Hematopoietic Stem Cell Transplantation for Primary Immunodeficiency Disease
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

IDF Patient & Family Handbook
Immune Deficiency Foundation Patient & Family Handbook for Primary Immunodeficiency Diseases This book contains general medical information which cannot be applied safely to any individual case. Medical knowledge and practice can change rapidly. Therefore, this book should not be used as a substitute for professional medical advice. FIFTH EDITION COPYRIGHT 1987, 1993, 2001, 2007, 2013 IMMUNE DEFICIENCY FOUNDATION Copyright 2013 by Immune Deficiency Foundation, USA. REPRINT 2015 Readers may redistribute this article to other individuals for non-commercial use, provided that the text, html codes, and this notice remain intact and unaltered in any way. The Immune Deficiency Foundation Patient & Family Handbook may not be resold, reprinted or redistributed for compensation of any kind without prior written permission from the Immune Deficiency Foundation. If you have any questions about permission, please contact: Immune Deficiency Foundation, 110 West Road, Suite 300, Towson, MD 21204, USA; or by telephone at 800-296-4433. Immune Deficiency Foundation Patient & Family Handbook for Primary Immunodeficency Diseases 5th Edition This publication has been made possible through a generous grant from Baxalta Incorporated Immune Deficiency Foundation 110 West Road, Suite 300 Towson, MD 21204 800-296-4433 www.primaryimmune.org [email protected] EDITORS R. Michael Blaese, MD, Executive Editor Francisco A. Bonilla, MD, PhD Immune Deficiency Foundation Boston Children’s Hospital Towson, MD Boston, MA E. Richard Stiehm, MD M. Elizabeth Younger, CPNP, PhD University of California Los Angeles Johns Hopkins Los Angeles, CA Baltimore, MD CONTRIBUTORS Mark Ballow, MD Joseph Bellanti, MD R. Michael Blaese, MD William Blouin, MSN, ARNP, CPNP State University of New York Georgetown University Hospital Immune Deficiency Foundation Miami Children’s Hospital Buffalo, NY Washington, DC Towson, MD Miami, FL Francisco A. -

Prof.Dr. TÜRKAN PATIROĞLU
Prof.Dr. TÜRKAN PATIROĞLU Kişisel Bilgiler WE-epbo:s that:t pt:u/r/[email protected]/rturkanp/ ETığpitati Yman Bdail gUizlmeranilık, Erciyes Üniversitesi, Dahili Tıp Bil., Çocuk Sağlığı ve Hastalıkları, Türkiye 1998 - 2000 Tıpta UYazmndaanll ıUkz, mEracniylıeks, EÜrnciivyerss Üitnesivi,e Drsaihteilsi iT, Dıpa Bhiilli., TÇıopc Buikl. ,S Çaoğclıuğkı vSea ğHlaığsıt avleık Hlaarsıt, aTlüıkrlkairyı,e T 1ü9r7k7iy e- 11998828 - 1989 Yİnagbiliazcnec, Bı 2D Oilrltea rÜstü Sertifika, Kurs ve Eğitimler Sağlık ve Tıp, DEsesneenyt iHala Cylvinaniclaalr Rı Kesuellaarncıhm & S eGrCtiPfi kfoars ıT, Eriracli yInevse üsntiigvaetrosritse, sIni Hveasytvigaant oDre Anceaydleermi Yye, 2re0l1 E1tik Kurulu, 2008 Yaptığı Tezler STaıpğt.Va eU Hzmsta Andlık, 1, k9r8o2nik enfeksiyonu olan hastalarda glukoz metabolizması, Erciyes Üniversitesi, Tıp Fakültesi, Çocuk ASarğalışk tBırilimmlae rAi, lTaıpn, lDaarhıili Tıp Bilimleri, Çocuk Sağlığı ve Hastalıkları, Pediatrik Hematoloji, Pediatrik İmmünoloji ve Allerji APrkoaf.Ddre.,m Erickiy Uesn Üvnaivnelrasirte /si ,G Töıpr Feavklüeltresi, Çocuk Sağ.Ve Hst Ad, 1995 - Devam Ediyor YDrodç..DDorç., .DErrc.,i yEersc iÜyensiv Üenrsiviteerssii, tTeıspi, FTaıpk üFlateksüil, tÇeosic, uÇko cSuakğ .VSaeğ H.Vset AHdst, 1A9d9, 01 9- 8179 9- 51989 Yönetilen Tezler UPAzmTIaRnOlıĞk,L CU.E TR.,K HAENM(OÖFğrİLeİn Aci )H, A20ST0A6LARINDA F8 GENİ İNT22H BÖLGESİNDEKİ İNVERSİYONUN ARAŞTIRILMASI., Tıpta DPAÜTZIERYOLĞELRUİ VTE., DTİESDSAEMVİİ NETEK İNİNTLRİAĞVİ.,A TSıKptÜaL UEzRm KaOnAlıkG,Ü ML.AKSAYROANK ÜGKELCİÜŞ(TÖİRğrİLenEcNi) H, 2A0Y0V4ANLARDA ADRENOMEDÜLLİN KPARTAINRİOAĞLL RUA TD.,Y UOZTUENR ASPÜİRNEİLNİ EYTAKŞİALYEARNİ, TLıÖpStaE MUzİLmİ aHnAlıSkT, HA.LMAeRhDmAe tE(NÖDğrOeKnRciİ)N, 2F0O0N4KSİYONLARIN DEĞERLENDİRİLMESİ SCI. I, SGSeCneI tvice A AnHalCysIi sİn odf eak Csolehroirnt eo fG 2i7re5n P aDtieerngtisl ewridthe H Yyapyeırn-IlgaEn Saynn Mdraokmaelse laenrd/or Chronic MFruecdoe cNu.,t aRnoejaosu-Rse Cstarnepdoid Ji.,a Csaisballero Garcia de Oteyza A., Buchta M., Huebscher K., Gamez-Diaz L., Proietti M., JSOaUghRaNfAi SL. -

