University of Naples “Federico Ii”
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

IDF Patient & Family Handbook
Immune Deficiency Foundation Patient & Family Handbook for Primary Immunodeficiency Diseases This book contains general medical information which cannot be applied safely to any individual case. Medical knowledge and practice can change rapidly. Therefore, this book should not be used as a substitute for professional medical advice. FIFTH EDITION COPYRIGHT 1987, 1993, 2001, 2007, 2013 IMMUNE DEFICIENCY FOUNDATION Copyright 2013 by Immune Deficiency Foundation, USA. REPRINT 2015 Readers may redistribute this article to other individuals for non-commercial use, provided that the text, html codes, and this notice remain intact and unaltered in any way. The Immune Deficiency Foundation Patient & Family Handbook may not be resold, reprinted or redistributed for compensation of any kind without prior written permission from the Immune Deficiency Foundation. If you have any questions about permission, please contact: Immune Deficiency Foundation, 110 West Road, Suite 300, Towson, MD 21204, USA; or by telephone at 800-296-4433. Immune Deficiency Foundation Patient & Family Handbook for Primary Immunodeficency Diseases 5th Edition This publication has been made possible through a generous grant from Baxalta Incorporated Immune Deficiency Foundation 110 West Road, Suite 300 Towson, MD 21204 800-296-4433 www.primaryimmune.org [email protected] EDITORS R. Michael Blaese, MD, Executive Editor Francisco A. Bonilla, MD, PhD Immune Deficiency Foundation Boston Children’s Hospital Towson, MD Boston, MA E. Richard Stiehm, MD M. Elizabeth Younger, CPNP, PhD University of California Los Angeles Johns Hopkins Los Angeles, CA Baltimore, MD CONTRIBUTORS Mark Ballow, MD Joseph Bellanti, MD R. Michael Blaese, MD William Blouin, MSN, ARNP, CPNP State University of New York Georgetown University Hospital Immune Deficiency Foundation Miami Children’s Hospital Buffalo, NY Washington, DC Towson, MD Miami, FL Francisco A. -

Prof.Dr. TÜRKAN PATIROĞLU
Prof.Dr. TÜRKAN PATIROĞLU Kişisel Bilgiler WE-epbo:s that:t pt:u/r/[email protected]/rturkanp/ ETığpitati Yman Bdail gUizlmeranilık, Erciyes Üniversitesi, Dahili Tıp Bil., Çocuk Sağlığı ve Hastalıkları, Türkiye 1998 - 2000 Tıpta UYazmndaanll ıUkz, mEracniylıeks, EÜrnciivyerss Üitnesivi,e Drsaihteilsi iT, Dıpa Bhiilli., TÇıopc Buikl. ,S Çaoğclıuğkı vSea ğHlaığsıt avleık Hlaarsıt, aTlüıkrlkairyı,e T 1ü9r7k7iy e- 11998828 - 1989 Yİnagbiliazcnec, Bı 2D Oilrltea rÜstü Sertifika, Kurs ve Eğitimler Sağlık ve Tıp, DEsesneenyt iHala Cylvinaniclaalr Rı Kesuellaarncıhm & S eGrCtiPfi kfoars ıT, Eriracli yInevse üsntiigvaetrosritse, sIni Hveasytvigaant oDre Anceaydleermi Yye, 2re0l1 E1tik Kurulu, 2008 Yaptığı Tezler STaıpğt.Va eU Hzmsta Andlık, 1, k9r8o2nik enfeksiyonu olan hastalarda glukoz metabolizması, Erciyes Üniversitesi, Tıp Fakültesi, Çocuk ASarğalışk tBırilimmlae rAi, lTaıpn, lDaarhıili Tıp Bilimleri, Çocuk Sağlığı ve Hastalıkları, Pediatrik Hematoloji, Pediatrik İmmünoloji ve Allerji APrkoaf.Ddre.,m Erickiy Uesn Üvnaivnelrasirte /si ,G Töıpr Feavklüeltresi, Çocuk Sağ.Ve Hst Ad, 1995 - Devam Ediyor YDrodç..DDorç., .DErrc.,i yEersc iÜyensiv Üenrsiviteerssii, tTeıspi, FTaıpk üFlateksüil, tÇeosic, uÇko cSuakğ .VSaeğ H.Vset AHdst, 1A9d9, 01 9- 8179 9- 51989 Yönetilen Tezler UPAzmTIaRnOlıĞk,L CU.E TR.,K HAENM(OÖFğrİLeİn Aci )H, A20ST0A6LARINDA F8 GENİ İNT22H BÖLGESİNDEKİ İNVERSİYONUN ARAŞTIRILMASI., Tıpta DPAÜTZIERYOLĞELRUİ VTE., DTİESDSAEMVİİ NETEK İNİNTLRİAĞVİ.,A TSıKptÜaL UEzRm KaOnAlıkG,Ü ML.AKSAYROANK ÜGKELCİÜŞ(TÖİRğrİLenEcNi) H, 2A0Y0V4ANLARDA ADRENOMEDÜLLİN KPARTAINRİOAĞLL RUA TD.,Y UOZTUENR ASPÜİRNEİLNİ EYTAKŞİALYEARNİ, TLıÖpStaE MUzİLmİ aHnAlıSkT, HA.LMAeRhDmAe tE(NÖDğrOeKnRciİ)N, 2F0O0N4KSİYONLARIN DEĞERLENDİRİLMESİ SCI. I, SGSeCneI tvice A AnHalCysIi sİn odf eak Csolehroirnt eo fG 2i7re5n P aDtieerngtisl ewridthe H Yyapyeırn-IlgaEn Saynn Mdraokmaelse laenrd/or Chronic MFruecdoe cNu.,t aRnoejaosu-Rse Cstarnepdoid Ji.,a Csaisballero Garcia de Oteyza A., Buchta M., Huebscher K., Gamez-Diaz L., Proietti M., JSOaUghRaNfAi SL. -

