Addis Ababa University, College of Health Sciences, School of Public Health Ethiopian Field Epidemiology Training Program (EFETP)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

An Analysis of the Afar-Somali Conflict in Ethiopia and Djibouti
Regional Dynamics of Inter-ethnic Conflicts in the Horn of Africa: An Analysis of the Afar-Somali Conflict in Ethiopia and Djibouti DISSERTATION ZUR ERLANGUNG DER GRADES DES DOKTORS DER PHILOSOPHIE DER UNIVERSTÄT HAMBURG VORGELEGT VON YASIN MOHAMMED YASIN from Assab, Ethiopia HAMBURG 2010 ii Regional Dynamics of Inter-ethnic Conflicts in the Horn of Africa: An Analysis of the Afar-Somali Conflict in Ethiopia and Djibouti by Yasin Mohammed Yasin Submitted in partial fulfilment of the requirements for the degree PHILOSOPHIAE DOCTOR (POLITICAL SCIENCE) in the FACULITY OF BUSINESS, ECONOMICS AND SOCIAL SCIENCES at the UNIVERSITY OF HAMBURG Supervisors Prof. Dr. Cord Jakobeit Prof. Dr. Rainer Tetzlaff HAMBURG 15 December 2010 iii Acknowledgments First and foremost, I would like to thank my doctoral fathers Prof. Dr. Cord Jakobeit and Prof. Dr. Rainer Tetzlaff for their critical comments and kindly encouragement that made it possible for me to complete this PhD project. Particularly, Prof. Jakobeit’s invaluable assistance whenever I needed and his academic follow-up enabled me to carry out the work successfully. I therefore ask Prof. Dr. Cord Jakobeit to accept my sincere thanks. I am also grateful to Prof. Dr. Klaus Mummenhoff and the association, Verein zur Förderung äthiopischer Schüler und Studenten e. V., Osnabruck , for the enthusiastic morale and financial support offered to me in my stay in Hamburg as well as during routine travels between Addis and Hamburg. I also owe much to Dr. Wolbert Smidt for his friendly and academic guidance throughout the research and writing of this dissertation. Special thanks are reserved to the Department of Social Sciences at the University of Hamburg and the German Institute for Global and Area Studies (GIGA) that provided me comfortable environment during my research work in Hamburg. -

Districts of Ethiopia
Region District or Woredas Zone Remarks Afar Region Argobba Special Woreda -- Independent district/woredas Afar Region Afambo Zone 1 (Awsi Rasu) Afar Region Asayita Zone 1 (Awsi Rasu) Afar Region Chifra Zone 1 (Awsi Rasu) Afar Region Dubti Zone 1 (Awsi Rasu) Afar Region Elidar Zone 1 (Awsi Rasu) Afar Region Kori Zone 1 (Awsi Rasu) Afar Region Mille Zone 1 (Awsi Rasu) Afar Region Abala Zone 2 (Kilbet Rasu) Afar Region Afdera Zone 2 (Kilbet Rasu) Afar Region Berhale Zone 2 (Kilbet Rasu) Afar Region Dallol Zone 2 (Kilbet Rasu) Afar Region Erebti Zone 2 (Kilbet Rasu) Afar Region Koneba Zone 2 (Kilbet Rasu) Afar Region Megale Zone 2 (Kilbet Rasu) Afar Region Amibara Zone 3 (Gabi Rasu) Afar Region Awash Fentale Zone 3 (Gabi Rasu) Afar Region Bure Mudaytu Zone 3 (Gabi Rasu) Afar Region Dulecha Zone 3 (Gabi Rasu) Afar Region Gewane Zone 3 (Gabi Rasu) Afar Region Aura Zone 4 (Fantena Rasu) Afar Region Ewa Zone 4 (Fantena Rasu) Afar Region Gulina Zone 4 (Fantena Rasu) Afar Region Teru Zone 4 (Fantena Rasu) Afar Region Yalo Zone 4 (Fantena Rasu) Afar Region Dalifage (formerly known as Artuma) Zone 5 (Hari Rasu) Afar Region Dewe Zone 5 (Hari Rasu) Afar Region Hadele Ele (formerly known as Fursi) Zone 5 (Hari Rasu) Afar Region Simurobi Gele'alo Zone 5 (Hari Rasu) Afar Region Telalak Zone 5 (Hari Rasu) Amhara Region Achefer -- Defunct district/woredas Amhara Region Angolalla Terana Asagirt -- Defunct district/woredas Amhara Region Artuma Fursina Jile -- Defunct district/woredas Amhara Region Banja -- Defunct district/woredas Amhara Region Belessa -- -

