Dibutyl Phthalate Or DBP)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

HISTORY of LEAD POISONING in the WORLD Dr. Herbert L. Needleman Introduction the Center for Disease Control Classified the Cause
HISTORY OF LEAD POISONING IN THE WORLD Dr. Herbert L. Needleman Introduction The Center for Disease Control classified the causes of disease and death as follows: 50 % due to unhealthy life styles 25 % due to environment 25% due to innate biology and 25% due to inadequate health care. Lead poisoning is an environmental disease, but it is also a disease of life style. Lead is one of the best-studied toxic substances, and as a result we know more about the adverse health effects of lead than virtually any other chemical. The health problems caused by lead have been well documented over a wide range of exposures on every continent. The advancements in technology have made it possible to research lead exposure down to very low levels approaching the limits of detection. We clearly know how it gets into the body and the harm it causes once it is ingested, and most importantly, how to prevent it! Using advanced technology, we can trace the evolution of lead into our environment and discover the health damage resulting from its exposure. Early History Lead is a normal constituent of the earth’s crust, with trace amounts found naturally in soil, plants, and water. If left undisturbed, lead is practically immobile. However, once mined and transformed into man-made products, which are dispersed throughout the environment, lead becomes highly toxic. Solely as a result of man’s actions, lead has become the most widely scattered toxic metal in the world. Unfortunately for people, lead has a long environmental persistence and never looses its toxic potential, if ingested. -

A Simple, Fast, and Reliable LC-MS/MS Method for Determination and Quantification of Phthalates in Distilled Beverages
A Simple, Fast, and Reliable LC-MS/MS Method for Determination and Quantification of Phthalates in Distilled Beverages Dimple Shah and Jennifer Burgess Waters Corporation, Milford, MA, USA APPLICATION BENEFITS INTRODUCTION ■■ Separation and detection of 7 phthalates Phthalates, esters of phthalic acid, are often used as plasticizers for polymers such in 11 minutes. as polyvinylchloride. They are widely applicable in various products including personal care goods, cosmetics, paints, printing inks, detergents, coatings, ■■ Simple, quick “dilute and shoot” sample preparation method for routine applications and food packaging. These phthalates have been found to leach readily into the where high sample throughput is required. environment and food as they are not chemically bound to plastics. As such they are known to be ubiquitously present in our environment. ■■ Elimination of major phthalate contamination using the ACQUITY UPLC® Isolator Column. Phthalates have been reported to show a variety of toxic effects related to reproduction in animal studies, which has resulted in these compounds being ■■ Selective mass spectra obtained for all seven considered as endocrine disruptors. Screening food and beverages for phthalates phthalates with dominant precursor ion. contamination is required by many legislative bodies, although regulations vary ■■ Low limits of quantification achieved using from country to country in regards to acceptable daily tolerances and specific Waters® ACQUITY UPLC H-Class System migration limits. and Xevo® TQD. Traditionally, phthalates have been analyzed by gas chromatography-mass ■■ Single and robust method for a variety spectrometry (GC-MS), where derivatization and/or extraction and sample of distilled beverages. preparation is often required to improve chromatographic separation.1 The ■■ Maintain consumer confidence and resulting GC-EI-MS spectra can lack selectivity, where the base ion, used for ensure compliance in market. -

