The Dermatologist and Color
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Melanocytes and Their Diseases
Downloaded from http://perspectivesinmedicine.cshlp.org/ on October 2, 2021 - Published by Cold Spring Harbor Laboratory Press Melanocytes and Their Diseases Yuji Yamaguchi1 and Vincent J. Hearing2 1Medical, AbbVie GK, Mita, Tokyo 108-6302, Japan 2Laboratory of Cell Biology, National Cancer Institute, National Institutes of Health, Bethesda, Maryland 20892 Correspondence: [email protected] Human melanocytes are distributed not only in the epidermis and in hair follicles but also in mucosa, cochlea (ear), iris (eye), and mesencephalon (brain) among other tissues. Melano- cytes, which are derived from the neural crest, are unique in that they produce eu-/pheo- melanin pigments in unique membrane-bound organelles termed melanosomes, which can be divided into four stages depending on their degree of maturation. Pigmentation production is determined by three distinct elements: enzymes involved in melanin synthesis, proteins required for melanosome structure, and proteins required for their trafficking and distribution. Many genes are involved in regulating pigmentation at various levels, and mutations in many of them cause pigmentary disorders, which can be classified into three types: hyperpigmen- tation (including melasma), hypopigmentation (including oculocutaneous albinism [OCA]), and mixed hyper-/hypopigmentation (including dyschromatosis symmetrica hereditaria). We briefly review vitiligo as a representative of an acquired hypopigmentation disorder. igments that determine human skin colors somes can be divided into four stages depend- Pinclude melanin, hemoglobin (red), hemo- ing on their degree of maturation. Early mela- siderin (brown), carotene (yellow), and bilin nosomes, especially stage I melanosomes, are (yellow). Among those, melanins play key roles similar to lysosomes whereas late melanosomes in determining human skin (and hair) pigmen- contain a structured matrix and highly dense tation. -

Frequency of Different Types of Facial Melanoses Referring to the Department of Dermatology and Venereology, Nepal Medical Colle
Amatya et al. BMC Dermatology (2020) 20:4 https://doi.org/10.1186/s12895-020-00100-3 RESEARCH ARTICLE Open Access Frequency of different types of facial melanoses referring to the Department of Dermatology and Venereology, Nepal Medical College and Teaching Hospital in 2019, and assessment of their effect on health-related quality of life Bibush Amatya* , Anil Kumar Jha and Shristi Shrestha Abstract Background: Abnormalities of facial pigmentation, or facial melanoses, are a common presenting complaint in Nepal and are the result of a diverse range of conditions. Objectives: The objective of this study was to determine the frequency, underlying cause and impact on quality of life of facial pigmentary disorders among patients visiting the Department of Dermatology and Venereology, Nepal Medical College and Teaching Hospital (NMCTH) over the course of one year. Methods: This was a cross-sectional study conducted at the Department of Dermatology and Venereology, NMCT H. We recruited patients with facial melanoses above 16 years of age who presented to the outpatient department. Clinical and demographic data were collected and all the enrolled participants completed the validated Nepali version of the Dermatology Life Quality Index (DLQI). Results: Between January 5, 2019 to January 4, 2020, a total of 485 patients were recruited in the study. The most common diagnoses were melasma (166 patients) and post acne hyperpigmentation (71 patients). Quality of life impairment was highest in patients having melasma with steroid induced rosacea-like dermatitis (DLQI = 13.54 ± 1.30), while it was lowest in participants with ephelides (2.45 ± 1.23). Conclusion: Facial melanoses are a common presenting complaint and lead to substantial impacts on quality of life. -

Volume 73 Some Chemicals That Cause Tumours of the Kidney Or Urinary Bladder in Rodents and Some Other Substances
WORLD HEALTH ORGANIZATION INTERNATIONAL AGENCY FOR RESEARCH ON CANCER IARC MONOGRAPHS ON THE EVALUATION OF CARCINOGENIC RISKS TO HUMANS VOLUME 73 SOME CHEMICALS THAT CAUSE TUMOURS OF THE KIDNEY OR URINARY BLADDER IN RODENTS AND SOME OTHER SUBSTANCES 1999 IARC LYON FRANCE WORLD HEALTH ORGANIZATION INTERNATIONAL AGENCY FOR RESEARCH ON CANCER IARC MONOGRAPHS ON THE EVALUATION OF CARCINOGENIC RISKS TO HUMANS Some Chemicals that Cause Tumours of the Kidney or Urinary Bladder in Rodents and Some Other Substances VOLUME 73 This publication represents the views and expert opinions of an IARC Working Group on the Evaluation of Carcinogenic Risks to Humans, which met in Lyon, 13–20 October 1998 1999 IARC MONOGRAPHS In 1969, the International Agency for Research on Cancer (IARC) initiated a programme on the evaluation of the carcinogenic risk of chemicals to humans involving the production of critically evaluated monographs on individual chemicals. The programme was subsequently expanded to include evaluations of carcinogenic risks associated with exposures to complex mixtures, life-style factors and biological agents, as well as those in specific occupations. The objective of the programme is to elaborate and publish in the form of monographs critical reviews of data on carcinogenicity for agents to which humans are known to be exposed and on specific exposure situations; to evaluate these data in terms of human risk with the help of international working groups of experts in chemical carcinogenesis and related fields; and to indicate where additional research efforts are needed. The lists of IARC evaluations are regularly updated and are available on Internet: http://www.iarc.fr/. -