On Farm Performance Evaluation of Three Local Chicken Ecotypes in Western Zone of Tigray, Northern Ethiopia
Journal of Biology, Agriculture and Healthcare www.iiste.org ISSN 2224-3208 (Paper) ISSN 2225-093X (Online) Vol.5, No.7, 2015 On Farm Performance Evaluation of Three Local Chicken Ecotypes in Western Zone of Tigray, Northern Ethiopia Shishay Markos 1* Berhanu Belay 2 Tadelle Dessie 3 1.Humera Agricultural Research Center of Tigray Agricultural Research Institute, P.O.BOX 492, Mekelle, Tigray, Ethiopia 2.Jimma University College of Agriculture and Veterinary Medicine, P.O.Box 307, Jimma, Ethiopia 3.International Livestock Research Institute (ILRI), P.O.BOX, 5689, Addis Ababa, Ethiopia Corresponding Author: [email protected] Abstract The study aimed to assess performances of three local chicken ecotypes under free scavenging production system in western Tigray. Multi stage sampling procedure was applied for the study, hence three rural weredas, nine kebeles and 385 respondents were selected by purposive, stratified purposive and purposive random sampli ng techniques, respectively. Pretested questionnaire was employed to generate data. Household characteristics w ere analyzed using descriptive statistics and Kruskal Wall’s of SPSS 16 was employed to test qualitative variable proportion difference across agroecologies. Performance traits were analyzed by GLM Procedures of SAS 9.2. Tukey test was used to compare means for significant traits. Significant differences were observed among chicken ecotypes in almost all studied performance traits. Lowland chicken ecotypes earlier to mature sexually, slaughter and onset egg laying in comparison to the other two ecotypes but yielded lower hatchability and egg yield. The overall mean age of sexual maturity of local chicken was 7.19±0.04 and 5.71±0.03 month for female and male respectively. -
20210714 Access Snapshot- Tigray Region June 2021 V2
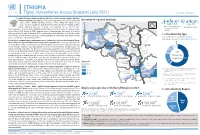
ETHIOPIA Tigray: Humanitarian Access Snapshot (July 2021) As of 31 July 2021 The conflict in Tigray continues despite the unilateral ceasefire announced by the Ethiopian Federal Government on 28 June, which resulted in the withdrawal of the Ethiopian National Overview of reported incidents July Since Nov July Since Nov Defense Forces (ENDF) and Eritrea’s Defense Forces (ErDF) from Tigray. In July, Tigray forces (TF) engaged in a military offensive in boundary areas of Amhara and Afar ERITREA 13 153 2 14 regions, displacing thousands of people and impacting access into the area. #Incidents impacting Aid workers killed Federal authorities announced the mobilization of armed forces from other regions. The Amhara region the security of aid Tahtay North workers Special Forces (ASF), backed by ENDF, maintain control of Western zone, with reports of a military Adiyabo Setit Humera Western build-up on both sides of the Tekezi river. ErDF are reportedly positioned in border areas of Eritrea and in SUDAN Kafta Humera Indasilassie % of incidents by type some kebeles in North-Western and Eastern zones. Thousands of people have been displaced from town Central Eastern these areas into Shire city, North-Western zone. In line with the Access Monitoring and Western Korarit https://bit.ly/3vcab7e May Reporting Framework: Electricity, telecommunications, and banking services continue to be disconnected throughout Tigray, Gaba Wukro Welkait TIGRAY 2% while commercial cargo and flights into the region remain suspended. This is having a major impact on Tselemti Abi Adi town May Tsebri relief operations. Partners are having to scale down operations and reduce movements due to the lack Dansha town town Mekelle AFAR 4% of fuel. -