Orphanet Report Series Rare Diseases Collection
Marche des Maladies Rares – Alliance Maladies Rares Orphanet Report Series Rare Diseases collection DecemberOctober 2013 2009 List of rare diseases and synonyms Listed in alphabetical order www.orpha.net 20102206 Rare diseases listed in alphabetical order ORPHA ORPHA ORPHA Disease name Disease name Disease name Number Number Number 289157 1-alpha-hydroxylase deficiency 309127 3-hydroxyacyl-CoA dehydrogenase 228384 5q14.3 microdeletion syndrome deficiency 293948 1p21.3 microdeletion syndrome 314655 5q31.3 microdeletion syndrome 939 3-hydroxyisobutyric aciduria 1606 1p36 deletion syndrome 228415 5q35 microduplication syndrome 2616 3M syndrome 250989 1q21.1 microdeletion syndrome 96125 6p subtelomeric deletion syndrome 2616 3-M syndrome 250994 1q21.1 microduplication syndrome 251046 6p22 microdeletion syndrome 293843 3MC syndrome 250999 1q41q42 microdeletion syndrome 96125 6p25 microdeletion syndrome 6 3-methylcrotonylglycinuria 250999 1q41-q42 microdeletion syndrome 99135 6-phosphogluconate dehydrogenase 67046 3-methylglutaconic aciduria type 1 deficiency 238769 1q44 microdeletion syndrome 111 3-methylglutaconic aciduria type 2 13 6-pyruvoyl-tetrahydropterin synthase 976 2,8 dihydroxyadenine urolithiasis deficiency 67047 3-methylglutaconic aciduria type 3 869 2A syndrome 75857 6q terminal deletion 67048 3-methylglutaconic aciduria type 4 79154 2-aminoadipic 2-oxoadipic aciduria 171829 6q16 deletion syndrome 66634 3-methylglutaconic aciduria type 5 19 2-hydroxyglutaric acidemia 251056 6q25 microdeletion syndrome 352328 3-methylglutaconic -