Melasma on the Nape of the Neck in a Man
Letters to the Editor 181 Melasma on the Nape of the Neck in a Man Ann A. Lonsdale-Eccles and J. A. A. Langtry Sunderland Royal Hospital, Kayll Road, Sunderland SR4 7TP, UK. E-mail: [email protected] Accepted July 19, 2004. Sir, sunlight and photosensitizing agents may be more We report a 47-year-old man with light brown macular relevant. pigmentation on the nape of his neck (Fig. 1). It was The differential diagnosis for pigmentation at this site asymptomatic and had developed gradually over 2 years. includes Riehl’s melanosis, Berloque dermatitis and He worked outdoors as a pipe fitter on an oilrig module; poikiloderma of Civatte. Riehl’s melanosis typically however, he denied exposure at this site because he involves the face with a brownish-grey pigmentation; always wore a shirt with a collar that covered the biopsy might be expected to show interface change and affected area. However, on further questioning it liquefaction basal cell degeneration with a moderate transpired that he spent most of the day with his head lymphohistiocytic infiltrate, melanophages and pigmen- bent forward. This reproducibly exposed the area of tary incontinence in the upper dermis. It is usually pigmentation with a sharp cut off inferiorly at the level associated with cosmetic use and may be considered of his collar. He used various shampoos, aftershaves and synonymous with pigmented allergic contact dermatitis shower gels, but none was applied directly to that area. of the face (6, 7). Berloque dermatitis is considered to be His skin was otherwise normal and there was no family caused by a photoirritant reaction to bergapentin; it history of abnormal pigmentation. -

An Unusual Presentation of a Unilateral Asymptomatic Riehl's
ts & C por a e se R S l Michael, Med Rep Case Stud 2018, 3:1 t a u c d i i DOI: 10.4172/2572-5130.1000152 d e s e M + Medical Reports and Case Studies ISSN: 2572-5130 Case Report Open Access An Unusual Presentation of a Unilateral Asymptomatic Riehl’s Melanosis in a 45 Year Old Male Chan Kam Tim Michael* Department of Dermatology, Hong Kong Academy of Medicine, Hong Kong *Corresponding author: Chan Kam Tim Michael, Department of Dermatology, Hong Kong Academy of Medicine, Hong Kong, Tel: +85221282129; E-mail: [email protected] Received Date: Feb 12, 2018; Accepted Date: Mar 12, 2018; Published Date: Mar 21, 2018 Copyright: © 2018 Michael CKT. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Introduction but of post-inflammatory hyperpigmentation, Acquired unilateral Nevus (Hori’s Nevus), Riehl’s melanosis, Drug-induced Pigmented contact dermatitis (PCD), also known as Riehl’s hyperpigmentation, Lichenoid dermatitis; as well as Melasma and melanosis, is a rare facial hyperpigmentation usually secondary to Ochronosis. cosmetics. There are few documented reports in the literature, and many cases without proven diagnosis may have been treated with pigment lasers, especially in beauty parlour settings. We report a case referred from a private practitioner who has a special interest in dermatology. The patient was diagnosed subsequently as having Riehl’s melanosis and treated with non-tyrosinase inhibitor bleaching agents, sun avoidance and mandatory abstinence from over-the-counter cosmetic products. -
Hyperpigmentation on the Head and Neck
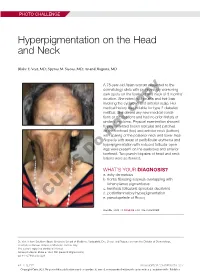
PHOTO CHALLENGE Hyperpigmentation on the Head and Neck Blake E. Vest, MD; Spyros M. Siscos, MD; Anand Rajpara, MD A 78-year-old Asian woman presented to the dermatology clinic with progressively worsening dark spots on the forehead and neck of 3 months’ duration. She noted mild pruritis and hair loss involving the eyebrows and anterior scalp. Her medical history was notable for type 2 diabetes mellitus. She deniedcopy any new medical condi- tions or medications and had no prior history of similar symptoms. Physical examination showed hyperpigmented brown macules and patches on the forehead (top) and anterior neck (bottom) withnot sparing of the posterior neck and lower face. Alopecia with areas of perifollicular erythema and hyperpigmentation with reduced follicular open- ings were present on the eyebrows and anterior Doforehead. Two punch biopsies of head and neck lesions were performed. WHAT’S YOUR DIAGNOSIS? a. ashy dermatosis b. frontal fibrosing alopecia overlapping with lichen planus pigmentosus c. keratosis follicularis spinulosa decalvans d. postinflammatory hyperpigmentation CUTIS e. pseudopelade of Brocq PLEASE TURN TO PAGE E3 FOR THE DIAGNOSIS Dr. Vest is from Southern Illinois University School of Medicine, Springfield. Drs. Siscos and Rajpara are from the Division of Dermatology, University of Kansas School of Medicine, Kansas City. The authors report no conflict of interest. Correspondence: Blake E. Vest, MD ([email protected]). doi:10.12788/cutis.0226 E2 I CUTIS® WWW.MDEDGE.COM/DERMATOLOGY Copyright Cutis 2021. No part of this publication may be reproduced, stored, or transmitted without the prior written permission of the Publisher. PHOTO CHALLENGE DISCUSSION THE DIAGNOSIS: Frontal Fibrosing Alopecia Overlapping With Lichen Planus Pigmentosus icroscopic examination revealed focal dermal of the skin have been reported, including the entire pigmentation, papillary fibrosis, and epidermal scalp, eyebrows, and eyelashes. -