Starving Tigray
Starving Tigray How Armed Conflict and Mass Atrocities Have Destroyed an Ethiopian Region’s Economy and Food System and Are Threatening Famine Foreword by Helen Clark April 6, 2021 ABOUT The World Peace Foundation, an operating foundation affiliated solely with the Fletcher School at Tufts University, aims to provide intellectual leadership on issues of peace, justice and security. We believe that innovative research and teaching are critical to the challenges of making peace around the world, and should go hand-in- hand with advocacy and practical engagement with the toughest issues. To respond to organized violence today, we not only need new instruments and tools—we need a new vision of peace. Our challenge is to reinvent peace. This report has benefited from the research, analysis and review of a number of individuals, most of whom preferred to remain anonymous. For that reason, we are attributing authorship solely to the World Peace Foundation. World Peace Foundation at the Fletcher School Tufts University 169 Holland Street, Suite 209 Somerville, MA 02144 ph: (617) 627-2255 worldpeacefoundation.org © 2021 by the World Peace Foundation. All rights reserved. Cover photo: A Tigrayan child at the refugee registration center near Kassala, Sudan Starving Tigray | I FOREWORD The calamitous humanitarian dimensions of the conflict in Tigray are becoming painfully clear. The international community must respond quickly and effectively now to save many hundreds of thou- sands of lives. The human tragedy which has unfolded in Tigray is a man-made disaster. Reports of mass atrocities there are heart breaking, as are those of starvation crimes. -

20Th International Conference of Ethiopian Studies ፳ኛ የኢትዮጵያ ጥናት ጉባኤ
20th International Conference of Ethiopian Studies ኛ ፳ የኢትዮጵያ ጥናት ጉባኤ Regional and Global Ethiopia – Interconnections and Identities 30 Sep. – 5 Oct. 2018 Mekelle University, Ethiopia Message by Prof. Dr. Fetien Abay, VPRCS, Mekelle University Mekelle University is proud to host the International Conference of Ethiopian Studies (ICES20), the most prestigious conference in social sciences and humanities related to the region. It is the first time that one of the younger universities of Ethiopia has got the opportunity to organize the conference by itself – following the great example set by the French team of the French Centre of Ethiopian Studies in Addis Abeba organizing the ICES in cooperation with Dire Dawa University in 2012, already then with great participation by Mekelle University academics and other younger universities of Ethiopia. We are grateful that we could accept the challenge, based on the set standards, in the new framework of very dynamic academic developments in Ethiopia. The international scene is also diversifying, not only the Ethiopian one, and this conference is a sign for it: As its theme says, Ethiopia is seen in its plural regional and global interconnections. In this sense it becomes even more international than before, as we see now the first time a strong participation from almost all neighboring countries, and other non-Western states, which will certainly contribute to new insights, add new perspectives and enrich the dialogue in international academia. The conference is also international in a new sense, as many academics working in one country are increasingly often nationals of other countries, as more and more academic life and progress anywhere lives from interconnections. -

