Appendix of Stains
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Comparative Evaluation of Ziehl-Neelsen and Kinyoun Staining in the Diagnosis of Clinically Suspected Cases of Pulmonary Tuberculosis
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Asian Pacific Journal of Health Sciences Asian Pac. J. Health Sci., 2019; 6(4):37-42 e-ISSN: 2349-0659, p-ISSN: 2350-0964 ____________________________________________________________________________________________________________________________________________ Document heading doi: 10.21276/apjhs.2019.6.4.8 Original Research Article Comparative Evaluation of Ziehl-Neelsen and Kinyoun Staining in the Diagnosis of Clinically Suspected Cases of Pulmonary Tuberculosis Sachin Kumar Mishra1, Sonali Mishra2* 1Assistant Professor, Department of Microbiology, Atal Bihari Vajpayee Government Medical College, NH-86, In-front of Khel Parisar, Sanchi Rd, Vidisha, 464001, Madhya Pradesh, India 2Assistant Professor, Department of Biochemistry, Atal Bihari Vajpayee Government Medical College, NH-86, In-front of Khel Parisar, Sanchi Rd, Vidisha, 464001, Madhya Pradesh, India Received: 26-08-2019 / Revised: 17-11-2019 / Accepted: 26-11-2019 ABSTRACT Background: Bacteriological examination of sputum is the cornerstone in diagnosis of pulmonary tuberculosis in developing world, which is usually done using a Ziehl-Nelseen (ZN) method. However, due to limited laboratory facilities that can satisfy the procedure, applicability of this procedure appears to be adversely affected in field conditions and at peripheral health institutions. Hence, it has become necessary to look for a procedure which can be used as alternative in such conditions. Material and Methods: This was a cross sectional study conducted in the Department of Microbiology, Index Medical College Hospital & Research Centre, Indore, Madhya Pradesh in conjunction with the Chest TB Clinic of Index Hospital, New Delhi for a period of 1year [from February 2018 to January 2019]. -
Cold Acid Fast Staining Method: Efficacy in Diagnosis of Mycobacterium Tuberculosis
African Journal of Microbiology Research Vol. 3(9) pp. 546-549, September, 2009 Available online http://www.academicjournals.org/ajmr ISSN 1996-0808 ©2009 Academic Journals Full Length Research Paper Cold acid fast staining method: Efficacy in diagnosis of Mycobacterium tuberculosis Anita Pandey*, Molly Madan, Ashish K. Asthana, Ritu Kansal, Anupam Das Department of Microbiology, Subharti Medical College, Swami Vivekanand Subharti University, Meerut, Uttar Pradesh, India. Accepted 16 July, 2009 Ziehl Neelson, a carbol fuschin based stain, using the 3 component hot process is a standard staining technique for staining sputum smears for detection of Mycobacterium tuberculosis. We evaluated a 2 step cold staining method for detection of acid fast bacilli in sputum smears. 1836 sputum samples from patients of pulmonary tuberculosis were studied. Smears were prepared from each sample and slides were simultaneously stained by both methods and examined. The 2 step cold stain method was found to be equally sensitive as the ZN method detecting 20% of cases, when the primary stain was kept for a period of 20 min. The CS method also has the advantage of being simple, economical and less cumbersome and in the procedure of staining, heating, a much too precise step in ZN method for large scale application, is eliminated. The CS method may therefore prove as a good alternative for diagnosis of M.tuberculosis, particularly in smaller laboratories and peripheral centers where there is limitation of the funds and equipments. Key words: Cold stain, acid fast bacilli, Mycobacterium tuberculosis. INTRODUCTION Demonstration of acid fast bacilli in the sputum is the methylene blue as decolouriser and counter-stain has been easiest, quickest and a reliable tool for the diagnosis of advocated as an alternative staining technique by various pulmonary tuberculosis (WHO, 1974). -