162 Part 175—Indirect Food Addi
§ 174.6 21 CFR Ch. I (4–1–19 Edition) (c) The existence in this subchapter B Subpart B—Substances for Use Only as of a regulation prescribing safe condi- Components of Adhesives tions for the use of a substance as an Sec. article or component of articles that 175.105 Adhesives. contact food shall not be construed as 175.125 Pressure-sensitive adhesives. implying that such substance may be safely used as a direct additive in food. Subpart C—Substances for Use as (d) Substances that under conditions Components of Coatings of good manufacturing practice may be 175.210 Acrylate ester copolymer coating. safely used as components of articles 175.230 Hot-melt strippable food coatings. that contact food include the fol- 175.250 Paraffin (synthetic). lowing, subject to any prescribed limi- 175.260 Partial phosphoric acid esters of pol- yester resins. tations: 175.270 Poly(vinyl fluoride) resins. (1) Substances generally recognized 175.300 Resinous and polymeric coatings. as safe in or on food. 175.320 Resinous and polymeric coatings for (2) Substances generally recognized polyolefin films. as safe for their intended use in food 175.350 Vinyl acetate/crotonic acid copoly- mer. packaging. 175.360 Vinylidene chloride copolymer coat- (3) Substances used in accordance ings for nylon film. with a prior sanction or approval. 175.365 Vinylidene chloride copolymer coat- (4) Substances permitted for use by ings for polycarbonate film. 175.380 Xylene-formaldehyde resins con- regulations in this part and parts 175, densed with 4,4′-isopropylidenediphenol- 176, 177, 178 and § 179.45 of this chapter. -
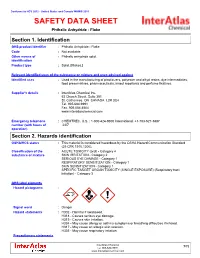
SAFETY DATA SHEET Phthalic Anhydride - Flake
Conforms to HCS 2012 - United States and Canada WHMIS 2015 SAFETY DATA SHEET Phthalic Anhydride - Flake Section 1. Identification GHS product identifier : Phthalic Anhydride - Flake Code : Not available. Other means of : Phthalic anhydride solid. identification Product type : Solid. [Flakes.] Relevant identified uses of the substance or mixture and uses advised against Identified uses : Used in the manufacturing of plasticizers, polyester and alkyd resins, dye intermediates, food preservatives, pharmaceuticals, insect repellants and perfume fixatives. Supplier's details : InterAtlas Chemical Inc. 63 Church Street, Suite 301 St. Catharines, ON CANADA L2R 3C4 Tel. 905.684.9991 Fax. 905.684.4504 www.interatlaschemical.com Emergency telephone : CHEMTREC, U.S. : 1-800-424-9300 International: +1-703-527-3887 number (with hours of 24/7 operation) Section 2. Hazards identification OSHA/HCS status : This material is considered hazardous by the OSHA Hazard Communication Standard (29 CFR 1910.1200). Classification of the : ACUTE TOXICITY (oral) - Category 4 substance or mixture SKIN IRRITATION - Category 2 SERIOUS EYE DAMAGE - Category 1 RESPIRATORY SENSITIZATION - Category 1 SKIN SENSITIZATION - Category 1 SPECIFIC TARGET ORGAN TOXICITY (SINGLE EXPOSURE) (Respiratory tract irritation) - Category 3 GHS label elements Hazard pictograms : Signal word : Danger Hazard statements : H302 - Harmful if swallowed. H318 - Causes serious eye damage. H315 - Causes skin irritation. H334 - May cause allergy or asthma symptoms or breathing difficulties if inhaled. H317 - May cause an allergic skin reaction. H335 - May cause respiratory irritation. Precautionary statements InterAtlas Chemical 1/12 Tel: 905-684-9991 www.interatlaschemical.com Phthalic Anhydride - Flake Section 2. Hazards identification Prevention : P280 - Wear protective gloves. Wear eye or face protection. -

The Condensation of Phenols with Maleic Anhydride
South Dakota State University Open PRAIRIE: Open Public Research Access Institutional Repository and Information Exchange Theses and Dissertations 1951 The ondeC nsation of Phenols with Maleic Anhydride Leslie D. Kamstra Follow this and additional works at: https://openprairie.sdstate.edu/etd Recommended Citation Kamstra, Leslie D., "The ondeC nsation of Phenols with Maleic Anhydride" (1951). Theses and Dissertations. 2215. https://openprairie.sdstate.edu/etd/2215 This Thesis - Open Access is brought to you for free and open access by Open PRAIRIE: Open Public Research Access Institutional Repository and Information Exchange. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of Open PRAIRIE: Open Public Research Access Institutional Repository and Information Exchange. For more information, please contact [email protected]. THE CONDENSATION OF PHENOLS WITH MALEIC ANHYDRIDE By Leslie D. Kamstra This thesis is approved as a creditable independent investigation by a candidate for the degree, Master of Science, and acceptable as meeting the thesis requirements for this degree, but without imVlying that the conclusions reached by the candidate are neces sarily the conclusions of the major department. ,(\ � -� fSOUTH DAKOTA ·STATE COLLEGE LIBRARY page i TABLE OF CONTENTS Introduction• ••.......•..••••••••.•••••....•.•..•.••••• #,• 1 Condensation using Hydrated and Anhydrous Stannic Chloride 2 Preparation of the Original Product•• � •...•• � 2 Determination of Temperature and Time for Optimum -

