Emergency Department Core Competencies, Skills Checklist, and Development Tool Updated September 2015
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Emergency Care
P: Emergency Care Saskatchewan Association of Licensed Practical Nurses, Competency Profile for LPNs, 3rd Ed. 141 Major Competency Area: P Emergency Care Competency: P-1 Date: January 16, 2017 Emergency Nursing **LPNs will not independently triage/Canadian Triage Assessment Scale (CTAS) patients, this process must be done in collaboration with the inter-professional team** A Licensed Practical Nurse will: P-1-1 Demonstrate knowledge and ability to apply critical thinking and critical inquiry throughout the nursing process in emergency nursing. P-1-2 Demonstrate knowledge and ability to perform a comprehensive health assessment. P-1-3 Demonstrate knowledge and ability to perform nursing procedures and interventions in an emergency setting as defined by scope of practice and according to agency policy. P-1-4 Demonstrate knowledge and ability to obtain, assess and monitor diagnostic tests and lab values according to agency policy. P-1-5 Demonstrate knowledge and ability to communicate, collaborate and consult with emergency care team. 142 Saskatchewan Association of Licensed Practical Nurses, Competency Profile for LPNs, 3rd Ed. Competency: P-1 Page: 2 Emergency Nursing A Licensed Practical Nurse will: P-1-6 Demonstrate knowledge and ability to obtain additional education and certification in emergency assessment, intervention and care including: emergency assessment certifications o cardiac life support o emergency neonatal care o emergency nursing o emergency pediatric nursing o pediatric life support o trauma nursing additional certifications -

Journal of Emergency Nursing
Journal of Emergency Nursing Volume 31, Issue 6, Pages 515-612 (December 2005) 1. Table of Contents • CONTENTS LIST Pages A3-A8 2. Editorial Board • EDITORIAL BOARD Pages A11-A12 3. Author Guidelines • MISCELLANEOUS Pages A15-A16 4. Info for Readers • MISCELLANEOUS Page A20 President's Message 5. A Time for Giving • ARTICLE Page 515 Patricia Kunz Howard Editorial 6. Happy Holidays! • EDITORIAL Page 516 Gail Pisarcik Lenehan Letters 7. Head for the Hill • CORRESPONDENCE Page 517 Peter Kamon 8. Nurse/Victim: The Fallacy of the Divide • CORRESPONDENCE Page 518 James MacColl Research 9. A Descriptive Study of the Perceptions of Workplace Violence and Safety Strategies of Nurses Working in Level I Trauma Centers • ARTICLE Pages 519-525 Martha Catlette Clinical 10. Emergency Response to the Gulf Coast Devastation by Hurricanes Katrina and Rita: Experiences and Impressions • ARTICLE Pages 526-547 Iris C. Frank 11. The Creation of a Behavioral Health Unit as Part of the Emergency Department: One Community Hospital's Two-Year Experience • ARTICLE Pages 548-554 Christina Lewis, Gina Sierzega and Diana Haines Case Review 12. A 4-year-old Boy With Pulmonary Hemosiderosis and Respiratory Distress Requiring Use of a Cuffed Endotracheal Tube • SHORT COMMUNICATION Pages 555-557 Emily Colyer CEN Review Questions 13. Knowledge Assessment and Preparation for the Certified Emergency Nurses Examination • MISCELLANEOUS Pages 558-559 Carrie A. McCoy Clinical Notebook 14. Allow Natural Death: A More Humane Approach to Discussing End-of-Life Directives • SHORT COMMUNICATION Pages 560-561 Crissy Knox and John A. Vereb 15. A Percutaneous Coronary Intervention Kit and Program and PCI Kit: Reducing Door-to-Cath Lab Time • SHORT COMMUNICATION Pages 562-563 Julie Bunn and Elizabeth Coombes 16. -

