Original Article
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

LIST of HOSPITALS WITHIN NCR 1. Medical Center Manila 2. Philippine General Hospital 3
LIST OF HOSPITALS WITHIN NCR 1. Medical Center Manila 2. Philippine General Hospital 3. Amisola Maternity Hospital - Hermosa Street, Manuguit, Tondo 4. Canossa Health and Social Center Foundation, Inc. - E. Jacinto Street, Magsaysay Village 5. Chinese General Hospital and Medical Center - Blumentritt Road, Santa Cruz 6. Clinica Arellano General Hospital - Doroteo Jose Street, Santa Cruz 7. De Ocampo Memorial Medical Center - Nagtahan Street, Santa Mesa 8. Dr. Jose Fabella Memorial Hospital - Lope de Vega Street, Santa Cruz 9. Dr. Mirando Unciano, Sr. Medical Center - V. Mapa Street, Santa Mesa 10. Esperanza Health Center - Santa Mesa 11. F. Lanuza Health Center and Lying-in Clinic - Alvarez Street, Santa Cruz 12. GAT Andres Bonifacio Memorial Medical Center - Delpan Street, Tondo 13. Hospital of the Infant Jesus - Laong Laan Street, Sampaloc 14. Jose R. Reyes Memorial Medical Center - San Lazaro Compound, Rizal Avenue, Santa Cruz 15. Justice Jose Abad Santos General Hospital - Numancia St. Binondo Manila 16. Manila Doctors' Hospital - United Nations Avenue, Ermita 17. Maria Clara Health Center and Lying-in Clinic - Maria Clara corner Prudencio Streets 18. Mary Chiles General Hospital - Dalupan Street, Sampaloc 19. Mary Johnston Hospital - Juan Nolasco Street, Tond 20. Medical Center Manila- General Luna Street, Ermita 21. Metropolitan Medical Center - Masangkay Street, Tondo 22. Nephrology Center of Manila - San Andres Street corner Leon Guinto Street, Malate 23. Ospital ng Maynila Medical Center - Quirino Avenue corner Roxas Boulevard, Malate 24. Ospital ng Sampaloc - Geronimo Street, Sampaloc 25. Ospital ng Tondo - Jose Abad Santos Avenue, Tondo 26. Our Lady of Lourdes Hospital - P. Sanchez Street, Santa Mesa 27. Pedro Gil Health Center and Lying-in Clinic - A. -
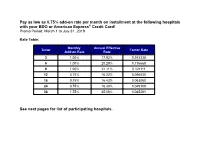
Pay As Low As 0.75% Add-On Rate Per Month on Installment at The
Pay as low as 0.75% add-on rate per month on installment at the following hospitals with your BDO or American Express® Credit Card! Promo Period: March 1 to July 31, 2019 Rate Table: Monthly Annual Effective Tenor Factor Rate Add-on Rate Rate 3 1.00% 17.92% 0.343338 6 1.00% 20.29% 0.176668 9 1.00% 21.11% 0.121111 12 0.75% 16.22% 0.090835 18 0.75% 16.43% 0.063060 24 0.75% 16.43% 0.049169 36 1.75% 35.08% 0.045281 See next pages for list of participating hospitals. Hospital Name Address METRO MANILA HOSPITALS Asian Hospital And Medical Center 2205 Civic Drive Filinvest Corporation City, Alabang, Muntinlupa Cardinal Santos Medical Center Cardinal Santos Medical Center, Wilson St., Greenhills, San Juan Chinese General Hospital 286 Blumentritt Road, Sta. Cruz, Manila, Philippines De Los Santos Medical Center 201 E. Rodriguez Sr. Boulevard, Quezon City Dihmesco General Hospital 215 Gen Luis St. Novaliches, Quezon City Dr. Jesus C. Delgado Memorial Hospital (Delgado Clinic) 7 Kamuning Road, Quezon City, Metro Manila, Philippines Fatima University Medical Center 120 McArthur