Practice Parameter for the Diagnosis and Management of Primary Immunodeficiency
Practice parameter Practice parameter for the diagnosis and management of primary immunodeficiency Francisco A. Bonilla, MD, PhD, David A. Khan, MD, Zuhair K. Ballas, MD, Javier Chinen, MD, PhD, Michael M. Frank, MD, Joyce T. Hsu, MD, Michael Keller, MD, Lisa J. Kobrynski, MD, Hirsh D. Komarow, MD, Bruce Mazer, MD, Robert P. Nelson, Jr, MD, Jordan S. Orange, MD, PhD, John M. Routes, MD, William T. Shearer, MD, PhD, Ricardo U. Sorensen, MD, James W. Verbsky, MD, PhD, David I. Bernstein, MD, Joann Blessing-Moore, MD, David Lang, MD, Richard A. Nicklas, MD, John Oppenheimer, MD, Jay M. Portnoy, MD, Christopher R. Randolph, MD, Diane Schuller, MD, Sheldon L. Spector, MD, Stephen Tilles, MD, Dana Wallace, MD Chief Editor: Francisco A. Bonilla, MD, PhD Co-Editor: David A. Khan, MD Members of the Joint Task Force on Practice Parameters: David I. Bernstein, MD, Joann Blessing-Moore, MD, David Khan, MD, David Lang, MD, Richard A. Nicklas, MD, John Oppenheimer, MD, Jay M. Portnoy, MD, Christopher R. Randolph, MD, Diane Schuller, MD, Sheldon L. Spector, MD, Stephen Tilles, MD, Dana Wallace, MD Primary Immunodeficiency Workgroup: Chairman: Francisco A. Bonilla, MD, PhD Members: Zuhair K. Ballas, MD, Javier Chinen, MD, PhD, Michael M. Frank, MD, Joyce T. Hsu, MD, Michael Keller, MD, Lisa J. Kobrynski, MD, Hirsh D. Komarow, MD, Bruce Mazer, MD, Robert P. Nelson, Jr, MD, Jordan S. Orange, MD, PhD, John M. Routes, MD, William T. Shearer, MD, PhD, Ricardo U. Sorensen, MD, James W. Verbsky, MD, PhD GlaxoSmithKline, Merck, and Aerocrine; has received payment for lectures from Genentech/ These parameters were developed by the Joint Task Force on Practice Parameters, representing Novartis, GlaxoSmithKline, and Merck; and has received research support from Genentech/ the American Academy of Allergy, Asthma & Immunology; the American College of Novartis and Merck. -

Novel Combined Immune Deficiency and Radiation Sensitivity Blended Phenotype in an Adult with Biallelic Variations in ZAP70 and RNF168
CASE REPORT published: 26 May 2017 doi: 10.3389/fimmu.2017.00576 Novel Combined Immune Deficiency and Radiation Sensitivity Blended Phenotype in an Adult with Biallelic Variations in ZAP70 and RNF168 Ivan K. Chinn1,2,3*†, Robert P. Sanders4†, Asbjørg Stray-Pedersen5,6,7, Zeynep H. Coban-Akdemir7,8, Vy Hong-Diep Kim9, Harjit Dadi9,10, Chaim M. Roifman9,10, Troy Quigg4, James R. Lupski1,7,8,11, Jordan S. Orange1,2,3 and I. Celine Hanson1,2 1 Department of Pediatrics, Baylor College of Medicine, Houston, TX, USA, 2 Section of Immunology, Allergy, and Rheumatology, Texas Children’s Hospital, Houston, TX, USA, 3 Center for Human Immunobiology, Texas Children’s Edited by: Hospital, Houston, TX, USA, 4 Texas Transplant Institute, Methodist Hospital, San Antonio, TX, USA, 5 Norwegian National Andrew Gennery, Unit for Newborn Screening, Department of Pediatric and Adolescent Medicine, Oslo University Hospital, Oslo, Norway, Newcastle University, UK 6 Institute of Clinical Medicine, University of Oslo, Oslo, Norway, 7 Baylor-Hopkins Center for Mendelian Genomics, Baylor College of Medicine, Houston, TX, USA, 8 Department of Molecular and Human Genetics, Baylor College of Medicine, Reviewed by: Houston, TX, USA, 9 Division of Immunology and Allergy, Department of Pediatrics, The Hospital for Sick Children, University Filomeen Haerynck, of Toronto, Toronto, ON, Canada, 10 Canadian Centre for Primary Immunodeficiency, The Jeffrey Model Research Laboratory Ghent University, Belgium for the Diagnosis of Primary Immunodeficiency, The Hospital for Sick Children, University of Toronto, Toronto, ON, Canada, Kohsuke Imai, 11 Human Genome Sequencing Center, Baylor College of Medicine, Houston, TX, USA Tokyo Medical and Dental University, Japan *Correspondence: With the advent of high-throughput genomic sequencing techniques, novel genetic Ivan K. -