Nursing Workforce Standards for Type 1 Emergency Departments
Nursing Workforce Standards for Type 1 Emergency Departments October 2020 Contents Foreword Foreword 3 Patients depend on acute care delivered in our Emergency Departments (EDs). We Scope 4are the frontline of the NHS. An appropriate Glossary of Nursing Roles in the Emergency Department 5 ED workforce is the most important factor for providing safe, effective, high quality Nursing Workforce Standards for emergency care in a timely, cost-effective Type 1 Emergency Departments 7and sustainable manner. This requires a balanced team of nurses, doctors, allied Converting the nursing workforce model health professionals and support staff, with into a Whole Time Equivalent (WTE) number 14 appropriate knowledge and skills. Determining the financial cost of the total WTE nursing workforce 15 Over time a number of organisations have endeavoured to make recommendations References 16 regarding the nursing workforce in EDs [1,2]. However, specific standards have Professor Dame Donna Kinnair Appendix - Approaches that may be used Chief Executive and General Secretary never previously been established. of the Royal College of Nursing to determine the nursing workforce 17 Authors and acknowledgments 18 Therefore, in the collective interests of patient safety and quality of care, the Royal College of Nursing (RCN) Emergency Care Association (ECA) and the Royal College of Emergency Medicine (RCEM) have collaborated to define, for the first time, the nursing workforce standards for Type 1 EDs. This collaboration represents something greater than just a workforce standard – it represents a recognition that the ED team is truly multidisciplinary. Dr Katherine Henderson President of the Royal College of Emergency Medicine 2 3 Scope Glossary of Nursing Roles in the Emergency Department Adapted from the RCN ECA National Foundation Staff Nurse: A Registered Nurse who This document details the nursing These standards are not intended for use Curriculum and Competency Framework is either newly qualified, or new to emergency workforce standards for Type 1 EDs. -

Advanced Interpretation of Adult Vital Signs in Trauma William D
Advanced Interpretation of Adult Vital Signs in Trauma William D. Hampton, DO Emergency Physician 26 March 2015 Learning Objectives 1. Better understand vital signs for what they can tell you (and what they can’t) in the assessment of a trauma patient. 2. Appreciate best practices in obtaining accurate vital signs in trauma patients. 3. Learn what teaching about vital signs is evidence-based and what is not. 4. Explain the importance of vital signs to more accurately triage, diagnose, and confidently disposition our trauma patients. 5. Apply the monitoring (and manipulation of) vital signs to better resuscitate trauma patients. Disclosure Statement • Faculty/Presenters/Authors/Content Reviewers/Planners disclose no conflict of interest relative to this educational activity. Successful Completion • To successfully complete this course, participants must attend the entire event and complete/submit the evaluation at the end of the session. • Society of Trauma Nurses is accredited as a provider of continuing nursing education by the American Nurses Credentialing Center's Commission on Accreditation. Vital Signs Vital Signs Philosophy: “View vital signs as compensatory to the illness/complaint as opposed to primary.” Crowe, Donald MD. “Vital Sign Rant.” EMRAP: Emergency Medicine Reviews and Perspectives. February, 2010. Vital Signs Truth over Accuracy: • Document the true status of the patient: sick or not? • Complete vital signs on every patient, every time, regardless of the chief complaint. • If vital signs seem misleading or inaccurate, repeat them! • Beware sending a patient home with abnormal vitals (especially tachycardia)! •Treat vital signs the same as any other diagnostics— review them carefully prior to disposition. The Mother’s Vital Sign: Temperature Case #1 - 76-y/o homeless ♂ CC: 76-y/o homeless ♂ brought to the ED by police for eval. -

Cardiovascular Assessment
Cardiovascular Assessment A Home study Course Offered by Nurses Research Publications P.O. Box 480 Hayward CA 94543-0480 Office: 510-888-9070 Fax: 510-537-3434 No unauthorized duplication photocopying of this course is permitted Editor: Nurses Research 1 HOW TO USE THIS COURSE Thank you for choosing Nurses Research Publication home study for your continuing education. This course may be completed as rapidly as you desire. However there is a one-year maximum time limit. If you have downloaded this course from our website you will need to log back on to pay and complete your test. After you submit your test for grading you will be asked to complete a course evaluation and then your certificate of completion will appear on your screen for you to print and keep for your records. Satisfactory completion of the examination requires a passing score of at least 70%. No part of this course may be copied or circulated under copyright law. Instructions: 1. Read the course objectives. 2. Read and study the course. 3. Log back onto our website to pay and take the test. If you have already paid for the course you will be asked to login using the username and password you selected when you registered for the course. 4. When you are satisfied that the answers are correct click grade test. 5. Complete the evaluation. 6. Print your certificate of completion. If you have a procedural question or “nursing” question regarding the materials, call (510) 888-9070 for assistance. Only instructors or our director may answer a nursing question about the test. -