Highway, Valenzuela City Makati Medical Center 2 Amorsolo Street, Makati City Medical Center Paranaque Dr. A. Santos Avenue, Sucat Road, Paranaque City Our Lady Of Lourdes Hospital 46 P. Sanchez Street, Sta Mesa, Manila Paranaque Premier Hospital & Medical Center Lot 2 Amvel Business Park, Dr. A Santos Avenue, Brgy. San Dionisio, Paranaque City Pasig Doctors Medical Center 254 Eulogio Amang Rodriguez Avenue, Pasig, Metro Manila Perpetual Help Medical Center Real Sr., Pamplona, Las Pinas City South Super Highway Medical Center KM 17 West Service Road. -
Directory of Disability Inclusive Schools, for Students with Disabilities to Enjoy Their Right to to Education
DIRECTORY OF DISABILITY INCLUSIVE SCHOOLS Basic Education Schools Providing Services to Students with Disabilities NATIONAL COUNCIL ON DISABILITY AFFAIRS Disablity Inclusive Schools 2016 Disclaimer: The Schools included in this Directory was updated this 2016. Information of Schools that have not responded is still included in this list which we have gathered from previous sources, such as the Department of Education – SPED, National Council on Disability Affairs (NCDA) Directory of Rehabilitation Resources, Autism Society Philippine’s (ASP) Directory of Resources, letter and phone inquiries, Internet, and personal knowledge and encounters. To further enrich, update and make this Directory most useful to our target users, please submit suggestions, corrections, comments or information on other Disability schools, to our email address at [email protected]. TABLE OF CONTENTS Page | 2 Disablity Inclusive Schools DISABILITY INCLUSIVE SCHOOLS: Basic Education Schools Providing Services to Students with Disabilities Page | 3 Disablity Inclusive Schools Page About the Directory 7 Caloocan City 8 Las Piñas City 11 Makati City 15 Malabon City 16 Mandaluyong City 18 Manila 20 Marikina City 26 Muntinlupa City 28 Navotas City 30 Parañaque City 30 Pasay City 35 Pasig City 36 Quezon City 38 San Juan City 53 Taguig City 55 Valenzuela City 56 Government Speciality School 59 Ilocos Norte 61 Ilocos Sur 63 La Union 65 Pangasinan 67 Cagayan 73 Isabela 75 Nueva Vizcaya 77 Quirino 78 Benguet 79 Ifugao 80 Kalinga 81 Mountain Province 82 Aurora 83 Page | 4 -
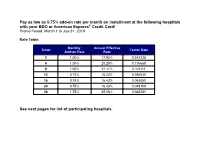
Pay As Low As 0.75% Add-On Rate Per Month on Installment at The
Pay as low as 0.75% add-on rate per month on installment at the following hospitals with your BDO or American Express® Credit Card! Promo Period: March 1 to July 31, 2019 Rate Table: Monthly Annual Effective Tenor Factor Rate Add-on Rate Rate 3 1.00% 17.92% 0.343338 6 1.00% 20.29% 0.176668 9 1.00% 21.11% 0.121111 12 0.75% 16.22% 0.090835 18 0.75% 16.43% 0.063060 24 0.75% 16.43% 0.049169 36 1.75% 35.08% 0.045281 See next pages for list of participating hospitals. Hospital Name Address METRO MANILA HOSPITALS Asian Hospital And Medical Center 2205 Civic Drive Filinvest Corporation City, Alabang, Muntinlupa Cardinal Santos Medical Center 10 Wilson St., Greenhills West, San Juan, San Juan City Chinese General Hospital 286 Blumentritt Road, Sta. Cruz, Manila De Los Santos Medical Center 201 E. Rodriguez Sr. Boulevard, Quezon