Annual Report 2018 - 2019
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Immigration Matters
ISSUE 8 • MAY 2008 Immigration Matters C A I I • THE CHURCHES’ AGENCY ON INTERNATIONAL ISSUES: RESOURCING CHURCHES AND CONGREGATIONS ON GLOBAL CONCERNS Seeking Refuge in a Strange Land – the experiences of refugees and asylum seekers hroughout history innocent people cleansing and crimes against humanity. Nicholson have been forced from their homes The Responsibility to Protect is becoming Tto seek safety and refuge in the an important issue for collective face of violence. Despite the United discussion and action when states and Nations (UN) agreeing in 1951 to the the international community have failed Convention relating to the Status of to prevent catastrophe. Refugees, civilians continue to be The United Nations High Commission for caught up in horrifying wars, whole Refugees (UNHCR) currently recognises communities are displaced within their some 14 million refugees. In addition, own countries and many live or are an estimated 24.5 million people are “warehoused” in makeshift refugee displaced within their own countries. camps relying on humanitarian aid With the large numbers of displaced for their very survival. Displacement people and increasing insecurity, there has become a strategy of war. Some, is a lot of pressure on governments, the especially those with more resources, international community, the churches, have sought refuge in developed and concerned people to uphold the countries but many more have entered Responsibility to Protect. Facing these neighbouring developing countries where challenges as a faith community is part often they are competing for limited of the continuing Christian commitment resources with those living in the host to help those made vulnerable by country. -

Wellington Town Belt Management Plan – June 2013 49
6 Recreation The play area at Central Park, Brooklyn. A flying fox and bike skills area are also provided. Guiding principles The Town Belt is for all to enjoy. This concerns equity of access and use of the Town Belt. The Council believes that the Town Belt should be available for all Wellingtonians to enjoy. The Council is committed to ensuring that the Town Belt will continue to be improved with more access and improved accessibly features where it is reasonably practicable to do so. The Town Belt will be used for a wide range of recreation activities. The Town Belt should cater for a wide range of sporting and recreation activities managed in a way to minimise conflict between different users. Co-location and intensification of sports facilities within existing hubs and buildings is supported where appropriate. 6.1 Objectives 6.1.1 The Town Belt is accessed and used by the community for a wide range of sporting and recreational activities. 6.1.2 Recreational and sporting activities are environmentally, financially and socially sustainable. 6.1.3 Participation in sport and recreation is encouraged and supported. 6.1.4 The Town Belt makes a significant contribution to the quality of life, health and wellbeing of Wellingtonians by increasing a range of physical activity and providing active transport routes and access to natural environments 6.1.5 The track (open-space access) network provides for a range of user interests, skills, abilities and fitness levels, and pedestrian and cycling commuter links. 6.1.6 Management and development of formal sporting facilities and associated infrastructure does not compromise the landscape and ecological values of the Town Belt. -