Isolation of an Acid-Fast Organism from the Aqueous Humor in a Case of Sarcoidosis
Henry Ford Hosp Med Journal Vol 27, No 2, 1979 Isolation of an Acid-Fast Organism from the Aqueous Humor in a Case of Sarcoidosis C. L. Barth, PhD,* M. S. Judge, MS,** L. H. Mattman, PhD,** and P. C. Hessburg, MD * * * The anterior chamber fluid from the eye of this patient with Introduction sarcoidosis was found to contain microcolonies of a cell- wall-deficient organism that was propagated and identified as acid-fast by the Intensified Acid-Fast stain. The colonies Anterior uveitis is frequently a local manifestation of were inoculated into mice and retrieved from the dead or systemic Boeck's sarcoidosis.^-^ In fact, an early name for sacrificed animals. This report suggests that the acid-fast sarcoidosis was uveoparotid fever. In such cases the aque microbe in the aqueous humor of this case of uveitis- ous humor appears to be sterile by routine culture methods. sarcoidosis may be the same organism as that found in the Similarly, in the case described here no classical microorga blood in sarcoidosis. Thus, it may be associated not only nisms appeared in a battery of media for aerobes, an with the primary disease, but also with the complications of aerobes. Mycoplasma, Mycobacteria, and fungi. However, Boeck's sarcoidosis. special media and staining detected an organism which resembles the isolates from the blood of nine other cases of Boeck's sarcoidosis evaluated in a parallel study.^ Data regarding four ofthese patients have been published.^ This acid-fast organism remains to be identified, but wfth im proved staining and culture methods diagnosis of sar- coidosis-and its complications may be facilitated. -
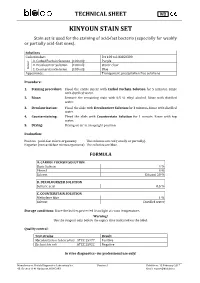
Kinyoun Stain Set
TECHNICAL SHEET IVD KINYOUN STAIN SET Stain set is used for the staining of acid-fast bacteria (especially for weakly or partially acid-fast ones). Solutions Code number: 3 x 100 ml: KIS60300 A. Carbol Fuchsin Solution (100 ml): Purple B. Decolourizer Solution (100 ml): Water clear Colour Colour C. Counterstain Solution (100 ml): Blue Appearance: Transparent, precipitation free solutions Procedure: 1. Staining procedure: Flood the entire smear with Carbol Fuchsin Solution for 5 minutes. Rinse with distilled water. 2. Rinse: Remove the remaining stain with 0,5 % ethyl alcohol. Rinse with distilled water. 3. Decolourization: Flood the slide with Decolourizer Solution for 3 minutes. Rinse with distilled water. 4. Counterstaining: Flood the slide with Counterstain Solution for 1 minute. Rinse with tap water. 5. Drying: Drying on air in an upright position. Evaluation: Positive (acid-fast micro-organism): The colonies are red (wholly or partially). Negative (non-acid-fast micro-organisms): The colonies are blue. FORMULA A. CARBOL FUCHSIN SOLUTION Basic fuchsin 4 % Phenol 8 % Solvent Ethanol 20 % B. DECOLOURIZER SOLUTION Sulfuric acid 0,5 % C. COUNTERSTAIN SOLUTION Methylene blue 1 % Solvent Distilled water Storage conditions : Store the bottles protected from light at room temperature. Warning! Use the reagent only before the expiry date indicated on the label. Quality control: Test strains Result Mycobacterium tuberculosis ATCC 25177 Positive Escherichia coli ATCC 25922 Negative In vitro diagnostics - for professional use only! Manufacturer: Biolab Diagnostics Laboratory Inc. Version: 1. Valid from: 15 February 2017 43. Öv utca 1141 Budapest, HUNGARY Email: [email protected] . -

