Biobank Scale Pharmacogenomics Informs the Genetic Underpinnings
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Impaired Hepatic Drug and Steroid Metabolism in Congenital Adrenal
European Journal of Endocrinology (2010) 163 919–924 ISSN 0804-4643 CLINICAL STUDY Impaired hepatic drug and steroid metabolism in congenital adrenal hyperplasia due to P450 oxidoreductase deficiency Dorota Tomalik-Scharte1, Dominique Maiter2, Julia Kirchheiner3, Hannah E Ivison, Uwe Fuhr1 and Wiebke Arlt School of Clinical and Experimental Medicine, Centre for Endocrinology, Diabetes and Metabolism (CEDAM), University of Birmingham, Birmingham B15 2TT, UK, 1Department of Pharmacology, University Hospital, University of Cologne, 50931 Cologne, Germany, 2Department of Endocrinology, University Hospital Saint Luc, 1200 Brussels, Belgium and 3Department of Pharmacology of Natural Products and Clinical Pharmacology, University of Ulm, 89019 Ulm, Germany (Correspondence should be addressed to W Arlt; Email: [email protected]) Abstract Objective: Patients with congenital adrenal hyperplasia due to P450 oxidoreductase (POR) deficiency (ORD) present with disordered sex development and glucocorticoid deficiency. This is due to disruption of electron transfer from mutant POR to microsomal cytochrome P450 (CYP) enzymes that play a key role in glucocorticoid and sex steroid synthesis. POR also transfers electrons to all major drug- metabolizing CYP enzymes, including CYP3A4 that inactivates glucocorticoid and oestrogens. However, whether ORD results in impairment of in vivo drug metabolism has never been studied. Design: We studied an adult patient with ORD due to homozygous POR A287P, the most frequent POR mutation in Caucasians, and her clinically unaffected, heterozygous mother. The patient had received standard dose oestrogen replacement from 17 until 37 years of age when it was stopped after she developed breast cancer. Methods: Both subjects underwent in vivo cocktail phenotyping comprising the oral administration of caffeine, tolbutamide, omeprazole, dextromethorphan hydrobromide and midazolam to assess the five major drug-metabolizing CYP enzymes. -

Identification and Developmental Expression of the Full Complement Of
Goldstone et al. BMC Genomics 2010, 11:643 http://www.biomedcentral.com/1471-2164/11/643 RESEARCH ARTICLE Open Access Identification and developmental expression of the full complement of Cytochrome P450 genes in Zebrafish Jared V Goldstone1, Andrew G McArthur2, Akira Kubota1, Juliano Zanette1,3, Thiago Parente1,4, Maria E Jönsson1,5, David R Nelson6, John J Stegeman1* Abstract Background: Increasing use of zebrafish in drug discovery and mechanistic toxicology demands knowledge of cytochrome P450 (CYP) gene regulation and function. CYP enzymes catalyze oxidative transformation leading to activation or inactivation of many endogenous and exogenous chemicals, with consequences for normal physiology and disease processes. Many CYPs potentially have roles in developmental specification, and many chemicals that cause developmental abnormalities are substrates for CYPs. Here we identify and annotate the full suite of CYP genes in zebrafish, compare these to the human CYP gene complement, and determine the expression of CYP genes during normal development. Results: Zebrafish have a total of 94 CYP genes, distributed among 18 gene families found also in mammals. There are 32 genes in CYP families 5 to 51, most of which are direct orthologs of human CYPs that are involved in endogenous functions including synthesis or inactivation of regulatory molecules. The high degree of sequence similarity suggests conservation of enzyme activities for these CYPs, confirmed in reports for some steroidogenic enzymes (e.g. CYP19, aromatase; CYP11A, P450scc; CYP17, steroid 17a-hydroxylase), and the CYP26 retinoic acid hydroxylases. Complexity is much greater in gene families 1, 2, and 3, which include CYPs prominent in metabolism of drugs and pollutants, as well as of endogenous substrates. -
Mycode®: Engineering the Perfect Biobank