Repercussions of Inborn Errors of Immunity on Growth☆ Jornal De Pediatria, Vol
Jornal de Pediatria ISSN: 0021-7557 ISSN: 1678-4782 Sociedade Brasileira de Pediatria Goudouris, Ekaterini Simões; Segundo, Gesmar Rodrigues Silva; Poli, Cecilia Repercussions of inborn errors of immunity on growth☆ Jornal de Pediatria, vol. 95, no. 1, Suppl., 2019, pp. S49-S58 Sociedade Brasileira de Pediatria DOI: https://doi.org/10.1016/j.jped.2018.11.006 Available in: https://www.redalyc.org/articulo.oa?id=399759353007 How to cite Complete issue Scientific Information System Redalyc More information about this article Network of Scientific Journals from Latin America and the Caribbean, Spain and Journal's webpage in redalyc.org Portugal Project academic non-profit, developed under the open access initiative J Pediatr (Rio J). 2019;95(S1):S49---S58 www.jped.com.br REVIEW ARTICLE ଝ Repercussions of inborn errors of immunity on growth a,b,∗ c,d e Ekaterini Simões Goudouris , Gesmar Rodrigues Silva Segundo , Cecilia Poli a Universidade Federal do Rio de Janeiro (UFRJ), Faculdade de Medicina, Departamento de Pediatria, Rio de Janeiro, RJ, Brazil b Universidade Federal do Rio de Janeiro (UFRJ), Instituto de Puericultura e Pediatria Martagão Gesteira (IPPMG), Curso de Especializac¸ão em Alergia e Imunologia Clínica, Rio de Janeiro, RJ, Brazil c Universidade Federal de Uberlândia (UFU), Faculdade de Medicina, Departamento de Pediatria, Uberlândia, MG, Brazil d Universidade Federal de Uberlândia (UFU), Hospital das Clínicas, Programa de Residência Médica em Alergia e Imunologia Pediátrica, Uberlândia, MG, Brazil e Universidad del Desarrollo, -