HS805-AMB Cold ZN – Kinyoun Stain Pack Counterstain: Alcoholic Methylene Blue
HS805-AMB Cold ZN – Kinyoun Stain Pack counterstain: Alcoholic Methylene Blue Stain pack consists of: HS180 – Carbol Fuchsin (Kinyoun) HS787 – ZN Decolouriser HS500 – Methylene Blue (1% w/v alcoholic) Issue 3/08.2014 SDS Ref: HS180 Carbol Fuchsin ( Kinyoun) v3 Review Date: 20.08.2014 Print Date: 20.08.2014 SAFETY DATA SHEET This Safety Data Sheet contains information concerning the potential risks to those involved in handling, transporting and working with this material, as well as describing potential risks to the environment. This information must be made available to those who may come into contact with the material or are responsible for the use of the material. This Safety Data Sheet is prepared in accordance with formatting described in the REACH Regulation (EC) No 1907/2006 and (EU) No 453/2010 SECTION 1. Identification of the substances/mixture and of the company/undertaking . 1.1 Product Identifier Product Name: Carbol Fuchsin ( Kinyoun ) Product Number: HS180 Brand: TCS Biosciences IUPAC name not determined 1.2 Relevant identified uses of the substance or mixture and uses advised against Identified uses: Laboratory Reagent 1.3 Details of the supplier of the safety data sheet Company: TCS Biosciences Ltd Botolph Claydon, Buckingham, MK18 2LR, UK Telephone: +44 (0) 1296 714222 Email address: [email protected] Web address: www.tcsbiosciences.co.uk 1.4 Emergency telephone number In case of emergency: 24hr contact number: +44 (0)1296 711205 SECTION 2. Hazards Identification . 2.1 Classification of the substance or mixture Classification in accordance with the Classification Labelling and Packaging Regulation EC (no) 1272/2008: Flammable Liquid ( Category 3) Acute inhalation toxicity, (Category 3) Carcinogenic (Category 2) Mutagenic ( Category 2) Skin corrosion (Category 1B) Specific target organ toxicity — repeated exposure- Category 2 Classification according to Directive 1999/45/EEC & 67/548/EEC and its amendments Flammable Harmful by inhalation, in contact with the skin and if swallowed. -

Diagnostic Stains & Laboratory Reagents
polysciences.com Diagnostic Stains & Laboratory Reagents • Cytology • Dermatology • General Reagents • Hematology • Histology • Microbiology U.S. Corporate Headquarters | 400 Valley Rd, Warrington, PA 18976 | 1(800) 523-2575 (215) 343-6484 | Fax 1(800) 343-3291 | [email protected] Polysciences Europe GmbH | Badener Str. 13, 69493 Hirschberg an der Bergstr., Germany | +(49) 6201 845 20 0 | Fax +(49) 6201 845 20 20 | [email protected] Polysciences Asia Pacific, Inc. | 2F-1, 207 DunHua N. Rd. Taipei, Taiwan 10595 | (886) 2 8712 0600 | Fax (886) 2 8712 2677 | [email protected] Life Sciences Astral Diagnostics Catalog # Size Cytology Acrylic Mounting Medium . 25835-16 16 oz Histo/Cyto Mounting Medium in a toluene matrix using an acrylic resin for coverslipping . 25835-4 4 oz AQUAbluing Reagent . 25836-1 1 gal Bluing reagent used to provide crisp nuclear detail . Bluing Reagent . 25837-32 32 oz Lithium carbonate solution used to provide crisp nucler detail to cells . 25837-1 1 gal Human Colon, 20X Harris Hematoxylin, Eosin Y Pap Stain Gynecological stain used in combination with OG-6 and hematoxylin in the diagnosis of malignant cytological diseases . FDA approved for in vitro diagnostic use . EA-36 25865-32 32 oz 25865-1 1 gal EA-50 25841-2 .5 2 .5 gal EA-65 25842-2 .5 2 5. gal EASYpap . 25843-32 32 oz Gynecological single solution counterstain . A substitute to the traditional Eosin 25843-1 1 gal azure and Orange G . FDA approved for in vitro diagnostic use . Formalin 10%, Buffered . 25848-16 16 oz Most widely used fixative used for routine processing of tissue in histology laboratories . -