City Dihmesco General Hospital 215 Gen Luis St. Novaliches, Quezon City Dr. Jesus C. Delgado Memorial Hospital 7 Kamuning Road, Quezon City (Delgado Clinic) Fatima University Medical Center 120 McArthur Highway, Valenzuela City Makati Medical Center 2 Amorsolo Street, Makati City Medical Center Paranaque Dr. A. Santos Avenue, Sucat Road, Paranaque City Our Lady Of Lourdes Hospital 46 P. Sanchez Street, Sta Mesa, Manila Pasig Doctors Medical Center 254 Eulogio Amang Rodriguez Avenue, Pasig City Perpetual Help Medical Center Real Sr., Pamplona, Las Pinas City South Super Highway Medical Center KM 17 West Service Road. Brgy. Marcelo, Paranaque City St Clares Medical Center 1838 Dian St., Palanan, Makati City St. -
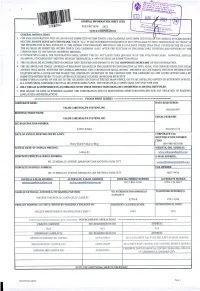
Ictdl Jiiu /R^ GENERAL INFORMATION SHEET (GIS) M & \W BT , for the YEAR 2021 RECEIVCDSOB ------—— STOCK CORPORATION GENERAL INSTRUCTIONS: [ ------^7 1
* ■ «=f S On,j A r>9«=» ICTDl jiiu /r^ GENERAL INFORMATION SHEET (GIS) m & \W BT , FOR THE YEAR 2021 RECEIVCDSOB -------—— STOCK CORPORATION GENERAL INSTRUCTIONS: [ --------------- ^7 1. FOR USER CORPORATION: THIS GIS SHOULD BE SUBMITTED WITHIN THIRTY (30) CALENDAR DAYS FROM THE DATE Or THE ANNUAL STOCKHOLDERS' MEETING. DO NOT LEAVE ANY ITEM BLANK. WRITE "N.A." IF THE INFORMATION REQUIRED IS NOT APPLICABLE TO THE CORPORATION OR "NONE" IF THE INFORMATION IS NON-EXISTENT. IF THE ANNUAL STOCKHOLDERS' MEETING IS HELD ON A DATE OTHER THAN THAT STATED IN THE BY-LAWS, THE GIS SHALL BE SUBMITTED WITHIN THIRTY (30) CALENDAR DAYS AFTER THE ELECTION OF THE DIRECTORS, TRUSTEES AND OFFICERS OF THE CORPORATION AT THE ANNUAL MEMBERS' MEETING. 2. IF NO MEETING IS HELD, THE CORPORATION SHALL SUBMIT THE GIS NOT LATER THAN JANUARY 30 OF THE FOLLOWING YEAR. HOWEVER, SHOULD AN ANNUAL STOCKHOLDERS' MEETING BE HELD THEREAFTER, A NEW GIS SHALL BE SUBMITTED/FILED. 3. THIS GIS SHALL BE ACCOMPLISHED IN ENGLISH AND CERTIFIED AND SWORN TO BY THE CORPORATE SECRETARY OF THE CORPORATION. 4. THE SEC SHOULD BE TIMELY APPRISED OF RELEVANT CHANGES IN THE SUBMITTED INFORMATION AS THEY ARISE. FOR CHANGES RESULTING FROM ACTIONS THAT AROSE BETWEEN THE ANNUAL MEETINGS, THE CORPORATION SMALL SUBMIT AMENDED GIS CONTAINING THE NEW INFORMATION TOGETHER WITH A COVER LETTER SIGNED THE CORPORATE SECRETARY OF THE CORPORATION. THE AMENDED GIS AND COVER LETTER SHALL BE SUBMITTED WITHIN SEVEN (7) DAYS AFTER SUCH CHANGE OCCURED OR BECAME EFFECTIVE. 5. SUBMIT FOUR (4) COPIES OF THE GIS TO THE RECEIVING SECTION AT THE SEC MAIN OFFICE, OR TO SEC SATELLITE OFFICES OR EXTENSION OFFICES. -

PCI Direct Billing Network 2019 Add
PH ILIPPINES TH AILAND VIETNAM SINGAPORE MYAN MAR CAMBO DIA LAOS TAIWAN INDONESIA MALAYSIA More than just ins u r anc e . P a cific Cross pro vid e s p e a ce o f m i n d . PHILIPPINES HOSPITAL PLAN COORDINATOR’S REGION PROVINCE CITY HOSPITAL ADDRESS CONTACT NO. EMAIL ADDRESS PLAN COORDINATOR SCHEDULE CONTACT NO. CORDILLERA DR. ALFREDO IGAMA Rm. N3B13, Mon - Sat, 1 - 6 pm / RM. 215, Tues. NOTRE DAME DE CHARTRES 25 Gen. Luna Road., Baguio (074) 619-8530 to 34, ADMINISTRATIVE Benguet Baguio (Surgery) / DR.JUSTINA 09175061928 9am-5pm , Wed & Fri. 9am - 1pm , Sat. 9am- HOSPITAL City Fax No.: (074) 304-5960 REGION (CAR) CALIBUSO (I.M./Cardilogy) 12nn (074) 442-5701 to 02, CORDILLERA ST. LOUIS UNIVERSITY OF THE Assump on Road Extension, Fax No.: (074) 442-5624 DR. ALFREDO IGAMA ADMINISTRATIVE Benguet Baguio 09175061928 Mon - Sat, 9am - 12nn SACRED HEART Baguio City Billing No.: (074) 442- (Surgery) REGION (CAR) 3621 #849 General Luis St., NATIONAL CAPITAL Metro (02) 983 5363 DR. EDDIE D. ACEBEDO (Plan Caloocan ACEBEDO GENERAL HOSPITAL Bagbaguin, Caloocan Tel. No.: 983-5363 REGION (NCR) Manila (02) 935 9139 coordinator) City (02) 8524 7360 Proceed to ER/OP, Company NATIONAL CAPITAL Metro ADVENTIST MEDICAL CENTER (Company Sec.) Pasay Donada St., Pasay City Sec on, Company REGION (NCR) Manila MANILA (02) 8525 9191 sec on( OP/IP), ER ( OP/IP) (Trunkline) Ayala Alabang Village, NATIONAL CAPITAL Metro Dra. Annie Ty ( Plan Mun nlupa ALABANG MEDICAL CENTER Madrigal Business (02) 8850 8719 REGION (NCR) Manila Coordinator) Park, Mun nlupa City 297 Mon llano St., Alabang, NATIONAL CAPITAL Metro ALABANG MEDICAL CLINIC - Mun nlupa Mun nlupa (02) 8842 0680 Contact Person: Ana Luba 842-1639 /842-1723 REGION (NCR) Manila MONTILLANO City ALLIED CARE EXPERTS (ACE) NATIONAL CAPITAL Metro 884 P. -

Hospital List Page 1
Hospital List Hospital Name Address METRO MANILA HOSPITALS 1 Asian Hospital And Medical Center 2205 Civic Drive Filinvest Corporation City, Alabang, Muntinlupa 2 Cardinal Santos Medical Center Cardinal Santos Medical Center, Wilson St., Greenhills, San Juan 3 Chinese General Hospital* 286 Blumentritt Road, Sta. Cruz, Manila, Philippines 4 De Los Santos Medical Center 201 E. Rodriguez Sr. Boulevard, Quezon City 5 Dihmesco General Hospital 215 Gen Luis St. Novaliches, Quezon City Dr. Jesus C. Delgado Memorial Hospital 6 7 Kamuning Road, Quezon City, Metro Manila, Philippines (Delgado Clinic)* 7 Fatima University Medical Center 120 McArthur Highway, Valenzuela City 8 Medical Center Paranaque Dr. A. Santos Avenue, Sucat Road, Paranaque City 9 Our Lady Of Lourdes Hospital 46 P. Sanchez Street, Sta Mesa, Manila Lot 2 Amvel Business Park, Dr. A Santos Avenue, Brgy. San Dionisio, 10 Paranaque Premier Hospital & Medical Center Paranaque City 11 Pasig Doctors Medical Center* 254 Eulogio Amang Rodriguez Avenue, Pasig, Metro Manila 12 South Super Highway Medical Center KM 17 West Service Road. Brgy. Marcelo, Paranaque City 13 St Clares Medical Center 1838 Dian St., Palanan, Makati 14 St. Luke’s BGC* Rizal Drive corner 32nd St. and 5th Drive, Taguig, 1634 Metro Manila 15 St Luke's Hospital E. Rodriguez Avenue, Quezon City 16 Tricity Medical Center C. Raymundo Avenue Corner F. Legaspi St., Maybunga, Pasig University Of The East Ramon Magsaysay Memorial 17 64 Aurora Boulevard, Brgy. Dona Imelda, Quezon City Medical Center 18 University Of Perpetual Help Dalta Medical Center Real Sr., Pamplona, Las Pinas City 19 VRP Medical Center 163 EDSA, Malamig, Mandaluyong LUZON HOSPITALS 1 Angeles Medical Center 641 Rizal Street, Angeles City 2 Angeles University Foundation MacArthur Highway, Angeles City Block 8, Lot 1A &1B Dewey Avenue, CBD Area, Subic Bay Freeport Zone, 3 Baypointe Hospital & Medical Center Olongapo City, Zambales 4 Bethany Hospital Widdoes Street, Barangay 2, San Fernando, La Union 5 Castro Maternity Hospital And Medical Center M. -