NIH Public Access Author Manuscript J Allergy Clin Immunol
NIH Public Access Author Manuscript J Allergy Clin Immunol. Author manuscript; available in PMC 2008 December 12. NIH-PA Author ManuscriptPublished NIH-PA Author Manuscript in final edited NIH-PA Author Manuscript form as: J Allergy Clin Immunol. 2007 October ; 120(4): 776±794. doi:10.1016/j.jaci.2007.08.053. The International Union of Immunological Societies (IUIS) Primary Immunodeficiency Diseases (PID) Classification Committee Raif. S. Geha, M.D., Luigi. D. Notarangelo, M.D. [Co-chairs], Jean-Laurent Casanova, M.D., Helen Chapel, M.D., Mary Ellen Conley, M.D., Alain Fischer, M.D., Lennart Hammarström, M.D., Shigeaki Nonoyama, M.D., Hans D. Ochs, M.D., Jennifer Puck, M.D., Chaim Roifman, M.D., Reinhard Seger, M.D., and Josiah Wedgwood, M.D. Abstract Primary immune deficiency diseases (PID) comprise a genetically heterogeneous group of disorders that affect distinct components of the innate and adaptive immune system, such as neutrophils, macrophages, dendritic cells, complement proteins, NK cells, as well as T and B lymphocytes. The study of these diseases has provided essential insights into the functioning of the immune system. Over 120 distinct genes have been identified, whose abnormalities account for more than 150 different forms of PID. The complexity of the genetic, immunological, and clinical features of PID has prompted the need for their classification, with the ultimate goal of facilitating diagnosis and treatment. To serve this goal, an international Committee of experts has met every two years since 1970. In its last meeting in Jackson Hole, Wyoming, United States, following three days of intense scientific presentations and discussions, the Committee has updated the classification of PID as reported in this article. -

Novel Combined Immune Deficiency and Radiation Sensitivity Blended Phenotype in an Adult with Biallelic Variations in ZAP70 and RNF168
CASE REPORT published: 26 May 2017 doi: 10.3389/fimmu.2017.00576 Novel Combined Immune Deficiency and Radiation Sensitivity Blended Phenotype in an Adult with Biallelic Variations in ZAP70 and RNF168 Ivan K. Chinn1,2,3*†, Robert P. Sanders4†, Asbjørg Stray-Pedersen5,6,7, Zeynep H. Coban-Akdemir7,8, Vy Hong-Diep Kim9, Harjit Dadi9,10, Chaim M. Roifman9,10, Troy Quigg4, James R. Lupski1,7,8,11, Jordan S. Orange1,2,3 and I. Celine Hanson1,2 1 Department of Pediatrics, Baylor College of Medicine, Houston, TX, USA, 2 Section of Immunology, Allergy, and Rheumatology, Texas Children’s Hospital, Houston, TX, USA, 3 Center for Human Immunobiology, Texas Children’s Edited by: Hospital, Houston, TX, USA, 4 Texas Transplant Institute, Methodist Hospital, San Antonio, TX, USA, 5 Norwegian National Andrew Gennery, Unit for Newborn Screening, Department of Pediatric and Adolescent Medicine, Oslo University Hospital, Oslo, Norway, Newcastle University, UK 6 Institute of Clinical Medicine, University of Oslo, Oslo, Norway, 7 Baylor-Hopkins Center for Mendelian Genomics, Baylor College of Medicine, Houston, TX, USA, 8 Department of Molecular and Human Genetics, Baylor College of Medicine, Reviewed by: Houston, TX, USA, 9 Division of Immunology and Allergy, Department of Pediatrics, The Hospital for Sick Children, University Filomeen Haerynck, of Toronto, Toronto, ON, Canada, 10 Canadian Centre for Primary Immunodeficiency, The Jeffrey Model Research Laboratory Ghent University, Belgium for the Diagnosis of Primary Immunodeficiency, The Hospital for Sick Children, University of Toronto, Toronto, ON, Canada, Kohsuke Imai, 11 Human Genome Sequencing Center, Baylor College of Medicine, Houston, TX, USA Tokyo Medical and Dental University, Japan *Correspondence: With the advent of high-throughput genomic sequencing techniques, novel genetic Ivan K. -

Host Genetics and Infectious Disease: New Tools, Insights and Translational Opportunities
REVIEWS Host genetics and infectious disease: new tools, insights and translational opportunities Andrew J. Kwok 1, Alex Mentzer 1,2 and Julian C. Knight 1 ✉ Abstract | Understanding how human genetics influence infectious disease susceptibility offers the opportunity for new insights into pathogenesis, potential drug targets, risk stratification, response to therapy and vaccination. As new infectious diseases continue to emerge, together with growing levels of antimicrobial resistance and an increasing awareness of substantial differences between populations in genetic associations, the need for such work is expanding. In this Review, we illustrate how our understanding of the host–pathogen relationship is advancing through holistic approaches, describing current strategies to investigate the role of host genetic variation in established and emerging infections, including COVID-19, the need for wider application to diverse global populations mirroring the burden of disease, the impact of pathogen and vector genetic diversity and a broad array of immune and inflammation phenotypes that can be mapped as traits in health and disease. Insights from study of inborn errors of immunity and multi-omics profiling together with developments in analytical methods are further advancing our knowledge of this important area. Penetrance Disease syndromes caused by infectious agents have A seminal study of adoptees in the 1980s reported 1 The proportion of individuals occurred throughout the history of modern humans . increased risk of death from infectious disease in chil- with a particular genotype As a result of our continued interactions with patho- dren whose biological parents succumbed to an infec- that also has an associated gens, our genomes have been shaped through processes tious disease7, highlighting the significance of human phenotype. -