Risk Factors and Spatio-Temporal Patterns of Human Rabies Exposure in Northwestern Tigray, Ethiopia
Gebru G, et al. Risk Factors and Spatio-Temporal Patterns of Human Rabies Exposure in Northwestern Tigray, Ethiopia. Annals of Global Health. 2019; 85(1): 119, 1–12. DOI: https://doi.org/10.5334/aogh.2518 ORIGINAL RESEARCH Risk Factors and Spatio-Temporal Patterns of Human Rabies Exposure in Northwestern Tigray, Ethiopia Gebreyohans Gebru*, Gebremedhin Romha†, Abrha Asefa‡, Haftom Hadush§ and Muluberhan Biedemariam‖ Background: Rabies is a neglected tropical disease, which is economically important with great public health concerns in developing countries including Ethiopia. Epidemiological information can play an important role in the control and prevention of rabies, though little is known about the status of the disease in many settings of Ethiopia. The present study aimed to investigate the risk factors and spatio-temporal patterns of human rabies exposure in Northwestern Tigray, Ethiopia. Methods: A prospective study was conducted from 01 January 2016 to 31 December 2016 (lapsed for one year) at Suhul general hospital, Northern Ethiopia. Data of human rabies exposure cases were collected using a pretested questionnaire that was prepared for individuals dog bite victims. Moreover, GPS coordinate of each exposure site was collected for spatio-temporal analysis using hand-held Garmin 64 GPS apparatus. Later, cluster of human rabies exposures were identified using Getis-Ord *Gi statistics. Results: In total, 368 human rabies exposure cases were collected during the study year. Age group of 5 to 14 years old were highly exposed (43.2%; 95% CI, 38.2–48.3). Greater number of human rabies exposures was registered in males (63%; 95% CI, 58.0–67.8) than females (37%; 95% CI, 32.1–42.0). -

Regreening of the Northern Ethiopian Mountains: Effects on Flooding and on Water Balance
PATRICK VAN DAMME THE ROLE OF TREE DOMESTICATION IN GREEN MARKET PRODUCT VALUE CHAIN DEVELOPMENT IN AFRICA afrika focus — Volume 31, Nr. 2, 2018 — pp. 129-147 REGREENING OF THE NORTHERN ETHIOPIAN MOUNTAINS: EFFECTS ON FLOODING AND ON WATER BALANCE Tesfaalem G. Asfaha (1,2), Michiel De Meyere (2), Amaury Frankl (2), Mitiku Haile (3), Jan Nyssen (2) (1) Department of Geography and Environmental Studies, Mekelle University, Ethiopia (2) Department of Geography, Ghent University, Belgium (3) Department of Land Resources Management and Environmental Protection, Mekelle University, Ethiopia The hydro-geomorphology of mountain catchments is mainly determined by vegetation cover. This study was carried out to analyse the impact of vegetation cover dynamics on flooding and water balance in 11 steep (0.27-0.65 m m-1) catchments of the western Rift Valley escarpment of Northern Ethiopia, an area that experienced severe deforestation and degradation until the first half of the 1980s and considerable reforestation thereafter. Land cover change analysis was carried out using aerial photos (1936,1965 and 1986) and Google Earth imaging (2005 and 2014). Peak discharge heights of 332 events and the median diameter of the 10 coarsest bedload particles (Max10) moved in each event in three rainy seasons (2012-2014) were monitored. The result indicates a strong re- duction in flooding (R2 = 0.85, P<0.01) and bedload sediment supply (R2 = 0.58, P<0.05) with increas- ing vegetation cover. Overall, this study demonstrates that in reforesting steep tropical mountain catchments, magnitude of flooding, water balance and bedload movement is strongly determined by vegetation cover dynamics. -