21. Rights of Refugees Tikanga O Ngä Tängata Rerenga
336 SEctioN Four – Rights oF SpEcific groUpS 21. Rights of Refugees Tikanga o ngä Tängata Rerenga “Everyone has the right to go to another country and ask forprotection if they are being mistreated or are in danger.” HUMAN RIGHTS IN NEW ZEALAND 2010 337 Everyone has the right to go to another unable or, owing to such fear, is unwilling to country and ask for protection if they avail himself of the protection of that country; are being mistreated or are in danger. or who, not having a nationality and being Universal Declaration of Human Rights, Article 14 outside the country of his former habitual residence as a result of such events, is unable or, owing to such fear, is unwilling to return Introduction to it. Timatatanga In the New Zealand context, refugees fall into a number The human rights of refugees are specified in the 1951 of categories: quota or mandated refugees, spontaneous United Nations Convention Relating to the Status of refugees or asylum seekers, and family members of Refugees (the Refugee Convention) and its 1967 protocol. refugees resident in New Zealand. Spontaneous refugees The International Covenant on Civil and Political Rights are people who claim refugee status on arriving at the (ICCPR) and the Convention Against Torture and Other border or after entering New Zealand. Typically, people Cruel, Inhumane or Degrading Treatment or Punishment in this situation arrive without papers, or claim refugee 1984 (CAT) also contain provisions relevant to refugees. status before or after the expiry of a temporary permit. New Zealand has ratified all three treaties and they They can be divided into those awaiting a decision on are reflected in a variety of domestic legislation. -
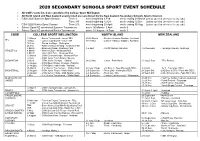
2020 Secondary Schools Sport Event Schedule
2020 SECONDARY SCHOOLS SPORT EVENT SCHEDULE All CSW events listed are sanctioned by College Sport Wellington All North Island and New Zealand events listed are sanctioned by the New Zealand Secondary Schools Sports Council. CSW 2020 Summer Sport Season: Term 1: week beginning 3 Feb week ending 29 March [unless specified otherwise for any code] Term 3/4: week beginning 12 Oct week ending 12 Dec [unless specified otherwise for any code] CSW 2020 Winter Sport Season: Term 2/3: week beginning 28 April week ending 30 Aug [unless specified otherwise for any code] School Sport NZ sanctioned Summer Tournament week: 30 March - 3 April week 9 School Sport NZ sanctioned Winter Tournament week: 31 August - 4 Sept week 7 CODE COLLEGE SPORT WELLINGTON NORTH ISLAND NEW ZEALAND 19 March - Senior Tournament - venue TBA 25-26 March - Seniors -Harbour Stadium, Auckland AFL 10 Nov - Junior Tournament - venue TBA 18-19 Nov - Juniors -Harbour Stadium, Auckland 16 Feb - Round the Bays - Wellington 25 Feb - AWD selection Meeting - Newtown Park 3 March - McEvedy Shield - Newtown Park 3-5 April - Porritt Stadium, Hamilton 4-6 December - Tauranga Domain, Tauranga ATHLETICS 4 March - Western Zone - Newtown Park 5 March - Hutt / Girls Zone - Newtown Park 12 March - CSW Championships - Newtown Park 23 July - CSW Junior Team Finals - Naenae BADMINTON 29 July - CSW Junior Champs - Haitaitai 24-26 Nov - Junior - Palm North 31 Aug-3 Sept - TRA, Porirua 12 August - CSW Open Singles Champs - Haitaitai 21 August - CSW Open Team Finals - Haitaitai 26 March - 3 x 3 Senior -

Shifting Consciousness About Refugees in New Zealand
“GIMME SHELTER”: SHIFTING CONSCIOUSNESS ABOUT REFUGEES IN NEW ZEALAND GLOBAL MIGRATION: FEBRUARY20-22, 2018 DR. ELENA KOLESOVA & PROF. MATT ALLEN Source: Stuff, 2015 QUESTIONS TO CONSIDER How refugees are constructed in New Zealand through history and the present ? ‘Gimme Shelter’ – Shifting consciousness about refugees in New Zealand What is the role of ‘othering’ in constructing refugees? How does Edward Said’s Orientalism speak to the notion of ‘othering’ in the current context? Source: The Daily Blog, 2015 New Zealand is a ‘settler’ nation populated by ‘boat people’ The three stages of immigration to New Zealand according to Spoonley and Bedford (2012, p.51-52) •The first spans the period from 1840 to 1960 – From the signing of the Treaty of Waitangi that confirmed the status of New Zealand as a British colony, immigration policies reflected the ambition of recreating a country that embodied what were seen as the virtues of Britain and of being British. the 2nd phase •The second phase, from about 1950s/1960s to the 1980s, produced a new set of ambitions. The nation as a single community and a colony of the British crown was challenged, with greater recognition of Māori and their rights. During this phase a Labour Prime Minister in the 1970s, Norman Kirk, identified the importance of building our Asia-Pacific connections. This led to a more lenient immigration policy for Pacific nations annexed as colonies of the British government then taken over by New Zealand, such as the Cook Islands, Samoa, Niue and Tokelau. the 3rd phase •The third phase was marked by major changes to immigration policy from 1986. -