(12) Patent Application Publication (10) Pub. No.: US 2006/0020077 A1 Miyoshi Et Al
US 20060020077A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2006/0020077 A1 Miyoshi et al. (43) Pub. Date: Jan. 26, 2006 (54) ELECTRICALLY CONDUCTIVE RESIN (30) Foreign Application Priority Data COMPOSITION AND PRODUCTION PROCESS THEREOF Apr. 26, 2000 (JP)...................................... 2000-125081 (76) Inventors: Takaaki Miyoshi, Kimitsu-shi (JP); Publication Classification Kazuhiko Hashimoto, Sodegaura-shi (JP) (51) Int. Cl. C08K 3/04 (2006.01) Correspondence Address: (52) U.S. Cl. .............................................................. 524/495 BRCH STEWART KOLASCH & BRCH PO BOX 747 FALLS CHURCH, VA 22040-0747 (US) (57) ABSTRACT A resin composition comprising a polyamide, a polyphe (21) Appl. No.: 11/203,245 nylene ether, an impact modifier, and a carbon type filler for (22) Filed: Aug. 15, 2005 an electrically conductive use, the filler residing in a phase of the polyphenylene ether. The resin composition of the Related U.S. Application Data present invention has excellent electrical conductivity, flu idity, and an excellent balance of a coefficient of linear (62) Division of application No. 10/240,793, filed on Oct. expansion and an impact resistance, and generation of fines 4, 2002, filed as 371 of international application No. caused by pelletizing thereof can be largely Suppressed PCT/JPO1/O1416, filed on Feb. 26, 2001. when processing of an extrusion thereof is conducted. Patent Application Publication Jan. 26, 2006 US 2006/0020077 A1 FIG. 1 FIG. 2 US 2006/0020077 A1 Jan. 26, 2006 ELECTRICALLY CONDUCTIVE RESIN 0009 From the above-described standpoint, the tech COMPOSITION AND PRODUCTION PROCESS nique wherein improvement in balance of a coefficient of THEREOF linear expansion and an impact resistance can be attained by using a composition Substantially not containing an inor 0001. -

Acute Poisoning: Understanding 90% of Cases in a Nutshell S L Greene, P I Dargan, a L Jones
204 REVIEW Postgrad Med J: first published as 10.1136/pgmj.2004.027813 on 5 April 2005. Downloaded from Acute poisoning: understanding 90% of cases in a nutshell S L Greene, P I Dargan, A L Jones ............................................................................................................................... Postgrad Med J 2005;81:204–216. doi: 10.1136/pgmj.2004.024794 The acutely poisoned patient remains a common problem Paracetamol remains the most common drug taken in overdose in the UK (50% of intentional facing doctors working in acute medicine in the United self poisoning presentations).19 Non-steroidal Kingdom and worldwide. This review examines the initial anti-inflammatory drugs (NSAIDs), benzodiaze- management of the acutely poisoned patient. Aspects of pines/zopiclone, aspirin, compound analgesics, drugs of misuse including opioids, tricyclic general management are reviewed including immediate antidepressants (TCAs), and selective serotonin interventions, investigations, gastrointestinal reuptake inhibitors (SSRIs) comprise most of the decontamination techniques, use of antidotes, methods to remaining 50% (box 1). Reductions in the price of drugs of misuse have led to increased cocaine, increase poison elimination, and psychological MDMA (ecstasy), and c-hydroxybutyrate (GHB) assessment. More common and serious poisonings caused toxicity related ED attendances.10 Clinicians by paracetamol, salicylates, opioids, tricyclic should also be aware that severe toxicity can result from exposure to non-licensed pharmaco- -
Toxicity Forecaster (Toxcasttm)
science in ACTION www.epa.gov/research INNOVATIVE RESEARCH FOR A SUSTAINABLE FUTURE Toxicity Forecaster (ToxCastTM) ADVANCING THE NEXT GENERATION OF CHEMICAL SAFETY EVALUATION Tens of thousands of chemicals are currently in commerce, and hundreds more are introduced every year. Because current chemical testing is expensive and time consuming, only a small fraction of chemicals have been fully evaluated for potential human health effects. Through its computational toxicology research (CompTox), the U.S. Environmental Protection Agency (EPA) is working to figure out how to change the current approach used to evaluate the safety of chemicals. CompTox research integrates advances in biology, biotechnology, chemistry, and computer science to identify important biological processes that may be disrupted by the chemicals and tracing those biological the potential to limit the number of of sources; including industrial and disruptions to a related dose and required laboratory animal-based consumer products, food additives, human exposure. The combined toxicity tests while quickly and and potentially “green” chemicals information helps prioritize efficiently screening large numbers that could be safer alternatives to chemicals based on potential human of chemicals. existing chemicals. These 2,000 health risks. Using CompTox, chemicals were evaluated in over thousands of chemicals can be The first phase of ToxCast, 700 high-throughput assays that evaluated for potential risk at a small appropriately called “Proof of cover a range of high-level cell cost in a very short amount of time. Concept”, was completed in responses and approximately 2009 and it evaluated over 300 300 signaling pathways. ToxCast A major part of EPA’s CompTox well studied chemicals (primarily research is the Toxicity Forecaster research is ongoing to determine pesticides) in over 500 high- which assays under what conditions (ToxCast™). -