Gram Stain Kit (Gram Fuchsin Counterstain)
Simplicity for Science Stain Kits 1 Contact Us About Us +44 (0) 161 366 5123 Atom Scientific is a specialised manufacturer of diagnostic reagents [email protected] with over 50 years in delivering exceptional quality to the life science industry throughout the world +44 (0) 1704 33 7167 ISO15189 compliant products simply delivering consistency History Quality Facilities www.atomscientific.com and reliability to Life Sciences Established in 2009, Atom Our Quality Management In 2014, the company Scientific is a specialist Systems are Certificated to opened our current single Orders manufacturer of diagnostic ISO9001:2008 site facility in Manchester, stains and reagents for Life enabling Atom Scientific Orders can be placed On-Line, by Email or by Fax Science Laboratories Our QA/Compliance Team to significantly increase ensure our products are fully operational capacity, whilst As the business has grown auditable from raw material ensuring compliance to all [email protected] it has organically grown its to finished product current and future legislation. product range to incorporate We specialise in finished All orders must include Delivery and a comprehensive range Our Life Science Testing product pack sizes from Invoice Address and product of chemicals to suit our Laboratory is operated by 10ml/10gm to 25L/25Kg and information as follows: customer’s needs experienced Life Scientists, have manufacturing capacity ensuring our products • Product Code for batches from 500ml • Product Name Our Primary Aims are to are compliant -

The Color of Tissue Diagnostics Routine Stains, Special Stains and Ancillary Reagents
The Color of Tissue Diagnostics Routine Stains, Special Stains and Ancillary Reagents The life science business of Merck KGaA, Darmstadt, Germany operates as MilliporeSigma in the U.S. and Canada. For over years, 100routine stains, special stains and ancillary reagents have been part of the MilliporeSigma product range. This tradition and experience has made MilliporeSigma one of the world’s leading suppliers of microscopy products. The products for microscopy, a comprehensive range for classical hematology, histology, cytology, and microbiology, are constantly being expanded and adapted to the needs of the user and to comply with all relevant global regulations. Many of MilliporeSigma’s microscopy products are classified as in vitro diagnostic (IVD) medical devices. Quality Means Trust As a result of MilliporeSigma’s focus on quality control, microscopy products are renowned for excellent reproducibility of results. MilliporeSigma products are manufactured in accordance with a quality management system using raw materials and solvents that meet the most stringent quality criteria. Prior to releasing the products for particular applications, relevant chemical and physical parameters are checked along with product functionality. The methods used for testing comply with international standards. For over Contents Ancillary Reagents Microbiology 3-4 Fixing Media 28-29 Staining Solutions and Kits years, 5-6 Embedding Media 30 Staining of Mycobacteria 100 6 Decalcifiers and Tissue Softeners 30 Control Slides 7 Mounting Media Cytology 8 Immersion -