Primary Immunodeficiency Diseases in Children and Adults
Primary Immunodeficiency Diseases in children and adults Microorganism Primary Immune Deficiency Diseases Disease (PID) Environment Host • Background • Approach to diagnosis of PID • Genetic diagnosis of PID • Lack of focus is good thing • Looks like duck but not a duck Primary Immunodeficiency diseases • Inherited diseases of immune system • Affect different components of the immune system • Clinically heterogeneous Why do we need to diagnose PIDs? • Collective Prevalence of high as 1 in 10000 suggesting a very high burden of disease • Often missed causing significant morbidity and mortality • Multiple family members may get affected leading to financial burden on the family and society • Early diagnosis and adequate management can lead to significant reduction in morbidity and mortality Group Category Group I Combined immunodeficiencies Group II Combined immunodeficiencies with associated or syndromic features. Group III Predominantly antibody deficiencies. Group IV Diseases of immune dysregulation. Group V Congenital defects of phagocyte number, function, or both. Group VI Defects in innate immunity. Group VII Autoinflammatory disorders. Group VIII Complement deficiencies. Group IX Phenocopies of PID • International Union of Immunological Societies (IUIS): • 354 distinct disorders • 344 different gene defects listed (Feb2017) Group I Combined immunodeficiencies Group IV Diseases of immune Group II Combined immunodeficiencies with dysregulation. associated or syndromic features. Group VII Autoinflammatory Group III Predominantly antibody disorders. -
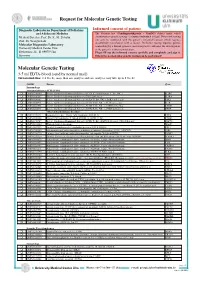
Molecular Genetic Testing
Request for Molecular Genetic Testing Diagnostic Laboratories Department of Pediatrics Informed consent of patient and Adolescent Medicine The German. law (Gendiagnostikgesetz – GenDG) defines under which Medical Director: Prof. Dr. K.-M. Debatin circumstances genetic testing of a human individual is legal. Diagnostic testing Prof. Dr. Georgia Lahr! can only be conducted with the patient’s informed consent which requires documented consultation with a doctor. Predictive testing requires genetic Molecular Diagnostics Laboratory! counselling by a human genetics specialist prior to and after the investigation, University Medical Center Ulm! or the patient’s written renunciation. Eythstrasse 24 - D-89075 Ulm Please fill out the informed consent carefully and completely and sign it. Germany Otherwise no molecular genetic testing can be performed! Molecular Genetic Testing 3-5 ml EDTA-blood (send by normal mail) Turnaround time: 2-4 weeks, more than one analysis and rare analyses may take up to 8 weeks OMIM Disease Gene Immunology Immunodeficiency SCID (T-B+) q OMIM 300400 Severe Combinined Immunodeficiency (SCID, X-chromosomal, T-, B+, NK- ) IL2RG q OMIM 606367 Severe Combinined Immunodeficiency, CD25 deficiency IL2RA q OMIM 600802 Severe Combinined Immunodeficiency (SCID, T-, B+, NK- ), JAK3 deficiency JAK3 q OMIM 608971 Severe Combinined Immunodeficiency (SCID, T- B+ NK+ ), IL7R deficiency IL7R q OMIM 608971 Severe Combinined Immunodeficiency (SCID, T- B+ NK+ ), CD3D deficiency CD3D q OMIM 608971 Severe Combinined Immunodeficiency (SCID, T- -

