Common Skin Diseases
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Seborrheic Dermatitis: an Overview ROBERT A
Seborrheic Dermatitis: An Overview ROBERT A. SCHWARTZ, M.D., M.P.H., CHRISTOPHER A. JANUSZ, M.D., and CAMILA K. JANNIGER, M.D. University of Medicine and Dentistry at New Jersey-New Jersey Medical School, Newark, New Jersey Seborrheic dermatitis affects the scalp, central face, and anterior chest. In adolescents and adults, it often presents as scalp scaling (dandruff). Seborrheic dermatitis also may cause mild to marked erythema of the nasolabial fold, often with scaling. Stress can cause flare-ups. The scales are greasy, not dry, as commonly thought. An uncommon generalized form in infants may be linked to immunodeficiencies. Topical therapy primarily consists of antifungal agents and low-potency steroids. New topical calcineurin inhibitors (immunomodulators) sometimes are administered. (Am Fam Physician 2006;74:125-30. Copyright © 2006 American Academy of Family Physicians.) eborrheic dermatitis can affect patients levels, fungal infections, nutritional deficits, from infancy to old age.1-3 The con- neurogenic factors) are associated with the dition most commonly occurs in condition. The possible hormonal link may infants within the first three months explain why the condition appears in infancy, S of life and in adults at 30 to 60 years of age. In disappears spontaneously, then reappears adolescents and adults, it usually presents as more prominently after puberty. A more scalp scaling (dandruff) or as mild to marked causal link seems to exist between seborrheic erythema of the nasolabial fold during times dermatitis and the proliferation of Malassezia of stress or sleep deprivation. The latter type species (e.g., Malassezia furfur, Malassezia tends to affect men more often than women ovalis) found in normal dimorphic human and often is precipitated by emotional stress. -

Scalp Eczema Factsheet the Scalp Is an Area of the Body That Can Be Affected by Several Types of Eczema
12 Scalp eczema factsheet The scalp is an area of the body that can be affected by several types of eczema. The scalp may be dry, itchy and scaly in a chronic phase and inflamed (red), weepy and painful in an acute (eczema flare) phase. Aside from eczema, there are a number of reasons why the scalp can become dry and itchy (e.g. psoriasis, fungal infection, ringworm, head lice etc.), so it is wise to get a firm diagnosis if there is uncertainty. Types of eczema • Hair clips and headgear – especially those containing that affect the scalp rubber or nickel. Seborrhoeic eczema (dermatitis) is one of the most See the NES booklet on Contact Dermatitis for more common types of eczema seen on the scalp and hairline. details. It can affect babies (cradle cap), children and adults. The Irritant contact dermatitis is a type of eczema that skin appears red and scaly and there is often dandruff as occurs when the skin’s surface is irritated by a substance well, which can vary in severity. There may also be a rash that causes the skin to become dry, red and itchy. on other parts of the face, such as around the eyebrows, For example, shampoos, mousses, hair gels, hair spray, eyelids and sides of the nose. Seborrhoeic eczema can perm solution and fragrance can all cause irritant contact become infected. See the NES factsheets on Adult dermatitis. See the NES booklet on Contact Dermatitis for Seborrhoeic Dermatitis and Infantile Seborrhoeic more details. Dermatitis and Cradle Cap for more details. -

