, #498 Electrical Bone Growth Stimulation of the Appendicular Skeleton, #499 Bone Morphogenetic Protein, #097 Policy Commercial Members: Managed Care (HMO and POS), PPO, and Indemnity Members Low-intensity ultrasound treatment may be MEDICALLY NECESSARY when used as an adjunct to conventional management (i.e., closed reduction and cast immobilization) for the treatment of fresh, closed fractures in skeletally mature individuals. Candidates for ultrasound treatment are those at high risk for delayed fracture healing or nonunion. These risk factors may include either locations of fractures or patient comorbidities and include the following: Patient comorbidities: Diabetes, Steroid therapy, Osteoporosis, History of alcoholism, History of smoking. Fracture locations: Jones fracture, Fracture of navicular bone in the wrist (also called the scaphoid), Fracture of metatarsal, Fractures associated with extensive soft tissue or vascular damage. Low-intensity ultrasound treatment may be MEDICALLY NECESSARY as a treatment of delayed union of bones, including delayed union** of previously surgically-treated fractures, and excluding the skull and vertebra. 1 Low-intensity ultrasound treatment may be MEDICALLY NECESSARY as a treatment of fracture nonunions of bones, including nonunion*** of previously surgically-treated fractures, and excluding the skull and vertebra. Other applications of low-intensity ultrasound treatment are INVESTIGATIONAL, including, but not limited to, treatment of congenital pseudarthroses, open fractures, fresh* surgically-treated closed fractures, stress fractures, arthrodesis or failed arthrodesis. -

CASE REPORT Injuries Following Segway Personal
UC Irvine Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health Title Injuries Following Segway Personal Transporter Accidents: Case Report and Review of the Literature Permalink https://escholarship.org/uc/item/37r4387d Journal Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health, 16(5) ISSN 1936-900X Authors Ashurst, John Wagner, Benjamin Publication Date 2015 DOI 10.5811/westjem.2015.7.26549 License https://creativecommons.org/licenses/by/4.0/ 4.0 Peer reviewed eScholarship.org Powered by the California Digital Library University of California CASE REPORT Injuries Following Segway Personal Transporter Accidents: Case Report and Review of the Literature John Ashurst DO, MSc Conemaugh Memorial Medical Center, Department of Emergency Medicine, Benjamin Wagner, DO Johnstown, Pennsylvania Section Editor: Rick A. McPheeters, DO Submission history: Submitted April 20, 2015; Accepted July 9, 2015 Electronically published October 20, 2015 Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.2015.7.26549 The Segway® self-balancing personal transporter has been used as a means of transport for sightseeing tourists, military, police and emergency medical personnel. Only recently have reports been published about serious injuries that have been sustained while operating this device. This case describes a 67-year-old male who sustained an oblique fracture of the shaft of the femur while using the Segway® for transportation around his community. We also present a review of the literature. [West J Emerg Med. 2015;16(5):693-695.] INTRODUCTION no parasthesia was noted. In 2001, Dean Kamen developed a self-balancing, zero Radiograph of the right femur demonstrated an oblique emissions personal transportation vehicle, known as the fracture of the proximal shaft of the femur with severe Segway® Personal Transporter (PT).1 The Segway’s® top displacement and angulation (Figure). -

Clinical Efficacy of Extended Modified Posteromedial Approach Versus
Clinical ecacy of extended modied posteromedial approach versus posterolateral approach for surgical treatment of posterior pilon fracture: a retrospective analysis Qin-Ming Zhang Aliated Hospital of Jining Medical University Hai-Bin Wang Aliated Hospital of Jining Medical University Xiao-Yan Li Aliated Hospital of Jining Medical University Feng-Long Chu Aliated Hospital of Jining Medical University Liang Han Aliated Hospital of Jining Medical University Dong-Mei Li Aliated Hospital of Jining Medical University Bin Wu ( [email protected] ) Alited Hospital of Jining Medical University https://orcid.org/0000-0003-3707-0056 Research article Keywords: posterior pilon fracture, approach, fracture xation, buttress plate Posted Date: March 30th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-19392/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/12 Abstract Background: Posterior pilon fracture is a type of ankle fracture associated with poorer treatment results compared to the conventional ankle fracture. This is partly related to the lack of consensus on the classication, approach selection, and internal xation method for this type of fracture. This study aimed to investigate the clinical ecacy of posterolateral approach versus extended modied posteromedial approach for surgical treatment of posterior pilon fracture. Methods: Data of 67 patients with posterior pilon fracture who received xation with a buttress plate between January 2015 and December 2018 were retrospectively reviewed. Patients received steel plate xation through either the posterolateral approach (n = 35, group A) or the extended modied posteromedial approach (n = 32, group B). Operation time, intraoperative blood loss, excellent and good rate of reduction, fracture healing time, American Orthopaedic Foot & Ankle Society (AOFAS) Ankle- Hindfoot Scale score, and Visual Analogue Scale score were compared between groups A and B. -