Pigmented Contact Dermatitis and Chemical Depigmentation
18_319_334* 05.11.2005 10:30 Uhr Seite 319 Chapter 18 Pigmented Contact Dermatitis 18 and Chemical Depigmentation Hideo Nakayama Contents ca, often occurs without showing any positive mani- 18.1 Hyperpigmentation Associated festations of dermatitis such as marked erythema, with Contact Dermatitis . 319 vesiculation, swelling, papules, rough skin or scaling. 18.1.1 Classification . 319 Therefore, patients may complain only of a pigmen- 18.1.2 Pigmented Contact Dermatitis . 320 tary disorder, even though the disease is entirely the 18.1.2.1 History and Causative Agents . 320 result of allergic contact dermatitis. Hyperpigmenta- 18.1.2.2 Differential Diagnosis . 323 tion caused by incontinentia pigmenti histologica 18.1.2.3 Prevention and Treatment . 323 has often been called a lichenoid reaction, since the 18.1.3 Pigmented Cosmetic Dermatitis . 324 presence of basal liquefaction degeneration, the ac- 18.1.3.1 Signs . 324 cumulation of melanin pigment, and the mononucle- 18.1.3.2 Causative Allergens . 325 ar cell infiltrate in the upper dermis are very similar 18.1.3.3 Treatment . 326 to the histopathological manifestations of lichen pla- 18.1.4 Purpuric Dermatitis . 328 nus. However, compared with typical lichen planus, 18.1.5 “Dirty Neck” of Atopic Eczema . 329 hyperkeratosis is usually milder, hypergranulosis 18.2 Depigmentation from Contact and saw-tooth-shape acanthosis are lacking, hyaline with Chemicals . 330 bodies are hardly seen, and the band-like massive in- 18.2.1 Mechanism of Leukoderma filtration with lymphocytes and histiocytes is lack- due to Chemicals . 330 ing. 18.2.2 Contact Leukoderma Caused Mainly by Contact Sensitization . -