Host Genetics and Infectious Disease: New Tools, Insights and Translational Opportunities
REVIEWS Host genetics and infectious disease: new tools, insights and translational opportunities Andrew J. Kwok 1, Alex Mentzer 1,2 and Julian C. Knight 1 ✉ Abstract | Understanding how human genetics influence infectious disease susceptibility offers the opportunity for new insights into pathogenesis, potential drug targets, risk stratification, response to therapy and vaccination. As new infectious diseases continue to emerge, together with growing levels of antimicrobial resistance and an increasing awareness of substantial differences between populations in genetic associations, the need for such work is expanding. In this Review, we illustrate how our understanding of the host–pathogen relationship is advancing through holistic approaches, describing current strategies to investigate the role of host genetic variation in established and emerging infections, including COVID-19, the need for wider application to diverse global populations mirroring the burden of disease, the impact of pathogen and vector genetic diversity and a broad array of immune and inflammation phenotypes that can be mapped as traits in health and disease. Insights from study of inborn errors of immunity and multi-omics profiling together with developments in analytical methods are further advancing our knowledge of this important area. Penetrance Disease syndromes caused by infectious agents have A seminal study of adoptees in the 1980s reported 1 The proportion of individuals occurred throughout the history of modern humans . increased risk of death from infectious disease in chil- with a particular genotype As a result of our continued interactions with patho- dren whose biological parents succumbed to an infec- that also has an associated gens, our genomes have been shaped through processes tious disease7, highlighting the significance of human phenotype. -

Immune Cellular Evaluation Following Newborn Screening for Severe T
In this issue: Clinical flow cytometry in 2019 This is a Platinum Open Access Journal distributed under the terms of the Creative Commons Attribution Non-Commercial License which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. Immune cellular evaluation following newborn screening for severe T and B cell lymphopenia Johannes Wolf1,2, Karolin Dahlenburg3, Stephan Borte2,4 1 Municipal Hospital St. Georg Leipzig, Academic Teaching Hospital of the University Leipzig, Department of Laboratory Medicine and Microbiology, Leipzig, Germany 2 Immuno Deficiency Center Leipzig (IDCL) at Hospital St. Georg Leipzig, Jeffrey Modell Diagnostic and Research Center for Primary Immunodeficiency Diseases, Leipzig, Germany 3 Faculty of Medicine, University Leipzig, Germany 4 Municipal Hospital St. Georg Leipzig, Academic Teaching Hospital of the University Leipzig, Department of Pediatrics, Leipzig, Germany ARTICLE INFO ABSTRACT Corresponding author: Newborn screening (NBS) for severe T and/or B cell Stephan Borte, MD, PhD Immuno Deficiency Center Leipzig (IDCL) lymphopenia to identify neonates with severe com- Hospital St. Georg Leipzig bined immunodeficiencies (SCID) or agammaglob- Delitzscher Strasse 141 ulinemia rapidly after birth has paved its way into D-04129 Leipzig clinical practice. Debate exists on the concept and Germany Phone: +49 341 909 4478 strategy for rapid verification and stratification of the E-mail: [email protected] cellular immune status of positively screened infants. We provide impulses for harmonization of flow cyto- Key words: newborn screening, T cell lymphopenia, metric approaches to allow rapid integration in the B cell lymphopenia, severe combined growing number of immunological laboratories in- immunodeficiency volved in follow-up and subdivision of SCID and non- Acknowledgement: SCID entities. -