Clinical Study of Nail Changes in Papulosquamous Disorders
Original Research Article Clinical study of Nail changes in papulosquamous disorders Vishal Wali1, Trivedi Rahul Prasad2* 1Associate Professor, 2Post Graduate, Department of Dermatology, Venereology and Leprology, Mahadevappa Rampure Medical College, Sedam Road, Kalaburagi (Gulbarga) 585105, Karnataka, INDIA. Email: [email protected] Abstract Background: Nail disorders comprise ~10% of all dermatologic conditions. Nail disorders include those abnormalities that effect any portion of the nail unit. The nail unit includes the plate, matrix, bed, proximal and lateral folds, hyponychium, and some definitions include the underlying distal phalanx. These structures may be effected by heredity, skin disorders, infections, systemic disease, and aging process, internal and external medications, physical and environmental agents, trauma, and tumours, both benign and malignant. The main contributors being papulosquamous disorder. Nail changes in papulosquamous disorder have been inadequately discussed and only limited studies are present. This study aims to throw some light about frequency of nail involvement in papulosquamous disorders and its various patterns. Methodology: This is the descriptive study. It was conducted in department of DVL of Mahadevappa Rampura Medical college and Basaveshwar teaching and general hospital, Kalaburagi from July 2019 to Feb 2021. General, systemic and dermatological examinations were done. Nails were examined in detail. Special investigations like skin biopsy and potassium hydroxide (KOH) mount was done in relevant cases. Results: There were 50 cases of papulosquamous disorder. The most common papulosquamous disorder was psoriasis, followed by lichen planus and PRP. Out of these the most common nail change was pitting (81%) and lest common was dorsal pterygium (%) Conclusion: Nail being an important appendage affecting various dermatosis and acts as window in diagnosis. -

Skin Conditions and Related Need for Medical Care Among Persons 1=74 Years United States, 1971-1974
Data from the Series 11 NATIONAL HEALTH SURVEY Number 212 Skin Conditions and Related Need for Medical Care Among Persons 1=74 Years United States, 1971-1974 DHEW Publication No. (PHS) 79-1660 U.S, DEPARTMENT OF HEALTH, EDUCATION, AND WELFARE Public Health Service Office of the Assistant Secretary for Health National Center for Health Statistics Hyattsville, Md. November 1978 NATIONAL CENTIER FOR HEALTH STATISTICS DOROTHY P. RICE, Director ROBERT A. ISRAEL, Deputy Director JACOB J. FELDAMN, Ph.D., Associate Director for Amdy.sis GAIL F. FISHER, Ph.D., Associate Director for the Cooperative Health Statistics System ELIJAH L. WHITE, Associate Director for Data Systems JAMES T. BAIRD, JR., Ph.D., Associate Director for International Statistics ROBERT C. HUBER, Associate Director for Managewzent MONROE G. SIRKEN, Ph.D., Associate Director for Mathematical Statistics PETER L. HURLEY, Associate Director for Operations JAMES M. ROBEY, Ph.D., Associate Director for Program Development PAUL E. LEAVERTON, Ph.D., Associate Director for Research ALICE HAYWOOD,, Information Officer DIVISION OF HEALTH EXAMINATION STATISTICS MICHAEL A. W. HATTWICK, M.D., Director JEAN ROEERTS, Chiej, Medical Statistics Branch ROBERT S. MURPHY, Chiej Survey Planning and Development Branch DIVISION OF OPERATIONS HENRY MILLER, ChieJ Health -Examination Field Operations Branch COOPERATION OF THE U.S. BUREAU OF THE CENSUS Under the legislation establishing the National Health Survey, the Public Health Service is authorized to use, insofar as possible, the sesw?icesor facilities of other Federal, State, or private agencies. In accordance with specifications established by the National Center for Health Statis- tics, the U.S. Bureau of the Census participated in the design and selection of the sample and carried out the household interview stage of :the data collection and certain parts of the statis- tical processing. -