Relations and Relationships: 40 Years of People Movements from ASEAN Countries to New Zealand R
1 Relations and Relationships: 40 years of people movements from ASEAN countries to New Zealand R Report Research Relations and Relationships: 40 years of people movements from ASEAN countries to New Zealand Author Kate McMillan June 2016 ISBN: 978-0-9941233-2-9 (PDF) © Asia New Zealand Foundation Disclaimer: Comments made in this research report do not necessarily represent the views of the Asia New Zealand Foundation 02 Relations and Relationships: 40 years of people movements from ASEAN countries to New Zealand Contents 03 About the author 04 Introduction 06 New Zealand-ASEAN relations and people movements: A background 10 Students from ASEAN countries 18 Migrants from ASEAN countries 32 Irregular migration from ASEAN countries 35 Tourists and other short- term visitors from ASEAN countries 41 Looking ahead 44 Conclusion 03 Relations and Relationships: 40 years of people movements from ASEAN countries to New Zealand About the author Dr Kate McMillan is a Senior Lecturer in Comparative Politics at Victoria University of Wellington. Her research and teaching interests focus on immigration, citizenship and media politics. Kate has published numerous articles and book chapters on New Zealand’s immigration policy, New Zealand’s Australian diaspora, the role of the news media in New Zealand politics, the representation of women in the New Zealand news media, and immigrants’ voting rights and electoral participation in New Zealand. Current research projects focus on the electoral participation of Asian immigrants in New Zealand, and the future of human mobility arrangements such as the Trans-Tasman Travel Arrangement. In 2012 Kate was awarded a Knowledge and Expertise Exchange Europe-New Zealand Fellowship to Lund University, Sweden. -

Section Ii: Other Items
SECTION II: OTHER ITEMS II.i Contents of Miscellaneous Folders II.i.a Britain: Miscellaneous Folder B.E England B.E40 “Society of Brushmakers’ Descendants, Members’ Interest Names, 1997”. B.E39 “How names are in our genes” Observer, Feb. 2001. B.E38 “Update on Places in London [central] Where Records are Located” from Richard Moore. Also “English Poor Laws”, brief notes (incl. list of recommended reading) from Marjorie R. Moore, Jul 2000. 2 pp. B.E37 Family Records, Centre, 1 Myddelton St, London (flyer) B.E36 NORCAP News no.53, 1998 (Nat.Org.for Counselling of Adoptees & Parents) B.E35 Access to Birth Records: counselling organisations outside the United Kingdom; and Access to Birth Records: Information for adopted people living outside the United Kingdom, Office of National Statistics B.E34 Addresses for Genealogical Research in Great Britain & Eire B.E33 Roll of Battle Abbey, A.D. 1066 B.E32 “The modern way to trace your family tree”, from Woman’s Weekly, 1999. B.E31 Review of Anthony Camp talk on occupations in towns, with extensive bibliography B.E30 St Catherines House Indexes - volume nos. by counties, 1992 B.E29 Record repositories, extract from Family Tree Magazine 1996 B.E28 Extract from London Street Directory 1852, & 1854 (2 pp only) B.E27 The modern British army cap badge: a brief guide as to how it evolved, compiled by John McConaghy. 9 pp. B.E26 Research material available to the genealogist in the UK & Europe B.E25 British & Irish Biographies 1840-1940, review B.E24 Barnardo’s: information for enquirers B.E23 Manorial documents register B.E22 “Cave man added to family tree”, cutting 1997 B.E21 Ministry of Defence: application for information from army service records, 1994 B.E20 What to do with the body: some Victorian solutions, extract from Family Tree Magazine, 1995 B.E19 Soldiers: snippets from Peoples England. -