Intellectual Property Center, 28 Upper Mckinley Rd
Intellectual Property Center, 28 Upper McKinley Rd. McKinley Hill Town Center, Fort Bonifacio, Taguig City 1634, Philippines Tel. No. 238-6300 Website: http://www.ipophil.gov.ph e-mail: [email protected] Publication Date: 28 January 2021 1 ALLOWED MARKS PUBLISHED FOR OPPOSITION .................................................................................................... 2 1.1 ALLOWED NATIONAL MARKS ............................................................................................................................................. 2 Intellectual Property Center, 28 Upper McKinley Rd. McKinley Hill Town Center, Fort Bonifacio, Taguig City 1634, Philippines Tel. No. 238-6300 Website: http://www.ipophil.gov.ph e-mail: [email protected] Publication Date: 28 January 2021 1 ALLOWED MARKS PUBLISHED FOR OPPOSITION 1.1 Allowed national marks Application No. Filing Date Mark Applicant Nice class(es) Number 16 June 1 4/2017/00009271 Green Cross, Inc. [PH] 5 2017 8 March Tristellar Trading Corporation 2 4/2018/00004269 ROYALE 30 2018 [PH] 24 April 3 4/2018/00006882 GAMEBOOKR Isaiah A. Mangundayao [PH] 35 2018 Mary Assumption S. Bautista- 20 June 4 4/2018/00010337 MARISON`S Villareal [PH] andMarison`s 43 2018 Home Cuisine, Inc. [PH] 8 October Batuhan Upland and Lowland 5 4/2018/00017813 BULFA 30 2018 Farmers Association [PH] 10 October 6 4/2018/00018191 KABAB REPUBLIC Ecko8 Trading Inc. [PH] 43 2018 10 October 7 4/2018/00018192 NAY LEBANESE Ecko8 Trading Inc. [PH] 43 2018 17 October 8 4/2018/00018674 SEACOM Seacom, Inc [PH] 7 and37 2018 26 May 9 4/2018/00502319 TUTU PASTRIES Mercado, Cearita [PH] 35 2018 11 July 10 4/2018/00503154 PW EVENTS MMM Partyworks Shop [PH] 35 2018 11 4/2019/00007456 7 May 2019 TICKETKO Journeytech Inc. -

NCR FY2013/Propfy2013 25-Jan-13 3:21:25 PM FY 2013 DPWH INFRASTRUCTURE PROGRAM NATIONAL CAPITAL REGION (Based on GAA)
NCR FY2013/PropFY2013 25-Jan-13 3:21:25 PM FY 2013 DPWH INFRASTRUCTURE PROGRAM NATIONAL CAPITAL REGION (Based on GAA) Physical Amount Implementing Name of Project/Location Scope of Work Target (P0'000) Office (1) (2) (3) (5) (6) NORTH MANILA DISTRICT ENGINEERING OFFICE 975,366 MANILA CITY, 1ST DISTRICT 220,669 Cong. Benjamin D.R. Asilo I. Locally Funded a. National Arterial and Secondary National Roads and Bridges 70,155 1. Assets Preservation of National Roads Generated from Pavement Management System/Highway Development and Management-4 (HDM-4) Intermittent Sections a. Preventive Maintenance 1. Secondary (Preventive Maintenance) a. R - 10 0.75 20,155 1. K0005 + 504 - K0005 + 980 Overlay 100mm w/ corrections 0.49 13,196 North Manila DEO 2. K0008 + 135 - K0006 + 386 Overlay 100mm w/ corrections 0.26 6,959 2. Roads to Address Critical Bottlenecks a. Traffic Decongestion 1. Widening of National Roads in Manila 1st District Widening 1.25 km 50,000 North Manila DEO b. Flood Control and Drainage Projects 3,972.14 