Pulmonary Complications of Primary Immunodeficiencies
PAEDIATRIC RESPIRATORY REVIEWS (2004) 5(Suppl A), S225–S233 Pulmonary complications of primary immunodeficiencies Rebecca H. Buckley° Departments of Pediatrics and Immunology, Duke University Medical Center, Durham, NC 27710, USA Summary In the fifty years since Ogden Bruton discovered agammaglobulinemia, more than 100 additional immunodeficiency syndromes have been described. These disorders may involve one or more components of the immune system, including T, B, and NK lymphocytes; phagocytic cells; and complement proteins. Most are recessive traits, some of which are caused by mutations in genes on the X chromosome, others in genes on autosomal chromosomes. Until the past decade, there was little insight into the fundamental problems underlying a majority of these conditions. Many of the primary immunodeficiency diseases have now been mapped to specific chromosomal locations, and the fundamental biologic errors have been identified in more than 3 dozen. Within the past decade the molecular bases of 7 X-linked immunodeficiency disorders have been reported: X-linked immunodeficiency with Hyper IgM, X-linked lymphoproliferative disease, X-linked agammaglobulinemia, X-linked severe combined immunodeficiency, the Wiskott–Aldrich syndrome, nuclear factor úB essential modulator (NEMO or IKKg), and the immune dysregulation polyendocrinopathy (IPEX) syndrome. The abnormal genes in X-linked chronic granulomatous disease (CGD) and properdin deficiency had been identified several years earlier. In addition, there are now many autosomal recessive immunodeficiencies for which the molecular bases have been discovered. These new advances will be reviewed, with particular emphasis on the pulmonary complications of some of these diseases. In some cases there are unique features of lung abnormalities in specific defects. -

Kinase Inhibitors in the Treatment of Immune-Mediated Disease Apostolos Kontzias1, Arian Laurence1, Massimo Gadina2 and John J
Published: 01 March 2012 © 2012 Faculty of 1000 Ltd Kinase inhibitors in the treatment of immune-mediated disease Apostolos Kontzias1, Arian Laurence1, Massimo Gadina2 and John J. O’Shea1* Addresses: 1Molecular Immunology and Inflammation Branch, National Institute of Arthritis and Musculoskeletal and Skin Diseases, National Institutes of Health, Bethesda, MD 20892, USA; 2Translational Immunology Section, Office of Science and Technology, National Institute of Arthritis and Musculoskeletal and Skin Diseases, National Institutes of Health, Bethesda, MD 20892, USA * Corresponding author: John J. O’Shea ([email protected]) F1000 Medicine Reports 2012, 4:5 (doi:10.3410/M4-5) This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial License (http://creativecommons.org/licenses/by-nc/3.0/legalcode), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. You may not use this work for commercial purposes. The electronic version of this article is the complete one and can be found at: http://f1000.com/reports/m/4/5 Abstract Protein kinases are fundamental components of diverse signaling pathways, including immune cells. Their essential functions have made them effective therapeutic targets. Initially, the expectation was that a high degree of selectivity would be critical; however, with time, the use of “multikinase” inhibitors has expanded. Moreover, the spectrum of diseases in which kinase inhibitors are used has also expanded to include not only malignancies but also immune-mediated diseases. At present, thirteen kinase inhibitors have been approved in the United States, all for oncologic indications. However, there are a growing number of molecules, including several Janus kinase inhibitors, that are being tested in clinical trials for autoimmune diseases such as rheumatoid arthritis, psoriasis and inflammatory bowel diseases. -

J Recombination and Nonhomologous DNA End Joining
Functional redundancy between the XLF and DNA-PKcs DNA repair factors in V(D)J recombination and nonhomologous DNA end joining Valentyn Oksenycha,b,c, Vipul Kumara,b,c, Xiangyu Liud, Chunguang Guoa,b,c, Bjoern Schwera,b,c, Shan Zhad, and Frederick W. Alta,b,c,1 aHoward Hughes Medical Institute, bProgram in Cellular and Molecular Medicine, Boston Children’s Hospital, and cDepartment of Genetics, Harvard Medical School, Boston, MA 02115; and dInstitute for Cancer Genetics, Department of Pathology and Cell Biology and Department of Pediatrics, College of Physicians and Surgeons, Columbia University, New York, NY 10032 Contributed by Frederick W. Alt, December 26, 2012 (sent for review December 18, 2012) Classical nonhomologous end joining (C-NHEJ) is a major mamma- J coding segments are each flanked by RSs that target RAG. RAG lian DNA double-strand break (DSB) repair pathway that is required cleaves between the borders of two appropriately paired coding for assembly of antigen receptor variable region gene segments by segments and their flanking recombination signal sequences (RSs) V(D)J recombination. Recombination activating gene endonuclease to generate two hairpin-sealed coding ends (CEs) and two blunt 5′- initiates V(D)J recombination by generating DSBs between two V phosphorylated RS ends (SEs). The SEs are ligated back together (D)J coding gene segments and flanking recombination signal without further processing, whereas the coding ends must be sequences (RS), with the two coding ends and two RS ends joined opened and processed before they can be joined. Both CE and SE by C-NHEJ to form coding joins and signal joins, respectively. -