High Incidence of Human Rabies Exposure in Northwestern Tigray, Ethiopia: a Four-Year Retrospective Study
RESEARCH ARTICLE High Incidence of Human Rabies Exposure in Northwestern Tigray, Ethiopia: A Four-Year Retrospective Study Gebreyohans Gebru Teklu1*, Teweldemedhn Gebretinsae Hailu1, Gebremedhin Romha Eshetu2 1 Department of Animal Sciences, College of Agriculture, Aksum University, Shire Campus, Shire, Ethiopia, 2 Department of Animal Production and Technology, College of Agriculture and Environmental Science, Adigrat University, Adigrat, Ethiopia * [email protected] a1111111111 Abstract a1111111111 a1111111111 a1111111111 Background a1111111111 Rabies is a fatal zoonotic disease that has been known in Ethiopia for centuries in society as ªMad Dog Diseaseº. It is an important disease with veterinary and public health significance in the North western zone of Tigray where previous studies have not been conducted. Fre- quent occurrence of outbreaks in the area led the researchers to carry out a four year retro- OPEN ACCESS spective study to estimate the incidence of human rabies exposure in Northwestern Tigray, Citation: Teklu GG, Hailu TG, Eshetu GR (2017) Ethiopia. High Incidence of Human Rabies Exposure in Northwestern Tigray, Ethiopia: A Four-Year Methodology Retrospective Study. PLoS Negl Trop Dis 11(1): e0005271. doi:10.1371/journal.pntd.0005271 A referent study was conducted on human rabies exposure cases recorded from 2012 to Editor: Charles E Rupprecht, Wistar Institute, 2015 at Suhul hospital, Shire Endaselase, Northwestern Tigray, Ethiopia. Exposure cases UNITED STATES included in this research constituted victims bitten by unprovoked dogs and who received Received: September 7, 2016 post exposure prophylaxis (PEP) at the hospital. Two thousand one hundred eighty human rabies exposure cases retrieved from the rabies case database were included in Accepted: December 19, 2016 this study. -

Addis Ababa University, College of Health Sciences, School of Public Health
ADDIS ABABA UNIVERSITY, COLLEGE OF HEALTH SCIENCES, SCHOOL OF PUBLIC HEALTH Ethiopian Field Epidemiology Training Program(EFELTP) Compiled Body of Works in Field Epidemiology By Brhanu Adhana(Bsc) Cohort IX Submitted to School of Graduate Studies of Addis AbabUniversity in Partial Fulfilment for the Degree of Master Public Health in Field Epidemiology June 2019 Addis Ababa Ethiopia ADDIS ABABA UNIVERSITY COLLEGE OF HEALTHS CIENCES SCHOOL OF PUBLIC HEALTH Ethiopian Field Epidemology Trainning Program(EFETP) Compiled Body Of Work In Field Epidemiology By Brhanu Adhana(Bsc) Sumitted to the School of Graduate Studies Addis Ababa University in Parial Fifulment for the Degree of Master of Public Health in Field Epidemiology JUNE 2019 ADDIS ABABA ETHIOPIA ADDIS ABABA UNIVERSITY, COLLEGE OF HEALTH SCIENCES SCHOOL OF PUBLIC HEALTH Ethiopian Field Epidemiology Training Program (EFETP) Compiled Body of Works in Field Epidemiology By Brhanu Adhana Submitted to the School of Graduate Studies of Addis Ababa University in Partial Fulfillment for the Degree of Master of Public Health in Field Epidemiology Mentors Mr. Yimer Seid (MPH in Epi and Bio) Mr. Muluken Gizaw (MPH) June 2019 Addis Ababa ethiopia ADDIS ABABA UNIVERSITY, COLLEGE OF HEALTH SCIENCE SCHOOL OF PUBLIC HEALTH Ethiopian Field Epidemiology Training Program (EFELP) Compiled Body of Work in Field Epidemiology By Brhanu Adhana(Bsc) Submitted to the School of Graduate Studies of Addis Ababa University in Partial Fulfilment for the Degree of Master of Public Health in Field Epidemology Approval By Examiner Board --------------------------------- --------------------------- Chairman, School Graduate Committee ------------------------------------- ---------------------------- Advisor ----------------------------------- ----------------------------- Examiner ---------------------------------- ----------------------------- Examiner ------------------------------------------ ---------------------------------- Acknowledgement I would like to extend appreciation to my advisors Mr. Yimer Sied and Mr. -