Bates' Pocket Guide to Physical Examination and History Taking
Lynn S. Bickley, MD, FACP Clinical Professor of Internal Medicine School of Medicine University of New Mexico Albuquerque, New Mexico Peter G. Szilagyi, MD, MPH Professor of Pediatrics Chief, Division of General Pediatrics University of Rochester School of Medicine and Dentistry Rochester, New York Acquisitions Editor: Elizabeth Nieginski/Susan Rhyner Product Manager: Annette Ferran Editorial Assistant: Ashley Fischer Design Coordinator: Joan Wendt Art Director, Illustration: Brett MacNaughton Manufacturing Coordinator: Karin Duffield Indexer: Angie Allen Prepress Vendor: Aptara, Inc. 7th Edition Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins. Copyright © 2009 by Wolters Kluwer Health | Lippincott Williams & Wilkins. Copyright © 2007, 2004, 2000 by Lippincott Williams & Wilkins. Copyright © 1995, 1991 by J. B. Lippincott Company. All rights reserved. This book is protected by copyright. No part of this book may be reproduced or transmitted in any form or by any means, including as photocopies or scanned-in or other electronic copies, or utilized by any information storage and retrieval system without written permission from the copyright owner, except for brief quotations embodied in critical articles and reviews. Materials appear- ing in this book prepared by individuals as part of their official duties as U.S. government employees are not covered by the above-mentioned copyright. To request permission, please contact Lippincott Williams & Wilkins at Two Commerce Square, 2001 Market Street, Philadelphia PA 19103, via email at [email protected] or via website at lww.com (products and services). 9 8 7 6 5 4 3 2 1 Printed in China Library of Congress Cataloging-in-Publication Data Bickley, Lynn S. Bates’ pocket guide to physical examination and history taking / Lynn S. -

GYNECOLOGY Helen B. Albano, MD, FPOGS Medical History • The
GYNECOLOGY Only one Helen B. Albano, MD, FPOGS Reason for admission Common gynecological complaints Medical History o Bleeding (vaginal) The quality of the medical care provided by the o Pain (specify: use 9 regions of abdomen) physician o Mass (abdominal or pelvic) Type of relationship between physician and the o Vaginal discharge patient o Urinary or GI symptoms Can be determined largely the depth of o o Protrusion out of the vagina gynecological history o Infertility Patient-Doctor Relationship o Complete history HPI (History of Present Illness) o Complete PE Refers to the chief complaint o Labs o Duration New Patient o Severity o Take Time o Precipitating factors . Obtain comprehensive history o Occurrence in relation to other events . Perform comprehensive PE . Menstrual cycle o Establish data base, along with DPR basd on . Voiding a good communication . Bowel movements Old Patient or the established patient History of similar symptoms Updates o Outcome of previous therapies . Gynecological changes Impact on the patient’s: . Pregnancy history o Quality of life . Additional surgery, accidents or new o Self-image medications o Relationship with the family (sexual history to husband) History Taking o Daily activities Overview o Most important part of gynecological Menstrual History evaluation Age of menarche o Provides tentative diagnosis (impression) Date of onset of menstrual periods before PE Duration and quantity (i.e. number of pads used per o LEGAL document . Subject to subpoena, may be day) of flow defended in court Degree of Discomfort Premenstrual symptoms General Data Cycle Name o Counted from the first day of menstrual flow Age of one cycle to the first day of menstrual Gravidity (G) flow of the next o State of being pregnant Range of normal is wide Normal range of ovulatory cycles Parity (P) o . -