Phthalic Anhydride Catalysts Brochure
Do you want to combine experience with innovation? BASF Phthalic Anhydride Catalysts are the market leading solution for your oxidation process. Introduction Phthalic Anhydride Catalysts 03 Table of Content BASF Catalysts Introduction BASF – We create Chemistry BASF Catalysts Introduction 03 As the world’s leading chemical company, BASF: Offers intelligent solutions and high-quality products BASF Research & Development 09 for most industrial challenges Uses new technologies to optimize additional market opportunities Phthalic Anhydride Catalysts Portfolio 12 Combines added value with environmental protection and social responsibility Phthalic Anhydride Catalysts for o-Xylene Oxidation 12 Phthalic Anhydride Catalysts for Naphthalene/Mixed 16 BASF at a Glance Support Technical Services 19 At BASF, we create chemistry for a sustainable future. We combine economic success with environmental protection and social responsibility. More than 117,000 employees in the BASF Group work on contributing to the success of our customers in nearly all sectors and almost every country in the world. Our portfolio is organized into six segments: Chemicals, Materials, Industrial Solutions, Surface Technologies, Nutrition & Care and Agricultural Solutions. BASF has companies in more than 90 countries. We operate six Verbund sites and 361 additional production sites world- wide. Our Verbund site in Ludwigshafen, Germany, is the world’s largest chemical complex owned by a single company that was developed as an integrated network. This was where the Verbund principle was originally established and continu- ously optimized before being implemented at additional sites. BASF's Catalysts division, headquartered in Iselin, New Jersey, is the world’s leading supplier of environmental and process catalysts. The group employs more than 5,000, with over 30 manufacturing sites worldwide. -

TOXICOLOGY and EXPOSURE GUIDELINES ______(For Assistance, Please Contact EHS at (402) 472-4925, Or Visit Our Web Site At
(Revised 1/03) TOXICOLOGY AND EXPOSURE GUIDELINES ______________________________________________________________________ (For assistance, please contact EHS at (402) 472-4925, or visit our web site at http://ehs.unl.edu/) "All substances are poisons; there is none which is not a poison. The right dose differentiates a poison and a remedy." This early observation concerning the toxicity of chemicals was made by Paracelsus (1493- 1541). The classic connotation of toxicology was "the science of poisons." Since that time, the science has expanded to encompass several disciplines. Toxicology is the study of the interaction between chemical agents and biological systems. While the subject of toxicology is quite complex, it is necessary to understand the basic concepts in order to make logical decisions concerning the protection of personnel from toxic injuries. Toxicity can be defined as the relative ability of a substance to cause adverse effects in living organisms. This "relative ability is dependent upon several conditions. As Paracelsus suggests, the quantity or the dose of the substance determines whether the effects of the chemical are toxic, nontoxic or beneficial. In addition to dose, other factors may also influence the toxicity of the compound such as the route of entry, duration and frequency of exposure, variations between different species (interspecies) and variations among members of the same species (intraspecies). To apply these principles to hazardous materials response, the routes by which chemicals enter the human body will be considered first. Knowledge of these routes will support the selection of personal protective equipment and the development of safety plans. The second section deals with dose-response relationships. -