Blueprint Genetics Severe Combined Immunodeficiency Panel
Severe Combined Immunodeficiency Panel Test code: IM0101 Is a 80 gene panel that includes assessment of non-coding variants. Is ideal for patients with a clinical suspicion of combined immunodeficiencies. The genes on this panel are included in the Primary Immunodeficiency Panel. About Severe Combined Immunodeficiency Severe combined immunedeficiencies (SCIDs) are a group of primary immunodeficiencies characterized by specific mutations in genes of T and B-lymphocyte systems and leading to little or no immune response. Different subtypes of SCIDs are characterized and subdivided by the presence of circulating T and B cells. T cells are absent or markedly decreased in the most types, but levels of B cells vary. In addition, both of these disease subgroups (T-B+ and T-B-) can occur with or without NK cells. Patients with SCID are susceptible to recurrent infections that can be fatal. The worldwide prevalence of SCID is estimated to be at least 1:100,000 births, while some genetically more homogenous populations may show markedly increased numbers. Mutations in IL2RG are the most common reason for SCIDs, explaining approximately 50% of all cases and close to 100% of X-linked cases. Availability 4 weeks Gene Set Description Genes in the Severe Combined Immunodeficiency Panel and their clinical significance Gene Associated phenotypes Inheritance ClinVar HGMD ADA Severe combined immunodeficiency due to adenosine deaminase AR 49 93 deficiency AK2 Reticular dysgenesis AR 14 17 ATM Breast cancer, Ataxia-Telangiectasia AD/AR 1047 1109 BCL11B Immunodeficiency -

Primary Immunodeficiency Diseases in Children and Adults
Primary Immunodeficiency Diseases in children and adults Microorganism Primary Immune Deficiency Diseases Disease (PID) Environment Host • Background • Approach to diagnosis of PID • Genetic diagnosis of PID • Lack of focus is good thing • Looks like duck but not a duck Primary Immunodeficiency diseases • Inherited diseases of immune system • Affect different components of the immune system • Clinically heterogeneous Why do we need to diagnose PIDs? • Collective Prevalence of high as 1 in 10000 suggesting a very high burden of disease • Often missed causing significant morbidity and mortality • Multiple family members may get affected leading to financial burden on the family and society • Early diagnosis and adequate management can lead to significant reduction in morbidity and mortality Group Category Group I Combined immunodeficiencies Group II Combined immunodeficiencies with associated or syndromic features. Group III Predominantly antibody deficiencies. Group IV Diseases of immune dysregulation. Group V Congenital defects of phagocyte number, function, or both. Group VI Defects in innate immunity. Group VII Autoinflammatory disorders. Group VIII Complement deficiencies. Group IX Phenocopies of PID • International Union of Immunological Societies (IUIS): • 354 distinct disorders • 344 different gene defects listed (Feb2017) Group I Combined immunodeficiencies Group IV Diseases of immune Group II Combined immunodeficiencies with dysregulation. associated or syndromic features. Group VII Autoinflammatory Group III Predominantly antibody disorders. -
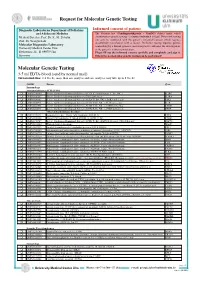
Molecular Genetic Testing
Request for Molecular Genetic Testing Diagnostic Laboratories Department of Pediatrics Informed consent of patient and Adolescent Medicine The German. law (Gendiagnostikgesetz – GenDG) defines under which Medical Director: Prof. Dr. K.-M. Debatin circumstances genetic testing of a human individual is legal. Diagnostic testing Prof. Dr. Georgia Lahr! can only be conducted with the patient’s informed consent which requires documented consultation with a doctor. Predictive testing requires genetic Molecular Diagnostics Laboratory! counselling by a human genetics specialist prior to and after the investigation, University Medical Center Ulm! or the patient’s written renunciation. Eythstrasse 24 - D-89075 Ulm Please fill out the informed consent carefully and completely and sign it. Germany Otherwise no molecular genetic testing can be performed! Molecular Genetic Testing 3-5 ml EDTA-blood (send by normal mail) Turnaround time: 2-4 weeks, more than one analysis and rare analyses may take up to 8 weeks OMIM Disease Gene Immunology Immunodeficiency SCID (T-B+) q OMIM 300400 Severe Combinined Immunodeficiency (SCID, X-chromosomal, T-, B+, NK- ) IL2RG q OMIM 606367 Severe Combinined Immunodeficiency, CD25 deficiency IL2RA q OMIM 600802 Severe Combinined Immunodeficiency (SCID, T-, B+, NK- ), JAK3 deficiency JAK3 q OMIM 608971 Severe Combinined Immunodeficiency (SCID, T- B+ NK+ ), IL7R deficiency IL7R q OMIM 608971 Severe Combinined Immunodeficiency (SCID, T- B+ NK+ ), CD3D deficiency CD3D q OMIM 608971 Severe Combinined Immunodeficiency (SCID, T- -