Asan Medical Center Comprehensive Health Evaluation Program
Asan Medical Center Comprehensive Health Evaluation Program Fee (1,000 KRW) Fundamental check-up program • Gastroscopy with • Abdominal ultrasonography • Thyroid ultrasonography • Blood pressure • Chest X-ray (front,lateral) conscious sedation • Lumbar X-ray • Ophthalmic Exam • Audiometry test • Pulmonary function test • Body Measurement (front, lateral) • Bone mineral density • Dental assessment • Urine test • Stool test • Electrocardiogram Male Essential • Blood sampling (Diabetes, Hypercholesteremia, Liver function, Hepatitis A/B/C, Kidney function, Electrolyte, Uric Acid, 1,850 Complete Blood Count, Blood Coagulation Test, Blood type,Inflammation,Thyroid function) (3hours) • Cancer marker(liver, lung, digestive organ, prostate, ovary) • Infection (Sypilis, AIDS) • Helicobacter pylori Female • Result consultation with a specialist • CD Copy 1,950 Male • Carotid ultrasonography • Prostate ultrasonography • Digital rectal examination • Male hormone • Pelvic ultrasonography • Pelvic examination • Pap smear • HPV Female • Breast Ultrasonography • Mammogram • Female hormone Specialized check-up program with a cancer for early detection Male Specialized 2,550 Cancer Standard + • Abdominal & Pelvic CT • Chest CT • Colonoscopy with conscious sedation Female (5hours) Program 2,650 Specialized check-up program for detecting disease of cardiovascular system (Colonoscopy not included) Male Specialized 2,700 Heart Standard • Coronary CT • Fat measurement CT • Echocardiography • Treadmill test Female (4hours) Program + • Ankle-Brachical • Heart -

Brain Pulsatility and Pulsatile Tinnitus: Clinical Types
EDITORIAL International Tinnitus Journal. 2012;17(1):2-3. Brain pulsatility and pulsatile tinnitus: clinical types The purpose of this commentary is to share our supported in the literature by animal and human studies evolving clinical experience with the tympanic membrane ongoing since 1980. The raw data analysis of the IPPA displacement (TMD) analyzer which has focused on wave in patients with nonpulsatile, predominantly central- brain pulsatility in nonpulsatile, predominantly central- type severe disabling SIT resistant to attempts for tinnitus type severe disabling subjective idiopathic tinnitus relief with instrumentation or medication are published (SIT) patients resistant to attempts for tinnitus relief with in this issue of the International Tinnitus Journal (see the instrumentation or medication. article “The Tympanic Membrane Displacement Test and One outcome of this evolving TMD experience Tinnitus”). has been the establishment of a classification system for In our experience, the extensive otologic, pulsatile tinnitus and its clinical translation for diagnosis neurotologic, and neuroradiolgical workup for pulsatile and treatment. tinnitus is frequently negative, and the etiology of the A new discipline, brain pulsatility, has been pulsation is a vascular hypothesis based predominantly emerging in the last 50-60 years, the principles of which on the clinical history and or physical examination. The are based on physical principles of matter, volume, and establishment of an accurate diagnosis and treatment pressure relationships in a confined area (i.e., brain) of pulsatile tinnitus has a satisfactory outcome to the and find clinical translation to the ear and the discipline patient and physician when a pathological process is of tinnitology - in particular, pulsatile tinnitus. -
Module 10: Vital Signs
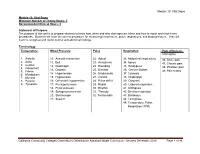
Module 10: Vital Signs Module 10: Vital Signs Minimum Number of Theory Hours: 3 Recommended Clinical Hours: 6 Statement of Purpose: The purpose of this unit is to prepare students to know how, when and why vital signs are taken and how to report and chart these procedures. Students will learn the correct procedure for measuring temperature, pulse, respirations, and blood pressure. They will learn to recognize and report normal and abnormal findings. Terminology: Temperature: Blood Pressure Pulse Respiration Pain (effects on Vital signs) 1. Afebrile 10. Aneroid manometer 22. Apical 33. Abdominal respirations 46. Acute pain 2. Axilla 11. Bell 23. Arrhythmia 34. Apnea 47. Chronic pain 3. Celsius 12. Diaphragm 24. Bounding 35. Bradypnea 4. Fahrenheit 48. Phantom pain 13. Diastolic 25. Brachial 36. Cheyne-Stokes 5. Febrile 49. Pain scales 6. Metabolism 14. Hypertension 26. Bradycardia 37. Cyanosis 7. Mucosa 15. Hypotension 27. Carotid 38. Diaphragm 8. Pyrexia 16. Orthostatic hypotension 28. Pulse deficit 39. Dyspnea 9. Tympanic 17. Pre-hypertension 29. Radial 40. Labored respiration 18. Pulse pressure 30. Rhythm 41. Orthopnea 19. Sphygmomanometer 31. Thready 42. Shallow respiration 20. Stethoscope 32. Tachycardia 43. Stertorous 21. Systolic 44. Tachypnea 45. Temperature, Pulse, Respiration (TPR) Patient, patient/resident, and client are synonymous terms Californiareferring to Community the person Colleges Chancellor’s Office Nurse Assistant Model Curriculum - Revised December 2018 Page 1 of 46 receiving care Module 10: Vital Signs Patient, resident, and client are synonymous terms referring to the person receiving care Performance Standards (Objectives): Upon completion of three (3) hours of class plus homework assignments and six (6) hours of clinical experience, the student will be able to: 1. -