lm 150,514 1. Flood Control in Manila 1st District a. Drainage Improvement along R-10 (Moriones to Pacheco) Drainage Improvement 409.14 lm 15,138 North Manila DEO b. Construction/Rehabilitation of Flood Control in Manila Construction/Rehabilitation 3,563.00 lm 135,376 North Manila DEO 1st District NCR FY2013/PropFY2013 25-Jan-13 3:21:25 PM FY 2013 DPWH INFRASTRUCTURE PROGRAM NATIONAL CAPITAL REGION (Based on GAA) Physical Amount Implementing Name of Project/Location Scope of Work Target (P0'000) Office (1) (2) (3) (5) (6) MANILA CITY, 2ND DISTRICT 172,908 Cong. -

(CSHP) DOLE-National Capital Region June 2018
REGIONAL REPORT ON THE APPROVED/CONCURRED CONSTRUCTION SAFETY & HEALTH PROGRAM (CSHP) DOLE-National Capital Region June 2018 No. Company Name and Address Project Name Date Approved Healthy Options Healthy Options Festival Mall Renovation 1 2/F Topy's Place, 3 Economia St. cor. Calle Industria, 6/4/2018 Unit 2005-2006 Level 2 Festival Supermall, Muntinlupa City Bagumbayan, Quezon City Demolition and Restoration of Existing Perimeter Fence at Maynilad Water Services Inc. 2 Bagbag Reservoir 6/14/2018 MWSS Compound, Katipunan Road, Balara, Quezon City F. Delos Santos St. Sauyo Road, Novaliches, Quezon City Proposed Construction of Bank of the Philippine Island Office - Carlo Poblete 3 2nd Floor, BPI M.H. Del Pilar Branch 6/4/2018 M.H. Del Pilar corner U.N. Avenue, Ermita, Manila M.H. Del Pilar corner U.N. Avenue, Ermita, Manila Enrique Fernandez Proposed Repair of Two (2) Storey Old House 4 6/5/2018 614 Trinidad St., Sta. Cruz, Manila 614 Trinidad St., Sta. Cruz, Manila Lory Anne V. Kim Proposed Renovation of Good Friends Holdings, Inc. 5 6/5/2018 1535 M. Adriatico St., Ermita, Manila 1535 M. Adriatico St., Ermita, Manila Helen Hular Piring Proposed Construction of Perimeter Fence 6 6/5/2018 1546 N. Zamora St., Tondo, Manila 1546 N. Zamora St., Tondo, Manila Proposed Renovation of Comworks Clickstore Ma. Elizabeth M. Leyeza / Comworks Inc. 7 Unit 33, C7 030, Lower Ground Floor, SM City Manila, Ermita, 6/14/2018 CWI Corporate Center 1050 Quezon Ave., Quezon City Manila Nonito Y. Lao / BRL Food Service Management, Inc. Proposed Repair of Kiosk (Yang's Hong Kong Style Noodle) 8 6/14/2018 20 Felipe Pike St., Bagon Ilog, Pasig City Park 'N Ride, Arroceros St., Ermita, Manila Jaime Lim Proposed Repair of Residential Building 9 6/14/2018 # 3581 Mag Arellano St., Bacood, Sta. -
Getting Options
GETTING OPTIONS A Handbook on Getting Education, Training and Work Options for Persons with Disabilities at the National Capital Region GETTING OPTIONS Copyright 2014 National Council on Disability Affairs All rights reserved Disclaimer Reproduction of material of this publication for sale or other commercial purposes, including publicity and advertising, is prohibited without the written permission from the National Council on Disability Affairs (NCDA). Application for permission should be addressed to the Executive Director with statement of purpose and extent of production. Published by: National Council on Disability Affairs NCDA Bldg., Isidora Street, Brgy. Holy Spirit, 1127 Quezon City 2 ISBN 978-621-95138-3-8 