An Ayurvedic Approach in the Management of Darunaka (Seborrhoeic Dermatitis): a Case Study
International Journal of Health Sciences and Research Vol.10; Issue: 4; April 2020 Website: www.ijhsr.org Case Study ISSN: 2249-9571 An Ayurvedic Approach in the Management of Darunaka (Seborrhoeic Dermatitis): A Case Study Kumari Archana1, D.B. Vaghela2 1PhD Scholar, 2Assosiate Professor, Shalakyatantra Department, Institute for Post Graduate Teaching and Research in Ayurveda, Gujarat Ayurved University, Jamnagar, India. Corresponding Author: Kumari Archana ABSTRACT Darunaka is a Kapalagataroga but Acharya Sushruta has described this disease as a Kshudraroga due to the vitiation of Vata and Kapha Doshas with symptoms like Kandu (itching on scalp), Keshachyuti (falling of hair), Swapa(abnormalities of touch sensation on scalp), Rookshata (roughness or dryness of the scalp) and Twaksphutana (breaking or cracking of the scalp skin). Seborrhoeic Dermatitis, an irritative disease of the scalp in which shedding of dead tissue from the scalp with itching sensation is the cardinal feature which can be correlated with Darunaka. It has been reported that Seborrhoeic Dermatitisaffect about 4% of the population, and dandruff (which is mild seborrhoeic dermatitis of the scalp) can affect almost half of all adults. It can start at any time after puberty and is slightly commoner in men. It can result in social or self-esteem problems. A 56 yr old male patient from Jamnagar came to OPD of ShalakyaTantra, with chief complaint of ShirahKandu (itching on scalp), Rukshata (dryness on scalp), TwakSphutana (cracks in the skin) with blood mixed watery oozing, KeshaChyuti (hair fall). In this case Ayurvedic formulation of ArogyavardhiniVati (orally), TriphalaChurna (orally), ManjisthadiKwatha (orally), YashtiChurna mixed with coconut hair oil as external application followed by washing the hair with a Kwatha (decoction) of TriphalaYavkut and ShuddhaTankana. -

Therapies for Common Cutaneous Fungal Infections
MedicineToday 2014; 15(6): 35-47 PEER REVIEWED FEATURE 2 CPD POINTS Therapies for common cutaneous fungal infections KENG-EE THAI MB BS(Hons), BMedSci(Hons), FACD Key points A practical approach to the diagnosis and treatment of common fungal • Fungal infection should infections of the skin and hair is provided. Topical antifungal therapies always be in the differential are effective and usually used as first-line therapy, with oral antifungals diagnosis of any scaly rash. being saved for recalcitrant infections. Treatment should be for several • Topical antifungal agents are typically adequate treatment weeks at least. for simple tinea. • Oral antifungal therapy may inea and yeast infections are among the dermatophytoses (tinea) and yeast infections be required for extensive most common diagnoses found in general and their differential diagnoses and treatments disease, fungal folliculitis and practice and dermatology. Although are then discussed (Table). tinea involving the face, hair- antifungal therapies are effective in these bearing areas, palms and T infections, an accurate diagnosis is required to ANTIFUNGAL THERAPIES soles. avoid misuse of these or other topical agents. Topical antifungal preparations are the most • Tinea should be suspected if Furthermore, subsequent active prevention is commonly prescribed agents for dermatomy- there is unilateral hand just as important as the initial treatment of the coses, with systemic agents being used for dermatitis and rash on both fungal infection. complex, widespread tinea or when topical agents feet – ‘one hand and two feet’ This article provides a practical approach fail for tinea or yeast infections. The pharmacol- involvement. to antifungal therapy for common fungal infec- ogy of the systemic agents is discussed first here. -

Natural Remedies for Dandruff
Natural Remedies for Dandruff Before you consider treating dandruff, you must first understand what it is, so that you can be sure you are suffering from dandruff and not a more serious condition. Dandruff is small pieces of dead skin found in a person’s hair. Dandruff can be mild and hardly noticeable, but in some cases can be itchy and the scalp can be red and inflamed. Dandruff can be a chronic condition or related to certain variables such as extreme temperatures and weather changes. If your dandruff is severe, the best option is to be seen by your dermatologist. If, however, it is mild there are several natural remedies that are thought to help improve dandruff. 1. Apple Cider Vinegar Possibly one of the best natural remedies for dandruff, rinsing your scalp with a half water half apple cider vinegar mixture can help decrease flakiness. Apple Cider Vinegar will remove dead skin cells and unclog pores. It also has strong anti-fungal properties, which can help fight off any dandruff caused by fungus on the scalp. Rinse your scalp with the mixture and leave it overnight. Wash your hair the next day with a gentle shampoo. 2. Chamomile Tea Chamomile is very soothing and safe for sensitive skin. It can help with redness and irritation. Brew three sachets of chamomile tea and be sure to allow ample time for the tea to cool. Once the tea has cooled to about room temperature, apply the liquid to the scalp and massage. Allow this to sit for several hours and then rinse thoroughly. -