L003566.C -- Kinyoun Stain Sets.Pdf
[+1] 800.221.6058 United States Directions For Use for the following: [+1] 360.260.2779 International Kinyoun Stain Set with Methylene Blue, Kinyoun Stain Set with Brilliant Green, Kinyoun Carbolfuchsin Stain, TB Decolorizer, Methylene Blue Counterstain, Brilliant Green Counterstain INTENDED USE SPECIMEN PROCESSING Alpha-Tec Systems, Inc. Kinyoun Stain Set with Methylene Blue, 1. Make a thin smear of the specimen over an area of 2-3 sq cm. Heat Kinyoun Stain Set with Brilliant Green; and components are fix by warming on a slide warmer (65-75ºC) for 10 minutes, or until recommended for use in qualitative procedures for the microscopic the smear is dry. If a Bunsen burner is used, pass the slide slowly detection of mycobacteria. 3 times over its cone of heat. Do not scorch. 2. Flood the smear with Kinyoun Carbolfuchsin Stain for 5 minutes. SUMMARY 3. Rinse with deionized or distilled water and drain. One of the earliest methods devised for the detection of the tubercle 4. Decolorize with TB Decolorizer for 3 minutes. bacillus is the microscopic staining technique. This method is valuable 5. Rinse with deionized or distilled water and drain. for the rapid initial step in the presumptive diagnosis of mycobacterial 6. Repeat decolorization for 1-2 minutes or until no red stain appears. infections and provides information about the number of acid-fast bacilli 7. Rinse with deionized or distilled water and drain. present. Species of Nocardia and Rhodococcus are also partially acid- 8. Flood smear with Methylene Blue or Brilliant Green Counterstain fast. Three types of staining procedures are used for the detection of for 3-4 minutes. -

Histology Specimen Collection Manual
Lee Memorial Health System Lee County, FL CLINICAL LABORATORY HISTOLOGY SPECIMEN COLLECTION MANUAL Abdominal Fluid Container No fixative in an appropriate sized container. Minimum Volume 1 mL Performed Monday - Friday Location CCH, GCMC, HPMC, LMH Special Instructions The container must contain 5 units of heparin for every 1 mL of aspirated fluid. Abcess Container Any appropriate sized container Fixative 10 % Formalin Performed Monday - Friday Location CCH, GCMC, HPMC, LMH Special Instructions Fresh tissue not needed unless Frozen or ORC requested. Abortion/Products of Conception (With no request for Chromosome Analysis/Cytogenetics) Container Any appropriate sized container. Fixative 10% Formalin Performed Monday - Friday Location CCH, GCMC, HPMC, LMH Special Instructions If Chromosome Analysis/Cytogenetics is requested - no Fixative. See Chromosome Analysis/Cytogenetics Acid Fast Bacilli/AFB (Kinyoun's Stain) - Brushings Container Any appropriate sized container or holder for glass slides. Fixative Spray alcohol fixative/70%-85% alcohol (ethyl or reagent) Performed Monday - Friday Location GCMC Rev. 04/13 Page 1 of 44 Acid Fast Bacilli/AFB (Kinyoun's Stain) - Fluid Container Any appropriate sized container Fixative None - Fresh Fluid Performed Monday - Friday Location GCMC Special Instructions Please note request for this stain on Histology Requisition in Epic. Acid Fast Bacilli/AFB (Kinyoun's Stain) - Tissue Container Any appropriate sized container Fixative 10% Formalin Performed Monday - Friday Location GCMC Special Instructions Please note request for this stain on Histology Requisition in Epic. Adenoids Container Any appropriate sized container Fixative 10% Formalin Performed Monday - Friday Location CCH, GCMC, HPMC, LMH Special Instructions Fresh tissue not needed unless Frozen or ORC requested. Adnexa Container Any appropriate sized container Fixative 10% Formalin Performed Monday - Friday Location CCH, GCMC, HPMC, LMH Special Instructions Fresh tissue not needed unless Frozen or ORC requested. -