Pulmonary Complications of Primary Immunodeficiencies
PAEDIATRIC RESPIRATORY REVIEWS (2004) 5(Suppl A), S225–S233 Pulmonary complications of primary immunodeficiencies Rebecca H. Buckley° Departments of Pediatrics and Immunology, Duke University Medical Center, Durham, NC 27710, USA Summary In the fifty years since Ogden Bruton discovered agammaglobulinemia, more than 100 additional immunodeficiency syndromes have been described. These disorders may involve one or more components of the immune system, including T, B, and NK lymphocytes; phagocytic cells; and complement proteins. Most are recessive traits, some of which are caused by mutations in genes on the X chromosome, others in genes on autosomal chromosomes. Until the past decade, there was little insight into the fundamental problems underlying a majority of these conditions. Many of the primary immunodeficiency diseases have now been mapped to specific chromosomal locations, and the fundamental biologic errors have been identified in more than 3 dozen. Within the past decade the molecular bases of 7 X-linked immunodeficiency disorders have been reported: X-linked immunodeficiency with Hyper IgM, X-linked lymphoproliferative disease, X-linked agammaglobulinemia, X-linked severe combined immunodeficiency, the Wiskott–Aldrich syndrome, nuclear factor úB essential modulator (NEMO or IKKg), and the immune dysregulation polyendocrinopathy (IPEX) syndrome. The abnormal genes in X-linked chronic granulomatous disease (CGD) and properdin deficiency had been identified several years earlier. In addition, there are now many autosomal recessive immunodeficiencies for which the molecular bases have been discovered. These new advances will be reviewed, with particular emphasis on the pulmonary complications of some of these diseases. In some cases there are unique features of lung abnormalities in specific defects. -

Investigations on the Molecular Biology of Human Adenylate
Ulm University Medical Center Institute for Transfusion Medicine Prof. Dr. med. Hubert Schrezenmeier Investigations on the Molecular Biology of Human Adenylate Kinase 2 Deficiency (Reticular Dysgenesis) and the Establishment and Characterisation of an Adenylate Kinase 2-deficient Mouse Model Dissertation to obtain the doctoral degree of Human Biology (Dr. biol. hum.) of the Medical Faculty of Ulm University Rebekka Waldmann Ulm 2017 Amtierender Dekan: Prof. Dr. rer. nat. Thomas Wirth 1. Berichterstatter: Prof. Dr. med. Hubert Schrezenmeier 2. Berichterstatter: PD Dr. med. Manfred Hönig Tag der Promotion: 13.04.2018 Index Index INDEX OF ABBREVIATIONS ........................................................................................................................... I 1 INTRODUCTION ..................................................................................................................................... 1 1.1 SEVERE COMBINED IMMUNODEFICIENCIES (SCIDS) ........................................................................................ 1 1.2 RETICULAR DYSGENESIS ............................................................................................................................. 2 1.3 ADENYLATE KINASES ................................................................................................................................. 3 1.4 IMMUNODEFICIENT MOUSE MODELS ........................................................................................................... 7 1.5 AIM OF THE STUDY ..................................................................................................................................