Linking the Research Community • Spring 2015 A message from MyCode®: Engineering the David H. Ledbetter, PhD Perfect Biobank Geisinger’s biobank and the MyCode® Community Health This issue of Research Initiative began in 2004 with a phone call from Glenn D. Connections is devoted to the Steele Jr., MD, PhD, Geisinger’s former president and CEO, to MyCode® Community Health David H. Ledbetter, PhD, then at Emory University’s School Initiative, a project with the of Medicine. Speaking genetically, not meteorologically, Steele potential to change significantly described Geisinger’s Pennsylvania footprint and resources to health and healthcare. MyCode Ledbetter as being, “as close to Iceland as you’ll ever find in the will uncover new connections United States.”* between genes and disease, inform and improve the health Ledbetter, now Geisinger’s Chief Scientific Officer, found many of Geisinger’s patients and re- similarities between Iceland and Geisinger’s central Pennsylvania envision how we approach our own well-being and that of location. Like Iceland, Geisinger’s regional population was stable, our families. often with three generations in the area. In addition, Geisinger‘s healthcare was centralized with a robust electronic health record This project is possible because of Geisinger’s specific (EHR) in place since 1996. combination of assets: an established biobank; an extensive and robust electronic health record (EHR); and According to Ledbetter, the qualities listed above, along with international expertise in bioethics, medical genetics, Geisinger’s tradition of innovation, creates, “a healthcare genetic counseling and genomics. Our partnership with laboratory and an ideal model to learn when and how genetic Regeneron, an innovative biotechnology company with information can improve health.” Ledbetter described Geisinger’s extensive resources for whole exome sequencing, is key service area as, “the ideal place in the United States to do to positioning this project to make groundbreaking longitudinal, large scale, genomic medicine research.” discoveries. -

Bioethics and Large-Scale Biobanking: Individualistic Ethics and Collective Projects*
Genomics, Society and Policy 2005, Vol.1, No.2, pp.50–66. Bioethics and large-scale biobanking: individualistic ethics and collective projects* GARRATH WILLIAMS Abstract Like most bioethical discussion, examination of human biobanks has been largely framed in terms of research subjects’ rights, principally informed consent, with some gestures toward public benefits. However, informed consent is for the competent, rights-bearing individual: focussing on the individual, it thus neglects social, economic and even political matters; focussing on the competent rights-bearer, it does not serve situations where consent is plainly inappropriate (eg, the young child) or where coercion can obviously be justified (the criminal). Using the British experience of large-scale biobanking, I argue that the focus on consenting individuals distorts our ways of thinking about biobanks and has serious practical ramifications. This becomes clear if we contrast the case of adult biobanks intended for medical research with two other forms of biobanking. Thus child cohort studies – vital for sound scientific investigation of the interplay of genetics and environment in health – have been very badly funded next to adult studies. On the other hand, forensic databases have attracted massive investment, but little debate – partly owing to a sense that here, at least, is a case where consent is not relevant. Contrasting these central types of biobanking, I will suggest that there are powerful factors at work in limiting ‘ethics’ to individual rights. Projects of this size should direct our attention to more overtly political questions concerning priority setting and organisation of medical research. Introduction In this paper I wish to cast a critical eye at the way in which we – meaning both bioethicists and practitioners – frame ethical and bioethical discussion. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

Synonymous Single Nucleotide Polymorphisms in Human Cytochrome