Special Staining Line
Special AUTO staining kit for Tiziano stainer A.F.O.G. (Acid Fuchsin Orange G) 250 tests 010307/AUTO Acid fast bacteria acc. Ziehl - Neelsen 250 tests 010201/AUTO NSH winning Staining * - Art of the Stain Contest 2019 Acid fast bacteria acc. Ziehl - Neelsen modified acc. Fite 250 tests 010202/AUTO Alcian blue pH 1,0 acc. Dorling 250 tests 010205/AUTO Alcian blue pH 1,5 acc. Dorling 250 tests 010206/AUTO Alcian blue pH 2,5 acc. Dorling 250 tests 010207/AUTO Acid Orcein acc. Shikata 250 tests 010251/AUTO Alcian yellow - Toluidine blue 250 tests 010269/AUTO Congo Red 250 tests 010214/AUTO Diastase Buffer 250 tests 010216/AUTO Fouchet Van Gieson acc. Kutlick 250 tests 010220/AUTO Giemsa acc. Lennert 250 tests 010225/AUTO Special Staining Line Goldner’s Trichrome 250 tests 010224/AUTO Gomori’s Trichrome 250 tests 010302/AUTO Hale Reaction - colloidal iron 250 tests 010312/AUTO Hematoxylin Eosin - fast method 100 tests 010263 M.S.B. 250 tests 010255/AUTO Mallory’s Trichrome acc. McFarlane 250 tests 010227/AUTO Masson’s Trichrome 250 tests 010210/AUTO May - Grunwald - Giemsa - fast method 100 tests 010253 May - Grunwald - Giemsa for smears 100 tests 010802 Methyl green Pyronin 250 tests 010230/AUTO Mucicarmine acc. Mayer 250 tests 010245/AUTO Oil Red O acc. Johnson 250 tests 010303/AUTO P.A.S. acc. Hotchkiss - McManus 250 tests 010231/AUTO P.A.S. acc. Morel-Maronger 250 tests 010232/AUTO P.A.S. acc. Pearse 250 tests 010233/AUTO Perls 250 tests 010236/AUTO Perls - Van Gieson 250 tests 010237/AUTO Section of intestinal wall (anorectal junction) stained with Picromallory 250 tests 010238/AUTO the M.S.B. -

Special Staining Line
Special AUTO staining kit for Tiziano stainer A.F.O.G. (Acid Fuchsin Orange G) 250 tests 010307/AUTO Acid fast bacteria acc. Ziehl - Neelsen 250 tests 010201/AUTO NSH winning Staining * - Art of the Stain Contest 2019 Acid fast bacteria acc. Ziehl - Neelsen modified acc. Fite 250 tests 010202/AUTO Alcian blue pH 1,0 acc. Dorling 250 tests 010205/AUTO Alcian blue pH 1,5 acc. Dorling 250 tests 010206/AUTO Alcian blue pH 2,5 acc. Dorling 250 tests 010207/AUTO Acid Orcein acc. Shikata 250 tests 010251/AUTO Alcian yellow - Toluidine blue 250 tests 010269/AUTO Congo Red 250 tests 010214/AUTO Diastase Buffer 250 tests 010216/AUTO Fouchet Van Gieson acc. Kutlick 250 tests 010220/AUTO Giemsa acc. Lennert 250 tests 010225/AUTO Special Staining Line Goldner’s Trichrome 250 tests 010224/AUTO Gomori’s Trichrome 250 tests 010302/AUTO Hale Reaction - colloidal iron 250 tests 010312/AUTO Hematoxylin Eosin - fast method 100 tests 010263 M.S.B. 250 tests 010255/AUTO Mallory’s Trichrome acc. McFarlane 250 tests 010227/AUTO Masson’s Trichrome 250 tests 010210/AUTO May - Grunwald - Giemsa - fast method 100 tests 010253 May - Grunwald - Giemsa for smears 100 tests 010802 Methyl green Pyronin 250 tests 010230/AUTO Mucicarmine acc. Mayer 250 tests 010245/AUTO Oil Red O acc. Johnson 250 tests 010303/AUTO P.A.S. acc. Hotchkiss - McManus 250 tests 010231/AUTO P.A.S. acc. Morel-Maronger 250 tests 010232/AUTO P.A.S. acc. Pearse 250 tests 010233/AUTO Perls 250 tests 010236/AUTO Perls - Van Gieson 250 tests 010237/AUTO Section of intestinal wall (anorectal junction) stained with Picromallory 250 tests 010238/AUTO the M.S.B.