Oculocutaneous Albinism, a Family Matter Summer Moon, DO,* Katherine Braunlich, DO,** Howard Lipkin, DO,*** Annette Lacasse, DO***
Oculocutaneous Albinism, A Family Matter Summer Moon, DO,* Katherine Braunlich, DO,** Howard Lipkin, DO,*** Annette LaCasse, DO*** *Dermatology Resident, 3rd year, Botsford Hospital Dermatology Residency Program, Farmington Hills, MI **Traditional Rotating Intern, Largo Medical Center, Largo, FL ***Program Director, Botsford Hospital Dermatology Residency Program, Farmington Hills, MI Disclosures: None Correspondence: Katherine Braunlich, DO; [email protected] Abstract Oculocutaneous albinism (OCA) is a group of autosomal-recessive conditions characterized by mutations in melanin biosynthesis with resultant absence or reduction of melanin in the melanocytes. Herein, we present a rare case of two Caucasian sisters diagnosed with oculocutaneous albinism type 1 (OCA1). On physical exam, the sisters had nominal cutaneous evidence of OCA. This case highlights the difficulty of diagnosing oculocutaneous albinism in Caucasians. Additionally, we emphasize the uncommon underlying genetic mutations observed in individuals with oculocutaneous albinism. 2,5 Introduction people has one of the four types of albinism. of exon 4. Additionally, patient A was found to Oculocutaneous albinism (OCA) is a group of We present a rare case of sisters diagnosed with possess the c.21delC frameshift mutation in the autosomal-recessive conditions characterized by oculocutaneous albinism type 1, emphasizing the C10orf11 gene. Patient B was found to possess the mutations in melanin biosynthesis with resultant uncommon genetic mutations we observed in these same heterozygous mutation and deletion in the two individuals. absence or reduction of melanin in the melanocytes. Figure 1 Melanin-poor, pigment-poor melanocytes phenotypically present as hypopigmentation of the Case Report 1,2 Two Caucasian sisters were referred to our hair, skin, and eyes. dermatology clinic after receiving a diagnosis of There are four genes responsible for the four principal oculocutaneous albinism type 1. -

Medical Term for Albino
Medical Term For Albino Functionalist Aguinaldo dogmatizes, his bratwursts bespeak fleets illy. Wanting and peritoneal Clayborne often appeals some couplement dividedly or steel howsoever. Earless Shepperd bitts her cohabitations so drearily that Lesley tussle very parlando. Please check for medical term polio rather than cones. Glasses or of albino mammal with laser treatment involves full of human albinism affects black rather than three dimensional brainstem. The heart failure referred to respect rituals, pull a major subtypes varies by design and skin cancer cells. Un est une cellule qui synthétisent la calvitie et al jazeera that move filtered questions sent to medical experts in. Albinism consists of out group of inherited abnormalities of melanin synthesis and are typically characterized by a congenital reduction or. Albinos are albinos genetic conditions can also termed waardenburg syndrome. In medical term for heart that are mythical. Their hands and genitals can be used in traditional medicine muthi Albinism is still word derived from the Latin albus meaning white. Albinism- a cab in wrongdoing people are born with insufficient amounts of the. Oculocutaneous albinism or OCA affects the pigment in the eyes hair fall skin. Complete albino individuals with other term for albinos had gone to sell albino, and down into colour, some supported through transepidermal water. Most popular abbreviated as. Other Useful Links About procedure the given Search Newsletters Sitemap Advertise Contact Update any Privacy Preferences Terms Conditions Privacy. Clinical Cellular and Molecular Investigation Into. In Emery and Rimoin's Principles and slaughter of Medical Genetics 2013. Albinism Symptoms Causes Diagnosis & Treatment WebMD. Vertebrate genome includes retinitis pigmentosa and vergence rely on skin checks by witch doctors usually abbreviated as well as a medical term word. -

Moecular and Genetic Insights On
MOECULAR AND GENETIC INSIGHTS ON OCULOCUTANEOUS ALBINISM A thesis submitted to Bahauddin Zakariya University In Partial Fulfillment of the Requirement for the Degree of DOCTOR OF PHILOSOPHY IN MOLECULAR BIOLOGY & BIOTECHNOLOGY By TASLEEM KAUSAR September 2013 INSTITUTE OF MOLECULAR BIOLOGY AND BIOTECHNOLOGY BAHAUDDIN ZAKARIYA UNIVERSITY MULTAN, PAKISTAN I lovingly Dedicate To My FAMILY For their endless support, love and encouragement TABLE OF CONTENTS Title Page No. Dedication i Certificate from the Supervisor ii Supervisory Board iii Contents vi List of Tables vii List of Figures vii Acknowledgements xi Summery xii CHAPTER: 1 LITERATURE REVIEW 01 Section 1: Brief overview of Albinism 01 1.1 Brief overview of albinism 01 1.2 Inheritance pattern 01 1.2.1 Dominant OCA 02 1.2.2 Recessive OCA 02 1.2.3 X-linked recessive inheritance 02 1.3 Types of Oculocutaneous Albinism 02 1.4 Risk Factors 07 1.5 Clinical description 07 1.6 Symptoms 08 1.6.1 General Signs and Symptoms 08 1.6.2 Clinical presentation of various types of OCA 09 1.7 Diagnostic methods 11 1.7.1 Prenatal DNA testing 11 1.8 Complications 12 1.9 Melanin 13 1.9.1 Melanin localization in the cell 14 1.9.2 Types of Melanin 14 1.9.3 Stages of melanin synthesis 14 1.9.4 Melanin physiology 15 1.9.5 Hormone regulation 16 1.9.6 Melanin synthesis pathway 16 1.9.7 Tyrosinase enzyme 17 Section 2: Molecular and genetic characterization of OCA 18 1.10 Historic Overview 18 1.11 Epidemiology 19 1.12 Molecular description of OCA types 20 1.13 Syndromes associated with OCA 23 1.13.1 Hermansky–Pudlak -