DMD Fast Forward. Published on February 9, 2009 as doi:10.1124/dmd.108.026047 DMD #26047 TITLE PAGE: A BIOINFORMATICS APPROACH FOR THE PHENOTYPE PREDICTION OF NON- SYNONYMOUS SINGLE NUCLEOTIDE POLYMORPHISMS IN HUMAN CYTOCHROME P450S LIN-LIN WANG, YONG LI, SHU-FENG ZHOU Department of Nutrition and Food Hygiene, School of Public Health, Peking University, Beijing 100191, P. R. China (LL Wang & Y Li) Discipline of Chinese Medicine, School of Health Sciences, RMIT University, Bundoora, Victoria 3083, Australia (LL Wang & SF Zhou). 1 Copyright 2009 by the American Society for Pharmacology and Experimental Therapeutics. DMD #26047 RUNNING TITLE PAGE: a) Running title: Prediction of phenotype of human CYPs. b) Author for correspondence: A/Prof. Shu-Feng Zhou, MD, PhD Discipline of Chinese Medicine, School of Health Sciences, RMIT University, WHO Collaborating Center for Traditional Medicine, Bundoora, Victoria 3083, Australia. Tel: + 61 3 9925 7794; fax: +61 3 9925 7178. Email: [email protected] c) Number of text pages: 21 Number of tables: 10 Number of figures: 2 Number of references: 40 Number of words in Abstract: 249 Number of words in Introduction: 749 Number of words in Discussion: 1459 d) Non-standard abbreviations: CYP, cytochrome P450; nsSNP, non-synonymous single nucleotide polymorphism. 2 DMD #26047 ABSTRACT Non-synonymous single nucleotide polymorphisms (nsSNPs) in coding regions that can lead to amino acid changes may cause alteration of protein function and account for susceptivity to disease. Identification of deleterious nsSNPs from tolerant nsSNPs is important for characterizing the genetic basis of human disease, assessing individual susceptibility to disease, understanding the pathogenesis of disease, identifying molecular targets for drug treatment and conducting individualized pharmacotherapy. -

Genetic Data Aren't So Special: Causes and Implications of Re
Genetic Data Aren’t So Special: Causes and Implications of Re-identification T.J. Kasperbauer & Peter H. Schwartz Indiana University Center for Bioethics Indiana University School of Medicine This is the pre-peer-reviewed version of the article published here: https://doi.org/10.1002/hast.1183 Full citation: Kasperbauer, T.J. & Schwartz, P.H. (2020). Genetic data aren’t so special: Causes and implications of re-identification. Hastings Center Report, 50, 30-39. Abstract: Genetic information is widely thought to pose unique risks of re-identifying individuals. Genetic data reveals a great deal about who we are, and, the standard view holds, should consequently be treated differently from other types of data. Contrary to this view, we argue that the dangers of re-identification for genetic and non-genetic data—including health, financial, and consumer information—are more similar than has been recognized. Before we impose different requirements on sharing genetic information, proponents of the standard view must show that they are in fact necessary. We further argue that the similarities between genetic and non-genetic information have important implications for communicating risks during consent for healthcare and research. While patients and research participants need to be more aware of pervasive data sharing practices, consent forms are the wrong place to provide this education. Instead, health systems should engage with patients throughout patient care to educate about data sharing practices. Introduction Genetic data and biological samples containing genetic material are widely thought to differ from other sorts of health data due to the impossibility of truly “de-identifying” genetic information. -

Human Cytochrome P450 CYP2A13
[CANCER RESEARCH 60, 5074–5079, September 15, 2000] Human Cytochrome P450 CYP2A13: Predominant Expression in the Respiratory Tract and Its High Efficiency Metabolic Activation of a Tobacco-specific Carcinogen, 4-(Methylnitrosamino)-1-(3-pyridyl)-1-butanone1 Ting Su, Ziping Bao, Qing-Yu Zhang, Theresa J. Smith, Jun-Yan Hong,2 and Xinxin Ding2 Wadsworth Center, New York State Department of Health, Albany, New York 12201 [T. S., Q-Y. Z., X. D.]; School of Public Health, State University of New York at Albany, Albany, New York [T. S., X. D.]; and Environmental and Occupational Health Sciences Institute, University of Medicine and Dentistry of New Jersey, Piscataway, New Jersey 08854 [Z. B., T. J. S., J-Y. H.] ABSTRACT However, heterologously expressed CYP2A7 showed no catalytic activity (17, 18). CYP2A13 cDNA has not been isolated previously; The human CYP2A subfamily comprises three genes, CYP2A6, the reported protein sequence was deduced from the