Hand Rehabilitation Current Awareness Bulletin NOVEMBER 2015
1 Hand Rehabilitation Current Awareness Bulletin NOVEMBER 2015 2 Lunchtime Drop-in Sessions The Library and Information Service provides free specialist information skills training for all UHBristol staff and students. To book a place, email: [email protected] If you’re unable to attend we also provide one-to-one or small group sessions. Contact library@ or katie.barnard@ to arrange a session. Literature Searching October (12pm) An in -depth guide on how to search Thurs 8th Statistics the evidence base, including an introduction to UpToDate and Fri 16th Literature Searching Anatomy.tv. Mon 19th Understanding articles Tues 27th Statistics Useful for anybody who wants to find the best and quickest way to source articles. November (1pm) Weds 4th Literature Searching Thurs 12th Understanding articles How to understand an article Fri 20th Statistics How to assess the strengths and Mon 23rd Literature Searching weaknesses of published articles. Examining bias and validity. December (12pm) Tues 1st Understanding articles Weds 9th Statistics Medi cal Statistics Thurs 17th Literature Searching A basic introduction to the key statistics in medical articles. Giving an overview of statistics that compare risk, test confidence, analyse clinical investigations, and test difference. 3 Contents Contents .................................................................................................................................................. 3 New from Cochrane Database of Systematic Reviews .......................................................................... -

Radial Head Fractures Treated with Open Reduction and Internal Fixation
Moghaddam et al. Trauma Cases Rev 2016, 2:028 Volume 2 | Issue 1 ISSN: 2469-5777 Trauma Cases and Reviews Research Article: Open Access Radial Head Fractures Treated with Open Reduction and Internal Fixation Moghaddam A1*, Raven TF1, Kaghazian P1, Studier-Fischer S2, Swing T1, Grützner PA2 and Biglari B2 1Trauma & Reconstructive Surgery, University hospital Heidelberg, Germany 2BG Unfallklinik, Ludwigshafen, Germany *Corresponding author: Prof. Dr. med. Arash Moghaddam, Consultant Orthopaedic & Trauma Surgeon Center of Trauma, Orthopaedics & Paraplegiology, Division of Trauma & Reconstructive Surgery, University hospital Heidelberg, Schlierbacher Landstraße 200a, 69118 Heidelberg, Germany, Tel: 0049-6221-5626263, Fax: 0049- 6221-26298, E-mail: [email protected] to a high percentage of associated injuries [6]. The combination of a Abstract dislocated fracture and unstable joint makes operative treatment as Background: Radial head fractures are responsible for 2 to 5% of well as early mobilization difficult. Other treatment options include adult fractures. Especially problematic is the treatment of dislocated the implantation of a radial head prosthesis and resection of the and unstable fractures which often have a worst prognosis. The radial head. The radial head prosthesis has become established as the purpose of this study was to evaluate the results of open reduction choice of treatment for multi-fragmented radial head fractures with and internal fixation (ORIF) in the treatment of radial head fractures. associated injuries, while resection of the radial head has increasingly Materials and Methods: Between June 2001 and January 2006, fallen out of use and is now reserved for isolated fractures of the 41 reconstructive surgical procedures were executed. Thirty-seven radial head without associated injuries [7]. -