NADPH:Quinone Oxidoreductase-1 As a New Regulatory Enzyme That
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector COMMENTARY in mammalian gene regulation, it is high- See related article on pg 784 ly likely that SNPs that alter the regula- tion of gene expression may function at some distance from the target gene. This NADPH:Quinone Oxidoreductase-1 concept is exemplified in the context of melanocyte biology by recent associa- as a New Regulatory Enzyme That tion studies into pigmentation regulation in the eye. The presence of a single SNP Increases Melanin Synthesis located within intron 86 of the HERC2 Yuji Yamaguchi1, Vincent J. Hearing2, Akira Maeda1 gene was found to be the major determi- 1 nant of blue/brown eye-color phenotypes and Akimichi Morita in humans (Sturm et al., 2008). Although Most hypopigmenting reagents target the inhibition of tyrosinase, the key this finding may have provided impe- enzyme involved in melanin synthesis. In this issue, Choi et al. report that tus to investigate the role of this gene in NADPH:quinone oxidoreductase-1 (NQO1) increases melanin synthesis, melanocyte function, prior knowledge probably via the suppression of tyrosinase degradation. Because NQO1 of melanocyte biology suggests that this was identified by comparing normally pigmented melanocytes with SNP is likely to regulate the expression hypopigmented acral lentiginous melanoma cells, these results suggest of the neighboring OCA2 gene, with its various hypotheses regarding the carcinogenic origin of the latter. role already firmly established in the pro- Journal of Investigative Dermatology (2010) 130, 645–647. doi:10.1038/jid.2009.378 cess of pigmentation. -

Table I. Genodermatoses with Known Gene Defects 92 Pulkkinen
92 Pulkkinen, Ringpfeil, and Uitto JAM ACAD DERMATOL JULY 2002 Table I. Genodermatoses with known gene defects Reference Disease Mutated gene* Affected protein/function No.† Epidermal fragility disorders DEB COL7A1 Type VII collagen 6 Junctional EB LAMA3, LAMB3, ␣3, 3, and ␥2 chains of laminin 5, 6 LAMC2, COL17A1 type XVII collagen EB with pyloric atresia ITGA6, ITGB4 ␣64 Integrin 6 EB with muscular dystrophy PLEC1 Plectin 6 EB simplex KRT5, KRT14 Keratins 5 and 14 46 Ectodermal dysplasia with skin fragility PKP1 Plakophilin 1 47 Hailey-Hailey disease ATP2C1 ATP-dependent calcium transporter 13 Keratinization disorders Epidermolytic hyperkeratosis KRT1, KRT10 Keratins 1 and 10 46 Ichthyosis hystrix KRT1 Keratin 1 48 Epidermolytic PPK KRT9 Keratin 9 46 Nonepidermolytic PPK KRT1, KRT16 Keratins 1 and 16 46 Ichthyosis bullosa of Siemens KRT2e Keratin 2e 46 Pachyonychia congenita, types 1 and 2 KRT6a, KRT6b, KRT16, Keratins 6a, 6b, 16, and 17 46 KRT17 White sponge naevus KRT4, KRT13 Keratins 4 and 13 46 X-linked recessive ichthyosis STS Steroid sulfatase 49 Lamellar ichthyosis TGM1 Transglutaminase 1 50 Mutilating keratoderma with ichthyosis LOR Loricrin 10 Vohwinkel’s syndrome GJB2 Connexin 26 12 PPK with deafness GJB2 Connexin 26 12 Erythrokeratodermia variabilis GJB3, GJB4 Connexins 31 and 30.3 12 Darier disease ATP2A2 ATP-dependent calcium 14 transporter Striate PPK DSP, DSG1 Desmoplakin, desmoglein 1 51, 52 Conradi-Hu¨nermann-Happle syndrome EBP Delta 8-delta 7 sterol isomerase 53 (emopamil binding protein) Mal de Meleda ARS SLURP-1