predicted coding CYP2A7, and CYP2A13. CYP2A6 is active toward many carcinogens and region of a CYP2A13 genomic clone (1). On the basis of its sequence is the major coumarin 7-hydroxylase and nicotine C-oxidase in the liver, whereas CYP2A7 is not functional. The function of CYP2A13 has not been features that resemble the nonfunctional CYP2A7 and CYP2A6v1 (a characterized. In this study, a CYP2A13 cDNA was prepared by RNA- genetic variant of CYP2A6) proteins, the CYP2A13 protein was PCR from human nasal mucosa and was translated using a baculovirus predicted to be nonfunctional in coumarin 7-hydroxylation (1). Be- expression system. In a reconstituted system, the expressed CYP2A13 was cause the deduced amino acid sequence of CYP2A13 shares a 95.4% more active than CYP2A6 in the metabolic activation of hexamethylphos- identity with that of CYP2A6 (1), antibodies and chemical probes for phoramide, N,N-dimethylaniline, 2-methoxyacetophenone, and N-nitro- CYP2A6 may interact with CYP2A13. -

Sample Data Sharing Consent Form
PREAMBLE: NINDS has the expectation that investigators will use broad consent language that allows for the storing, sharing, and use of human subjects data and specimens for future research, even if such future research may be unrelated to the original study or disorder for which the data and/or specimens were collected. NINDS expects investigators to consider including such language (or similar language as mandated by your IRB) in your consent forms in order to ensure that samples and data are available for storing, sharing and use in future, unspecified research. This language should be included in the draft consent submitted with your application and submitted to NINDS in preparation for your start-up meeting if your application is funded (EXHIBIT 1). If genetic sample collection is a component of the study, then consent language is expected to include the sharing of large-scale genomic data and associated phenotypic data in the NIH Database of Genotypes and Phenotypes (dbGaP: http://www.ncbi.nlm.nih.gov/gap). If another database is chosen, this would require pre-approval by NINDS program staff. A final, IRB-approved consent that includes this or similar language (or an explanation for why it was not included) should be submitted to NINDS program staff prior to study activation. If you have questions or need assistance developing your consent language, please feel free to contact NINDS Clinical Research Liaison (any consents) and/or Ran Zhang (consents with genetic/genomic data language). *Please note that all studies that generate large-scale human genomic data , regardless of cost, should refer to the the NIH Genomic Data Sharing (GDS) Policy for additional requirements. -
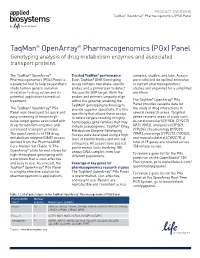
Taqman® Openarray® Pharmacogenomics (Pgx) Panel
PRODUCT OVERVIEW TaqMan® OpenArray® Pharmacogenomics (PGx) Panel TaqMan® OpenArray® Pharmacogenomics (PGx) Panel Genotyping analysis of drug metabolism enzymes and associated transport proteins The TaqMan® OpenArray® Trusted TaqMan® performance samples, studies, and labs. Assays Pharmacogenomics (PGx) Panel is Each TaqMan® DME Genotyping were selected for optimal relevance a powerful tool to help researchers Assay contains two allele-specific to current pharmacogenomics study human genetic variation probes and a primer pair to detect studies and organized for a simplified in relation to drug action and its the specific SNP target. Both the workflow. potential application to medical probes and primers uniquely align ® ® treatment. within the genome, enabling the The TaqMan OpenArray PGx TaqMan® genotyping technology to Panel provides valuable data for ® ® The TaqMan OpenArray PGx provide superior specificity. It is this the study of drug interactions in Panel was developed for quick and specificity that allows these assays several research areas. Targeted easy screening of known high- to detect targets residing in highly genes relate to areas of study such value target genes associated with homologous gene families that may as cardiovascular (CYP2D6, CYP2C19, drug metabolism enzymes and include pseudogenes. TaqMan® Drug NAT1, NAT2), analgesics (CYP2C9, associated transport proteins. Metabolism Enzyme Genotyping CYP2D6), rheumatology (CYP2C9, The panel consists of 158 drug Assays were developed using a high TPMT), neurology (CYP2C19, CYP2D6), metabolism enzyme (DME) assays level of bioinformatics and wet-lab and musculoskeletal (CYP2C19). A derived from the PharmaADME stringency. All assays have passed total of 29 genes are covered across Core Marker Set (Table 1). The performance tests involving 180 158 unique assays. -