Investment Opportunities in Mekelle, Tigray State, Ethiopia
MCI AND VCC WORKING PAPER SERIES ON INVESTMENT IN THE MILLENNIUM CITIES No 10/2009 INVESTMENT OPPORTUNITIES IN MEKELLE, TIGRAY STATE, ETHIOPIA Bryant Cannon December 2009 432 South Park Avenue, 13th Floor, New York, NY10016, United States Phone: +1-646-884-7422; Fax: +1-212-548-5720 Websites: www.earth.columbia.edu/mci; www.vcc.columbia.edu MCI and VCC Working Paper Series o N 10/2009 Editor-in-Chief: Dr. Karl P. Sauvant, Co-Director, Millennium Cities Initiative, and Executive Director, Vale Columbia Center on Sustainable International Investment: [email protected] Editor: Joerg Simon, Senior Investment Advisor, Millennium Cities Initiative: [email protected] Managing Editor: Paulo Cunha, Coordinator, Millennium Cities Initiative: [email protected] The Millennium Cities Initiative (MCI) is a project of The Earth Institute at Columbia University, directed by Professor Jeffrey D. Sachs. It was established in early 2006 to help sub-Saharan African cities achieve the Millennium Development Goals (MDGs). As part of this effort, MCI helps the Cities to create employment, stimulate enterprise development and foster economic growth, especially by stimulating domestic and foreign investment, to eradicate extreme poverty – the first and most fundamental MDG. This effort rests on three pillars: (i) the preparation of various materials to inform foreign investors about the regulatory framework for investment and commercially viable investment opportunities; (ii) the dissemination of the various materials to potential investors, such as through investors’ missions and roundtables, and Millennium Cities Investors’ Guides; and (iii) capacity building in the Cities to attract and work with investors. The Vale Columbia Center on Sustainable International Investment promotes learning, teaching, policy-oriented research, and practical work within the area of foreign direct investment, paying special attention to the sustainable development dimension of this investment. -

TIGRAY REGION : Who Does What Where (3W) (As of 21 January 2014)
(as of 21 January 2014) TIGRAY REGION : Who Does What Where (3W) Tigray Afar Amhara Eritrea Benshangul Gumuz Dire Dawa Addis Ababa Hareri CRS: Gambela î Oromia Somali SNNPR R REST: REST: dk dhk E Save the Children: Save the Children: D f f S NRC: ke Legend E REST:/ REST:k A International Boundary WVE:d hf CRS:î REST:d hk Regional Boundary Erob IMC: ! Zonal Boundary ! ! // ! Tahtay Adiyabo Save the Children: f Gulomekeda Woreda Boundary Laelay Adiyabo Mereb Leke Ahferom CRS: î n ! a REST: dhk Lake d ! u ! No Intervention/ No Data ! ! S Ganta Afeshum REST:d k Adwa Saesie Tsaedaemba Save the Children: f Other Region Wukro!Laelay Maychew ! North Western Tahtay Koraro Eastern WVE:d hfk Tahtay Maychew ! Clusters/Sectors Kafta Humera CRS: Agriculture ! Werei Leke î a Asgede Tsimbila Hawzen! Central REST:d hk Coordination Medebay Zana m Save the Children:f Education ! Naeder Adet Atsbi Wenberta d Western ! Food Wukro ! CRS:a / Welkait REST:d k î Kelete Aw! elallo REST:d k Food Security Kola Temben h ! Save the Children:f Tselemti Degua Temben f Health Save the Children: ! CRS:î Multi-Sectoral Assistance in f ! REST: / Refugee Camps Mekele! mdhk ! Tanqua Abergele Tsegede Nutrition REST:d k CRS: î Enderta Save the Children:d / ! ! Water and Sanitation NRC:d e/ WVE: lf REST:d hk WVE:d hfk k Shelter CRS: ak CCM:f e CRS: î Others (Climate Change, GBV, REST: / REST: dh dk Livelihood, etc) Interventions/Projects at Regional Level Hintalo Wejirat Save the Children: Save the Children: df df ! Saharti Samre 0 12.5 25 50 km CST: fk/ MCC: d ! WVE:d h CRS:h Handicap Int.: Save the Children: f d CRS: Creation date: 15 Jan.