Mod. 3 Vital Signs
Mod. 3 Vital Signs 1. What is most important to assess during secondary assessment? a. Airway b. Pulse c. Respiration d. Chief complaint 2. The first set of vital sign measurements obtained are often referred to as which of the following? a. Baseline vital signs b. Normal vital signs c. Standard vital signs d. None of the above 3. A patient with a pulse rate of 120 beats per minute is considered which of the following? a. Dyscardic b. Normocardic c. Tachycardic d. Bradycardic 4. Where do baseline vital signs fit into the sequence of patient assessment? a. Ongoing assessment b. At primary assessment c. At secondary assessment d. At the patient's side 5. In a conscious adult patient, which of the following pulses should be assessed initially? a. Brachial b. Radial c. Carotid d. Pedal 6. You are assessing a 55-year-old male complaining of chest pain and have determined that his radial pulse is barely palpable. You also determine that there were 20 pulsations over a span of 30 seconds. Based on this, how would you report this patient's pulse? a. Pulse 20, weak, and regular b. Pulse 20 and weak c. Pulse 40 and weak d. Pulse 40, weak, and irregular 7. Which of the following are the vital signs that need to be recorded? a. Pulse, respiration, skin color, skin temperature and condition b. Pulse, respiration, skin color, skin temperature and condition, pupils, blood pressure, and bowel sounds c. Pulse, respiration, skin color, skin temperature and condition, pupils, and blood pressure d. Pulse, respiration, skin color, skin temperature, pupils, and blood pressure 8. -

History & Physical Format
History & Physical Format SUBJECTIVE (History) Identification name, address, tel.#, DOB, informant, referring provider CC (chief complaint) list of symptoms & duration. reason for seeking care HPI (history of present illness) - PQRST Provocative/palliative - precipitating/relieving Quality/quantity - character Region - location/radiation Severity - constant/intermittent Timing - onset/frequency/duration PMH (past medical /surgical history) general health, weight loss, hepatitis, rheumatic fever, mono, flu, arthritis, Ca, gout, asthma/COPD, pneumonia, thyroid dx, blood dyscrasias, ASCVD, HTN, UTIs, DM, seizures, operations, injuries, PUD/GERD, hospitalizations, psych hx Allergies Meds (Rx & OTC) SH (social history) birthplace, residence, education, occupation, marital status, ETOH, smoking, drugs, etc., sexual activity - MEN, WOMEN or BOTH CAGE Review Ever Feel Need to CUT DOWN Ever Felt ANNOYED by criticism of drinking Ever Had GUILTY Feelings Ever Taken Morning EYE OPENER FH (family history) age & cause of death of relatives' family diseases (CAD, CA, DM, psych) SUBJECTIVE (Review of Systems) skin, hair, nails - lesions, rashes, pruritis, changes in moles; change in distribution; lymph nodes - enlargement, pain bones , joints muscles - fractures, pain, stiffness, weakness, atrophy blood - anemia, bruising head - H/A, trauma, vertigo, syncope, seizures, memory eyes- visual loss, diplopia, trauma, inflammation glasses ears - deafness, tinnitis, discharge, pain nose - discharge, obstruction, epistaxis mouth - sores, gingival bleeding, teeth,