Del Vecchio Upper Extremity Injury
UPPER EXTREMITY INJURIES Jeff Del Vecchio MPAS, PA-C, DFAAPA Mercy Clinic Orthopedics Springfield, Missouri OBJECTIVES IDENTIFY COMMON UPPER EXTREMITY INJURIES AND FRACTURES REVIEW EXAMINATION TECHNIQUES FOR COMMON UPPER EXTREMITY INJURIES DISCUSS AND REVIEW RADIOGRAPHIC FINDINGS OF UPPER EXTREMITY FRACTURES DISCUSS AND REVIEW TREATMENT OPTIONS FOR COMMON UPPER EXTREMITY INJURIES LATERAL EPICONDYLITIS Tennis elbow Definition Pain about lateral aspect of elbow Involves extensor musculature Rotation of arm and wrist extension Secondary to repetitive overuse or injury Microtears to tendon⇒ inflammation⇒fibrosis⇒degeneration Affects pt’s 30-60 yrs Clinical symptoms Outside elbow and back of upper forearm pain Pain lifting with palm facing down Holding lightweight objects difficult Physical Examination Lateral epicondylar area tender to palpation Tennis elbow test- elbow 90 deg, extend wrist against resistance. +pain at lateral epicondaylar area Radiographs Obtain to rule out osteoarthritis or calcifications Treatment NSAID’s (10-14 days) Avoid activities causing pain Heat or ice Corticosteroid injection Stretching and gradual strengthening program Tennis elbow strap MEDIAL EPICONDYLITIS Golfer’s elbow Definition Inflammation of flexor-pronator’s Less common than lateral epicondylitis Clinical Symptoms Medial elbow pain Physical Examination Pain with palpation over medial condyle Pain with flexion and pronation of wrist against resistance Rule out ulnar neuropathy Treatment Same as lateral epicondylitis CLAVICLE FRACTURE Most common bone injury -

OUTPATIENT REHABILITATION for a PATIENT FOLLOWING a SURGICALLY STABILIZED TRIMALLEOLAR FRACTURE a Doctoral Project a Comprehensi
OUTPATIENT REHABILITATION FOR A PATIENT FOLLOWING A SURGICALLY STABILIZED TRIMALLEOLAR FRACTURE A Doctoral Project A Comprehensive Case Analysis Presented to the faculty of the Department of Physical Therapy California State University, Sacramento Submitted in partial satisfaction of the requirements for the degree of DOCTOR OF PHYSICAL THERAPY by Julie Hammond FALL 2017 © 2017 Julie Hammond ALL RIGHTS RESERVED ii OUTPATIENT REHABILITATION FOR A PATIENT FOLLOWING A SURGICALLY STABILIZED TRIMALLEOLAR FRACTURE A Doctoral Project by Julie Hammond Approved by: _____________________________________, Committee Chair Edward Barakatt, PT, PhD _____________________________________, First Reader William Garcia, PT, DPT, OCS, FAAOMPT _____________________________________, Second Reader Rafael Escamilla, PhD, PT, CSCS ____________________________ Date iii Student: Julie Hammond I certify that this student has met the requirements for format contained in the University format manual, and that this project is suitable for shelving in the Library and credit is to be awarded for the project. __________________________________, Department Chair ____________ Michael McKeough, PT, EdD Date Department of Physical Therapy iv Abstract of OUTPATIENT REHABILITATION FOR A PATIENT FOLLOWING A SURGICALLY STABILIZED TRIMALLEOLAR FRACTURE by Julie Hammond A 46 year old woman with a right surgically stabilized trimalleolar fracture was seen for physical therapy treatment for 13 sessions from 06/17/2016 to 09/16/2106 at an outpatient pro bono physical therapy clinic. Treatment was provided by a student physical therapist under the supervision of a licensed physical therapist. The patient was evaluated at the initial encounter with manual muscle test, goniometric measurements, single leg balance test, Timed Up and Go test, and a self- report questionnaire (Foot and Ankle Ability Measure). -
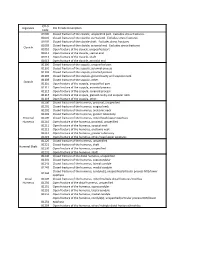
ICD*9, Diganosis ICD*9,Code,Description Code 81000 Closed,Fracture,Of,The,Clavicle,,Unspecified,Part.,,Excludes,Stress,Fractures
ICD*9, Diganosis ICD*9,Code,Description Code 81000 Closed,fracture,of,the,clavicle,,unspecified,part.,,Excludes,stress,fractures. 81001 Closed,fracture,of,the,clavicle,,sternal,end.,,Excludes,stress,fractures. 81002 Closed,fracture,of,the,clavicle,shaft.,,Excludes,stress,fractures. 81003 Closed,fracture,of,the,clavicle,,acromial,end.,,Excludes,stress,fractures. Clavicle 81010 Open,fracture,of,the,clavicle,,unspecified,part 81011 Open,fracture,of,the,clavicle,,sternal,end 81012 Open,fracture,of,the,clavicle,,shaft 81013 Open,fracture,of,the,clavicle,,acromial,end 81100 Closed,fracture,of,the,scapula,,unspecified,part 81101 Closed,fracture,of,the,scapula,,acromial,process 81102 Closed,fracture,of,the,scapula,,coracoid,process 81103 Closed,fracture,of,the,scapula,,glenoid,cavity,and,scapular,neck 81109 Closed,fracture,of,the,scapula,,other. Scapula 81110 Open,fracture,of,the,scapula,,unspecified,part 81111 Open,fracture,of,the,scapula,,acromial,process 81112 Open,fracture,of,the,scapula,,coracoid,process 81113 Open,fracture,of,the,scapula,,glenoid,cavity,and,scapular,neck 81119 Open,fracture,of,the,scapula,,other. 81200 Closed,fracture,of,the,humerus,,proximal,,unspecified 81201 Closed,fracture,of,the,humerus,,surgical,neck 81202 Closed,fracture,of,the,humerus,,anatomic,neck 81203 Closed,fracture,of,the,humerus,,greater,tuberosity Proximal, 81209 Closed,fracture,of,the,humerus,,other/head/upper,epiphysis Humerus 81210 Open,fracture,of,the,humerus,,proximal,,unspecified 81211 Open,fracture,of,the,humerus,,surgical,neck 81212 Open,fracture,of,the,humerus,,anatomic,neck -