PE2342 Seborrheic Dermatitis
Seborrheic Dermatitis What is seborrheic Seborrheic dermatitis is a common skin condition. It causes redness, dermatitis? scaling, or flaky patches in infants, teens and adults. What parts of the • Scalp (this is known as dandruff, or cradle cap in infants) body are usually • Eyebrows affected? • Eyelids • Ears • Nose • Skin fold areas (such as armpits or thighs) What causes The cause of seborrheic dermatitis is not known. Some believe that it is seborrheic caused by an overgrowth of yeast. It is not related to what you eat and it is dermatitis? not contagious. Stress and sickness often make seborrheic dermatitis symptoms worse, but they do not cause it. Symptoms can get better or worse for no reason. What are the Symptoms include: symptoms of • Redness seborrheic • Itching dermatitis? • Scaly patches on your skin that may look greasy or oily • Scales or flakes on the head or in the hair • Crusty yellow flakes on the eyelids or eyelashes What are the There is no cure for seborrheic dermatitis, but there are ways to keep it treatment options? under control. Treatment options for seborrheic dermatitis depend on what part of the body is showing symptoms. Skin Seborrheic dermatitis of the skin can usually be controlled by putting on steroid or antifungal creams to the skin (topical). These medicines help with the redness and itching of your child’s skin. Check with your child’s healthcare provider before giving your child any type of topical medicine. They will help you determine which treatment option would be best. 1 of 2 To Learn More Free Interpreter Services • Dermatology • In the hospital, ask your nurse. -
Healthy Hair Healthy Scalp
Healthy hair starts with a healthy scalp Understanding and treating common scalp problems #1 dermatologist recommended therapeutic shampoo brand Recognizing common scalp conditions The largest organ of the human body is the skin. Like any DANDRUFF organ or other part of the body, the skin is constantly healing Symptoms typically include itching, and rebuilding itself by creating new cells and shedding flaking, and dryness of the scalp. old ones. The same regenerative process happens on the scalp when skin cells complete their life cycle, then flake off. This kind of flaking is healthy and usually unnoticeable. Sometimes, people experience increased levels of scalp dryness and flaking. This can result from temporary changes like cold weather, washing hair too often or not often enough, or even stress. SCALP PSORIASIS Dandruff, on the other hand, is a chronic condition Symptoms include inflammation recognized by persistent flaking, itching, and irritation of and the build-up of powdery, large, the scalp. Dandruff has many causes including dry skin, silvery plaques on the skin’s surface, infrequent shampooing, sensitivity to hair care products, a especially on the knees, elbows, and yeast-like fungus, or a skin condition that causes a disruption scalp. The severity of scalp psoriasis can vary from thin and loose, to thick in the rhythm of skin renewal on the scalp that can result in and crusted plaques. too many cells shedding too quickly. While dandruff is responsible for most itchy, flaky scalp symptoms, two less common conditions also cause SEBORRHEIC DERMATITIS persistent flaking and scalp irritation: scalp psoriasis and Symptoms include reddened, irritated seborrheic dermatitis. -