Prof. TÜRKAN PATIROĞLU
Prof. TÜRKAN PATIROĞLU Personal Information WEmeabi:l :h tutpr:k/a/[email protected]/turkanp/ EPodsut Dcaocttioornat eIn off oMremdiacitnieo, nErciyes Üniversitesi, Dahili Tıp Bil., Çocuk Sağlığı ve Hastalıkları, Turkey 1998 - 2000 EPxopste rDtoiscet oInra Mtee odfic Mineed, iEcrinciey, eEsr Ücinyievse Ürsnitiveesir, sDitaehsii,l iD Taıph iBli iTl.,ı pÇ oBcilu.,k Ç Soacğulkığ Sı avğel ıHğıa vstea Hlıkalsatraıl, ıTkluarrkı,e Tyu 1r9k7ey7 1- 918988 2- 1989 FEnogrliesihg, nB2 L Uapnpgeru Iangteersmediate Certificates, Courses and Trainings Health&Medicine, DEsesneenyt iHala Cylvinaniclaalr Rı Kesuellaarncıhm & S eGrCtiPfi kfoars ıT, Eriracli yInevse üsntiigvaetrosritse, sIni Hveasytvigaant oDre Anceaydleermi Yye, 2re0l1 E1tik Kurulu, 2008 Dissertations ÇEoxpcuekrt Sisaeğ I.Vne M Hesdti cAidn,e 1, k9r8o2nik enfeksiyonu olan hastalarda glukoz metabolizması, Erciyes Üniversitesi, Tıp Fakültesi, Research Areas IHmemaluthn oScloiegnyc aens,d M Aelldeircginye, Internal Medicine Sciences, Child Health and Diseases, Pediatric Hematology, Pediatric APrcoafedsesomr,i Ecr Tciyitelse Üsn /iv eTrasistekssi, Tıp Fakültesi, Çocuk Sağ.Ve Hst Ad, 1995 - Continues Assiosctaiantte PPrrooffeessssoorr, , EErrcciiyyeess ÜÜnniivveerrssiitteessii, , TTııpp FFaakküülltteessii, , ÇÇooccuukk SSaağğ.V.Vee HHsstt AAdd, , 11998970 -- 11998995 APAdTvIRisOiĞnLgU TT.h, HeEsMesOFİLİ A HASTALARINDA F8 GENİ İNT22H BÖLGESİNDEKİ İNVERSİYONUN ARAŞTIRILMASI., PEAxpTeIRrtOisĞeL IUn TM.,e DdİiSciSnEeM, CİN.EER KİNATNR(ASVtuAdSeKnÜt)L, E2R0 0K6OAGÜLASYON GELİŞTİRİLEN HAYVANLARDA ADRENOMEDÜLLİN DÜZEYLERİ VE TEDAVİ ETKİNLİĞİ., Expertise In Medicine, M.KARAKÜKCÜ(Student), 2004 KPARTAINRİOAĞLL RUA TD.,Y UOZTUENR ASPÜİRNEİLNİ EYTAKŞİALYEARNİ, ELxÖpSeErMtiİsLeİ IHn AMSeTdAiLciAnRe,D HA.M EeNhDmOeKtR(SİNtu dFeOnNtK),S 2İY0O04NLARIN DEĞERLENDİRİLMESİ Articles Published in Journals That Entered SCI, SSCI and AHCI Indexes I. MGeunceotciuc tAanaeloyussis C oafn ad iCdoiahsoisrt of 275 Patients with Hyper-IgE Syndromes and/or Chronic SFargehdaef Ni S.,. ,R Cohjasv-oRsehsztardepeho ZJ.,.