Quarterly Report
1. GOVERNANCE Pārongo ā-Tāone We want to maintain confidence in our decision-making. We have an obligation to ensure the views of Māori and mana whenua are heard. WHAT WE DO • Governance, information and engagement • Māori and mana whenua partnerships. HIGHLIGHTS OF THIS QUARTER • We equipped the council meetings rooms to enable elected members and the public to participate remotely in meetings via audio and audio-visual links. • We interacted with over 78,000 customers through the Contact Centre. • We co-hosted with Port Nicholson Block Settlement Trust, the Waitangi Day celebrations at Waitangi Park. • The Mayor selected her Tuia Rangatahi (Young Māori Leadership Development Programme) representative - Māia Huriwaka, a Year 13 student nominated by Wellington East Girls College. • 11 March – we sponsored Te Rā Haka where 400 college students from across the region came together at ASB Sports Centre to learn local haka. • 15 March – we sponsored Te Rā o Kupe, which was hosted by The Kupe Charitable Trust, recognising local Māori music and food. SIGNIFICANT VARIANCES TO PERFORMANCE1: SERVICE DELIVERY Measure Actual Target Var Variance explanation Council, committee and 61% 80% (24%) Over 80% of agendas were with the elected members five days subcommittee reports that are made before meeting and in the public domain four days before the available to the public five days prior meeting. We continue to achieve 100% for our statutory target to to the meeting (%) make reports available to the public two days prior to meetings. NET OPERATING EXPENDITURE YTD Full Year Activity Actual Budget Variance Forecast Budget $000 $000 $000 $000 $000 1.1 Governance, Information & Engagement 10,444 10,669 224 14,057 14,213 1.2 Māori Engagement (mana whenua) 99 169 70 225 225 Year to date variance is due to timing of MOU payments. -

The Vietnam War
Fact Sheet 1: Introduction- the Vietnam War Between June 1964 and December 1972 around 3500 New Zealand service personnel served in South Vietnam. Unlike the First and Second World Wars New Zealand’s contribution in terms of personnel was not huge. At its peak in 1968 the New Zealand force only numbered 543. Thirty-seven died while on active service and 187 were wounded. The Vietnam War – sometimes referred to as the Second Indochina War – lasted from 1959 to 1975. In Vietnam it is referred to as the American War. It was fought between the communist Democratic Republic of Vietnam (North Vietnam) and its allies, and the US-supported Republic of Vietnam in the south. It ended with the defeat of South Vietnam in April 1975. Nearly 1.5 million military personnel were killed in the war, and it is estimated that up to 2 million civilians also died. This was the first war in which New Zealand did not fight with its traditional ally, Great Britain. Our participation reflected this country’s increasingly strong defence ties with the United States and Australia. New Zealand’s involvement in Vietnam was highly controversial and attracted protest and condemnation at home and abroad. A study of New Zealand’s involvement in the Vietnam War raises a number of issues. As a historical study we want to find out what happened, why it happened and how it affected people’s lives. This war meant different things to different people. The Vietnam War was, and still is, an important part of the lives of many New Zealanders. -

Sustainable Transport Committee 5 December 2018, Order Paper - Front Page
Sustainable Transport Committee 5 December 2018, Order Paper - Front Page If calling please ask for: Democratic Services 30 November 2018 Sustainable Transport Committee Order Paper for the meeting of the Sustainable Transport Committee to be held in the Council Chamber, Greater Wellington Regional Council, Level 2, 15 Walter Street, Te Aro, Wellington Wednesday, 5 December 2018 at 9.30am Membership Cr Donaldson (Chair) Cr Ponter (Deputy Chair) Cr Blakeley Cr Brash Cr Gaylor Cr Kedgley Cr Laban Cr Laidlaw Cr Lamason Cr McKinnon Cr Ogden Cr Staples Cr Swain Marama Tuuta Recommendations in reports are not to be construed as Council policy until adopted by Council 1 Sustainable Transport Committee 5 December 2018, Order Paper - Agenda Sustainable Transport Committee Order Paper for the meeting to be held on Wednesday, 5 December 2018 in the Council Chamber, Greater Wellington Regional Council, Level 2, 15 Walter Street, Te Aro, Wellington at 9.30am Public Business Page No. 1. Apologies 2. Declarations of conflict of interest 3. Public participation 4. Confirmation of the Public minutes of 30 October Report 18.517 3 2018 5. Action items from previous Sustainable Transport Report 18.529 11 Committee meetings 6. Implementation of new Wellington bus network – Report 18.526 14 December update 7. General Managers' report to the Sustainable Report 18.525 50 Transport Committee meeting on 5 December 2018 8. Exclusion of the public Report 18.575 56 Public Excluded Business 9. Confirmation of the Public Excluded minutes of Report PE18.518 57 30 October -