The Views of Participants in DNA Biobanks
The Views of Participants in DNA Biobanks Kelly E. Ormond,I Maureen E. Smith,II & Wendy A. WolfIII Abstract Biobanks are generally created with the long-term goal of establishing genotype-phenotype correlations. These resources collect and link DNA with health information for use in future genetic research studies. The biobanking process can vary with regard to specific characteristics in study design. Biobanks may extract DNA by using DNA from leftover samples or obtaining new DNA samples specifically for the biobank. Biobanks also vary in whether they use an opt- in or opt-out informed consent process. Some biobanks collect health information at a single point in time, while others “re-access” such information at designated points in the future to categorize subjects accurately into affected/unaffected status. These study design differences can influence the perception of participants and affect their willingness to participate. This paper will address the following three key issues: (1) why people decide to participate in DNA biobanks, (2) what enrollees understand about their participation in DNA biobanks, and (3) how participants feel about the possibility that biobanks will re-contact them, either to obtain new information for future studies or to share potential study results. Finally, we will suggest how information related to these three key issues ought to inform future study design for biobanks. I. INTRODUCTION.................................................................................................................81 II. WHY DO PEOPLE DECIDE TO PARTICIPATE IN DNA BIOBANKS?...........................82 III. WHAT DO ENROLLEES UNDERSTAND ABOUT THEIR PARTICIPATION IN A DNA BIOBANK? ..............................................................................................................................83 IV. HOW DO PARTICIPANTS FEEL ABOUT BIOBANK RE-CONTACT, AND HOW SHOULD THIS INFORMATION INFORM STUDY DESIGN?..............................................84 V. -

Screening of Genetic Variations of SLC15A2, SLC22A1, SLC22A2 and SLC22A6 Genes
Journal of Human Genetics (2011) 56, 666–670 & 2011 The Japan Society of Human Genetics All rights reserved 1434-5161/11 $32.00 www.nature.com/jhg ORIGINAL ARTICLE Screening of genetic variations of SLC15A2, SLC22A1, SLC22A2 and SLC22A6 genes Hyun Sub Cheong1,4, Hae Deun Kim2,4, Han Sung Na2,JiOnKim1, Lyoung Hyo Kim1, Seung Hee Kim2, Joon Seol Bae3, Myeon Woo Chung2 and Hyoung Doo Shin1,3 A growing list of membrane-spanning proteins involved in the transport of a large variety of drugs has been recognized and characterized to include peptide and organic anion/cation transporters. Given such an important role of transporter genes in drug disposition process, the role of single-nucleotide polymorphisms (SNPs) in such transporters as potential determinants of interindividual variability in drug disposition and pharmacological response has been investigated. To define the distribution of transporter gene SNPs across ethnic groups, we screened 450 DNAs in cohorts of 250 Korean, 50 Han Chinese, 50 Japanese, 50 African-American and 50 European-American ancestries for 64 SNPs in four transporter genes encoding proteins of the solute carrier family (SLC15A2, SLC22A1, SLC22A2 and SLC22A6). Of the 64 SNPs, 19 were core pharmacogenetic variants and 45 were HapMap tagging SNPs. Polymorphisms were genotyped using the golden gate genotyping assay. After genetic variability, haplotype structures and ethnic diversity were analyzed, we observed that the distributions of SNPs in a Korean population were similar to other Asian groups (Chinese and Japanese), and significantly different from African-American and European-American cohorts. Findings from this study would be valuable for further researches, including pharmacogenetic studies for drug responses.