Risk Factors for Fracture and Fracture Severity of the Distal Radius and Ankle. What About Osteoporosis, Celiac Disease and Obesity?
Risk factors for fracture and fracture severity of the distal radius and ankle. What about osteoporosis, celiac disease and obesity? Anja Myhre Hjelle Thesis for the degree of Philosophiae Doctor (PhD) University of Bergen, Norway 2021 Risk factors for fracture and fracture severity of the distal radius and ankle. What about osteoporosis, celiac disease and obesity? Anja Myhre Hjelle ThesisAvhandling for the for degree graden of philosophiaePhilosophiae doctorDoctor (ph.d (PhD). ) atved the Universitetet University of i BergenBergen Date of defense:2017 17.06.2021 Dato for disputas: 1111 © Copyright Anja Myhre Hjelle The material in this publication is covered by the provisions of the Copyright Act. Year: 2021 Title: Risk factors for fracture and fracture severity of the distal radius and ankle. Name: Anja Myhre Hjelle Print: Skipnes Kommunikasjon / University of Bergen 1 CONTRIBUTORS This work is the result of a collaboration between and funding from The Department of Global Public Health and Primary Care at the University of Bergen, The Department of Rheumatology at the District Hospital of Førde, and The Centre for Health Research in Sogn og Fjordane (a collaborative effort between Førde Health Trust and the health studies department of the Western Norway University College of Applied Sciences). We have also collaborated with The Department of Orthopedic surgery and the Department of Radiology at the District Hospital of Førde, The Departement of Rheumatology at Haukeland University Hospital, Bergen, and The KB Jebsen Coeliac Disease Research Centre, University of Oslo. We are grateful for additional funding received from The Norwegian association for Celiac Disease (Norsk Cøliakiforening) in 2012 and 2015. -
Radial Head Fracture Repair and Rehabilitation
1 Radial Head Fracture Repair and Rehabilitation Surgical Indications and Considerations Anatomical Considerations: The elbow is a complex joint due to its intricate functional anatomy. The ulna, radius and humerus articulate in such a way as to form four distinctive joints. Surrounding the osseous structures are the ulnar collateral ligament complex, the lateral collateral ligament complex and the joint capsule. Four main muscle groups provide movement: the elbow flexors, the elbow extensors, the flexor-pronator group, and the extensor-supinator groups. Different types of radial head fractures can occur each of which has separate surgical indications and considerations. Fractures of the proximal one-third of the radius normally occur in the head region in adults and in neck region in children. The most recognized and used standard for assessing radial head fractures is the 4-part Mason classification system. It is used for both treatment and prognosis. Classification: Type I fracture A fissure or marginal fracture without displacement. Type II fracture Marginal fractures with displacement involving greater than 2 mm displacement. Type III fracture Comminuted fractures of the whole radial head. Type IV fracture (variation) A comminuted fracture, with an associated dislocation, ligament injury, coronoid fracture, or Monteggia lesion. Pathogenesis: Severe comminuted fractures or fracture dislocations of the head of the radius often occur as the result of a fall on an outstretched arm with the distal forearm angled laterally, or a valgus stress on the elbow. Fractures can also occur from a direct blow or force to the elbow (e.g. MVA). Chronic synovitis and mild deterioration of the articular surfaces associated with arthritis (e.g. -