Soldiers and School Children Military Performances and National Identity During the Prince of Wales’ 1920 Visit to Wellington
UHPH_14: Landscapes and ecologies of urban and planning history | 463 Soldiers and School Children Military performances and national identity during the Prince of Wales’ 1920 visit to Wellington Christopher McDonald Victoria University of Wellington/University of New South Wales [email protected] Early royal visits to New Zealand were episodes of intense symbolic activity played out on an urban scale. These events are generally understood as affirmations of British identity. However, this paper shows how the Prince of Wales’ 1920 tour of New Zealand was also used to promote the distinct character of the young dominion. The research examines two military performances in Wellington: a review at Newtown Park and a quasi-military parade of school children in parliament grounds. Analysis of these events reveals dual narratives in which New Zealanders both reaffirm their links with the Motherland and acknowledge their own difference. The two sources of identity are found to be compatible but dependent on malleable images. The paper argues that military images and narratives were flexible enough to convey New Zealanders’ “imperial” and “national” allegiances. However, while a dual narrative operated successfully during the “Children’s Day” display, the more conventional military review at Newtown Park failed because it was unable to reconcile the antipodean traits of discipline and vigour. Both performances required a degree of improvisation because Wellington lacked dedicated sites for military ceremonial. The choice of venues contributed to the disparate outcomes of the two events. In parliament grounds, school groups exhibited the health and dynamism of New Zealand’s youth but also reinforced the latent order and unity of New Zealand’s pre-eminent “national” space. -

Unclaimed Capital Credits If Your Name Appears on This List, You May Be Eligible for a Refund
Unclaimed Capital Credits If your name appears on this list, you may be eligible for a refund. Complete a Capital Credits Request Form and return it to TCEC. 0'GRADY JAMES ABERNATHY RENETHA A ADAIR ANDY 2 C INVESTMENT ABETE LILLIE ADAIR CURTIS 2 GIRLS AND A COF FEE ABEYTA EUSEBIO ADAIR KATHLEEN SHOP ABEYTA SAM ADAIR LEANARD 21 DIESEL SERVICE ABLA RANDALL ADAIR SHAYLIN 4 RED CATTLE CO ABODE CONSTRUCTIO N ADAME FERNAND 5 C FARMS ABRAHA EDEN M ADAMS & FIELD 54 DINER ABRAHAM RAMPHIS ADAMS ALFRED 54 TOWING & RECOV ERY ABREM TERRY ADAMS ALVIN A & C FEED STORE ABSOLUTE ENDEAVORS INC ADAMS ALVIN L A & I SKYLINE ROO FING ACEVEDO ARNALDO ADAMS ASHLEY A & M CONSTRUCTIO N CO ACEVEDO DELFINA A ADAMS BAPTIST CHURCH A & S FARMS ACEVEDO LEONARD ADAMS CHARLES G A C CROSSLEY MOTE L ACKER EARL ADAMS DARREL A W H ON CO ACKER LLOYD ADAMS DAVID A WILD HAIR ACKER NELDA ADAMS DELBERT AARON KENNETH ACKERMAN AMIRAH ADAMS DIANE M ABADI TEAME ACKERS MELVIN D ADAMS DORIS ABARE JASMINE ACOSTA ARMANDO ADAMS DOYLE G ABARE KALYN ACOSTA CESAR ADAMS FERTILIZER ABAYNEH SOLOMON ACOSTA FERNANDO ADAMS GARY ABB RANDALL CORPO RATION ACOSTA GARCIA R ADAMS HALEY D ABBOTT CLYDE ACOSTA GILBERTO E ADAMS HEATHER ABBOTT CLYDE V ACOSTA JOE ADAMS JEROD ABBOTT FLOYD K ACOSTA JOSE A ADAMS JERRY ABBOTT MAUREAN ACOSTA MARIA ADAMS JILL M ABBOTT ROBERT ACOSTA VICTOR ADAMS JOHN ABBOTT SCOTTY ACTION REALTY ADAMS JOHNNY ACTON PAM ADAMS LINDA Current as of February 2021 Page 1 of 190 Unclaimed Capital Credits If your name appears on this list, you may be eligible for a refund.