GETTING OPTIONS GETTING OPTIONS A Handbook on Getting Education, Training and Work Options for Persons with Disabilities at the National Capital Region 3 GETTING OPTIONS ACKNOWLEDGMENT: This Handbook is part of the fulfilment of my Re-Entry Action Plan for Australian Scholarship Awards on Master of Social Science Specialization in Human Service Management at the University of Newcastle, Australia. The Handbook aims to let the students, parents and service providers know where and how to get available resources in education, training and employment for persons with disabilities at the National Capital Region. Added also, are practical tips on how and what to prepare when getting these opportunities. I would like to sincerely thank NCDA Management for their support led by Acting Executive Director Carmen Reyes-Zubiaga. May I also acknowledge, Deputy Executive Director Mateo A. Lee, Jr., for motivating me as my coach during the initial development of this Handbook. Let me also thank my ever supportive Division Chief of Technical Cooperation Division Ms. -

Hospital List Page 1
Hospital List Hospital Name Address METRO MANILA HOSPITALS 1 Asian Hospital And Medical Center 2205 Civic Drive Filinvest Corporation City, Alabang, Muntinlupa 2 Cardinal Santos Medical Center Cardinal Santos Medical Center, Wilson St., Greenhills, San Juan 3 Chinese General Hospital* 286 Blumentritt Road, Sta. Cruz, Manila, Philippines 4 De Los Santos Medical Center 201 E. Rodriguez Sr. Boulevard, Quezon City 5 Dihmesco General Hospital 215 Gen Luis St. Novaliches, Quezon City Dr. Jesus C. Delgado Memorial Hospital 6 7 Kamuning Road, Quezon City, Metro Manila, Philippines (Delgado Clinic)* 7 Fatima University Medical Center 120 McArthur Highway, Valenzuela City 8 Medical Center Paranaque Dr. A. Santos Avenue, Sucat Road, Paranaque City 9 Our Lady Of Lourdes Hospital 46 P. Sanchez Street, Sta Mesa, Manila Lot 2 Amvel Business Park, Dr. A Santos Avenue, Brgy. San Dionisio, 10 Paranaque Premier Hospital & Medical Center Paranaque City 11 Pasig Doctors Medical Center* 254 Eulogio Amang Rodriguez Avenue, Pasig, Metro Manila 12 South Super Highway Medical Center KM 17 West Service Road. Brgy. Marcelo, Paranaque City 13 St Clares Medical Center 1838 Dian St., Palanan, Makati 14 St. Luke’s BGC* Rizal Drive corner 32nd St. and 5th Drive, Taguig, 1634 Metro Manila 15 St Luke's Hospital E. Rodriguez Avenue, Quezon City 16 Tricity Medical Center C. Raymundo Avenue Corner F. Legaspi St., Maybunga, Pasig University Of The East Ramon Magsaysay Memorial 17 64 Aurora Boulevard, Brgy. Dona Imelda, Quezon City Medical Center 18 University Of Perpetual Help Dalta Medical Center Real Sr., Pamplona, Las Pinas City 19 VRP Medical Center 163 EDSA, Malamig, Mandaluyong LUZON HOSPITALS 1 Angeles Medical Center 641 Rizal Street, Angeles City 2 Angeles University Foundation MacArthur Highway, Angeles City Block 8, Lot 1A &1B Dewey Avenue, CBD Area, Subic Bay Freeport Zone, 3 Baypointe Hospital & Medical Center Olongapo City, Zambales 4 Bethany Hospital Widdoes Street, Barangay 2, San Fernando, La Union 5 Castro Maternity Hospital And Medical Center M.