Moda Health Plan, Inc. Medical Necessity Criteria
Moda Health Plan, Inc. Subject: Bone Growth Stimulators- Medical Necessity Criteria Ultrasound Page 1 of 8 Origination Date: 01/07 Revision Date(s): 1/08, 1/09, 2/11, 1/12, 09/12, 07/13, 06/14, 09/14, 05/15, 07/15 Developed By: Medical Criteria Committee 01/07 Approved: Mary Engrav, MD Date: 05/27/2015 Description: Bone growth stimulation is a technique of promoting bone growth in difficult to heal fractures. Two types of bone growth stimulators currently exist: electrical and ultrasonic. Ultrasonic fracture healing is a noninvasive treatment that utilizes low intensity, pulsed ultrasound delivered through a skin surface transducer placed directly over the fracture site. It is used to accelerate healing of fresh fractures and fracture nonunions of sites that are difficult to heal because of poor vascular supply. It is frequently used in conjunction with orthopedic treatments such as a cast or splint. The device is portable and can be used by the patient at home in daily 20 minute sessions. The Sonic Accelerated Fracture Healing System (SAFHS) is a type of ultrasound bone growth stimulator. Criteria: I. Ultrasonic Bone Growth Stimulators (CWQI HCS-0008A) A. Ultrasonic bone growth stimulators will be covered to plan limitations for skeletally mature individuals when 1 or more of the following criteria are met: 1. Fresh Acute Fractures a. Most fresh fractures heal with the use of standard fracture care such as closed reduction and cast immobilization. Ultrasonic bone growth stimulators may be indicated for the treatment of fresh fractures when 1 (one) or more of the following risk factors for delayed fracture healing or nonunion are present: i. -

Radiographic Evaluation, Fixation Principles, and Post-Operative Management of Ankle Fractures
Central JSM Foot and Ankle Bringing Excellence in Open Access Review Article *Corresponding author Lisa Zhang, Department of Podiatry, University Hospital, G142. 150 Bergen St. Newark, NJ 07103, USA, Tel: 908- Radiographic Evaluation, 577-2543; Email: Submitted: 15 March 2018 Fixation Principles, and Post- Accepted: 23 June 2017 Published: 25 June 2017 ISSN: 2475-9112 Operative Management of Copyright © 2017 Zhang et al. Ankle Fractures OPEN ACCESS 1 2 Lisa Zhang * and Ritchard Rosen Keywords 1Department of Podiatry, University Hospital, Newark, USA • Fracture blisters 2Department of Podiatric Surgery, Holy Name Medical Center, USA • Neutralization plate • Posterior-antiglide plate • Tension banding Abstract • Direct approach Radiographically, ankle fractures can be evaluated on the anterior-posterior (AP) view • Early weight bearing with the talocrural angle, and on the mortise view, by Shenton’sline, the dime sign, and talar tilt. Displaced fractures > 2 mm, lateral malleolar fractures that are shortened, rotated, or angulated, and bimalleolar and trimalleolar fractures require fixation. Principles of fixation include a proper soft tissue envelope without fracture blisters present at incision sites. Due to the formation of soft callus, fractures should be fixated within the first two weeks of injury. The lateral malleolus is the dominant fracture, and must be pulled out to length, which will pull other ligamentous attachments to proper alignment. Lateral malleolar fixation may be accomplished by a neutralization plate or posterior anti-glide plate; a locking plate may also be used in osteoporotic bone. Medial malleolar fixation can be accomplished by two screw cancellous fixation or tension banding, the latter especially useful in smaller, comminuted fractures.