How to Treat Dandruff
HOW TO TREAT DANDRUFF Dandruff is a common scalp condition in which small pieces of dry skin flake off of the scalp. The most effective way to treat and control dandruff is to use dandruff shampoo and scalp treatments. Follow these tips from dermatologists to get the best results. Dandruff is a common scalp condition in which small pieces of dry skin flake off of the scalp. If you have dark hair or you’re wearing dark colors, you may notice the flakes in your hair or on your shoulders. Dandruff may also make your scalp itch. Many people believe that dandruff is caused by poor hygiene, but this is not true. Although infrequent shampooing can make dandruff more obvious, researchers are still studying the causes, which appear to be complex. The most effective way to treat and control dandruff is to use dandruff shampoo and scalp treatments. Follow these tips from dermatologists to get the best results: 1. Follow the instructions on the dandruff shampoo bottle. There are many different dandruff shampoos, and each contains different active ingredients for controlling symptoms. To get the best results, always follow the instructions on the bottle. For example, some dandruff shampoos require that you lather the shampoo into the hair and scalp and leave the shampoo in for about five minutes before rinsing. Others should not be left on the scalp. 2. If you are Caucasian or Asian, shampoo daily and use dandruff shampoo twice a week. If using one dandruff shampoo does not bring relief, try alternating between dandruff shampoos with different active ingredients. -
Adolescent with Rash on Face and Scalp
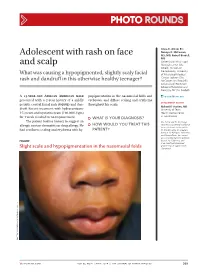
Photo RoUNDS Anna K. Allred, BS; Nancye K. McCowan, Adolescent with rash on face MS, MD; Robert Brodell, MD University of Mississippi and scalp Medical Center (Ms. Allred); Division of Dermatology, University What was causing a hypopigmented, slightly scaly facial of Mississippi Medical Center, Jackson (Drs. rash and dandruff in this otherwise healthy teenager? McCowan and Brodell); University of Rochester School of Medicine and Dentistry, NY (Dr. Brodell) A 13-year-old African American male popigmentation in the nasomesial folds and [email protected] presented with a 2-year history of a mildly eyebrows, and diffuse scaling and erythema DEpartment EDItOR pruritic central facial rash (FIGURE) and dan- throughout his scalp. Richard p. Usatine, MD druff. Recent treatment with hydrocortisone University of Texas 1% cream and nystatin cream (100,000 U/gm) Health Science Center at San Antonio for 1 week resulted in no improvement. ● What is youR diAgnosis? The patient had no history to suggest an Ms. Allred and Dr. McCowan allergic contact dermatitis or drug allergy. He ● HoW Would you TReAT THIS reported no potential conflict of interest relevant to this article. had confluent scaling and erythema with hy- pATIENT? Dr. Brodell serves on speaker’s bureaus for Allergan, Galderma, and PharmaDerm, has served as a consultant and on advisory Figure boards for Galderma, and is an investigator/received grant/research support from Slight scale and hypopigmentation in the nasomesial folds Genentech. PHO T o COU RT ESY OF : R o B e RT BR ODELL , MD jfponline.com Vol 63, no 4 | ApRIL 2014 | The jouRnAl of Family PracTice 209 PHOTO RoUNDS Diagnosis: the Malassezia yeast and topical steroids are Seborrheic dermatitis used to suppress inflammation. -

Pediatric Psoriasis
Pediatric Papulosquamous and Eczematous Disorders St. John’s Episcopal Hospital Program Director- Dr. Suzanne Sirota-Rozenberg Dr. Brett Dolgin, DO Dr. Asma Ahmed, DO Dr. Anna Slobodskya, DO Dr. Stephanie Lasky, DO Dr. Louis Siegel, DO Dr. Evelyn Gordon, DO Dr. Vanita Chand, DO Pediatric Psoriasis Epidemiology • Psoriasis can first appear at any age, from infancy to the eighth decade of life • The prevalence of psoriasis in children ages 0 to 18 years old is 1% with an incidence of 40.8 per 100,000 ppl • ~ 75% have onset before 40 years of age What causes psoriasis? • Multifactorial • Genetics – HLA associations (Cw6, B13, B17, B57, B27, DR7) • Abnormal T cell activation – Th1, Th17 with increased cytokines IL 1, 2, 12, 17, 23, IFN-gamma, TNF-alpha • External triggers: – Injury (Koebner phenomenon) – medications (lithium, IFNs, β-blockers, antimalarials, rapid taper of systemic corticosteroids) – infections (particularly streptococcal tonsillitis). Pediatric Psoriasis Types: • Acute Guttate Psoriasis – Small erythematous plaques occurring after infection (MOST common in children) • 40% of patients with guttate psoriasis will progress to develop plaque type psoriasis • Chronic plaque Psoriasis – erythematous plaques with scaling • Flexural Psoriasis – Erythematous areas between skin folds • Scalp Psoriasis – Thick scale found on scalp • Nail Psoriasis – Nail dystrophy • Erythrodermic Psoriasis– Severe erythema covering all or most of the body • Pustular Psoriasis – Acutely arising pustules • Photosensitive Psoriasis – Seen in areas of sun