Phthalic Anhydride
Right to Know Hazardous Substance Fact Sheet Common Name: PHTHALIC ANHYDRIDE Synonyms: 1,2-Benzendicarboxylic Anhydride; 1,3-Dioxophthalon CAS Number: 85-44-9 Chemical Name: 1,3-Isobenzofurandione RTK Substance Number: 1535 Date: August 2001 Revision: April 2010 DOT Number: UN 2214 Description and Use EMERGENCY RESPONDERS >>>> SEE LAST PAGE Phthallic Anhydride is a colorless to white, crystalline (sand- Hazard Summary like) or needle-shaped solid, or a pale yellow liquid when in Hazard Rating NJDOH NFPA molten form, with a strong, choking odor. It is used to make HEALTH - 3 plastics, resins, dyes, pharmaceuticals and fungicides. FLAMMABILITY - 1 REACTIVITY - 0 f ODOR THRESHOLD = 0.053 ppm CORROSIVE f Odor thresholds vary greatly. Do not rely on odor alone to POISONOUS GASES ARE PRODUCED IN FIRE determine potentially hazardous exposures. Hazard Rating Key: 0=minimal; 1=slight; 2=moderate; 3=serious; Reasons for Citation 4=severe f Phthallic Anhydride is on the Right to Know Hazardous Substance List because it is cited by OSHA, ACGIH, DOT, f Phthallic Anhydride can affect you when inhaled. NIOSH, DEP, IRIS, NFPA and EPA. f Contact can severely irritate and burn the skin and eyes. f This chemical is on the Special Health Hazard Substance f Inhaling Phthallic Anhydride can irritate the nose, throat List. and lungs. f Phthallic Anhydride may cause a skin allergy and an asthma-like allergy. f Phthallic Anhydride may damage the liver and kidneys. f Phthallic Anhydride is a DOT CORROSIVE. SEE GLOSSARY ON PAGE 5. Workplace Exposure Limits OSHA: The legal airborne permissible exposure limit (PEL) is FIRST AID 3 12 mg/m averaged over an 8-hour workshift. -

Ethylene Glycol Ingestion Reviewer: Adam Pomerlau, MD Authors: Jeff Holmes, MD / Tammi Schaeffer, DO
Pediatric Ethylene Glycol Ingestion Reviewer: Adam Pomerlau, MD Authors: Jeff Holmes, MD / Tammi Schaeffer, DO Target Audience: Emergency Medicine Residents, Medical Students Primary Learning Objectives: 1. Recognize signs and symptoms of ethylene glycol toxicity 2. Order appropriate laboratory and radiology studies in ethylene glycol toxicity 3. Recognize and interpret blood gas, anion gap, and osmolal gap in setting of TA ingestion 4. Differentiate the symptoms and signs of ethylene glycol toxicity from those associated with other toxic alcohols e.g. ethanol, methanol, and isopropyl alcohol Secondary Learning Objectives: detailed technical/behavioral goals, didactic points 1. Perform a mental status evaluation of the altered patient 2. Formulate independent differential diagnosis in setting of leading information from RN 3. Describe the role of bicarbonate for severe acidosis Critical actions checklist: 1. Obtain appropriate diagnostics 2. Protect the patient’s airway 3. Start intravenous fluid resuscitation 4. Initiate serum alkalinization 5. Initiate alcohol dehydrogenase blockade 6. Consult Poison Center/Toxicology 7. Get Nephrology Consultation for hemodialysis Environment: 1. Room Set Up – ED acute care area a. Manikin Set Up – Mid or high fidelity simulator, simulated sweat if available b. Airway equipment, Sodium Bicarbonate, Nasogastric tube, Activated charcoal, IV fluid, norepinephrine, Simulated naloxone, Simulate RSI medications (etomidate, succinylcholine) 2. Distractors – ED noise For Examiner Only CASE SUMMARY SYNOPSIS OF HISTORY/ Scenario Background The setting is an urban emergency department. This is the case of a 2.5-year-old male toddler who presents to the ED with an accidental ingestion of ethylene glycol. The child was home as the father was watching him. The father was changing the oil on his car.