Chronic Care Management Critical Access Hospital Administrator's
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Voorbeeld Voor Tabs
1 GENEALOGY updated Dec. 2018 LEVANTINE BRANCHES VAN LENNEP DE HOCHEPIED DE LA FONTAINE LEYTSTAR BY HENRICK S. VAN LENNEP 2 INTRODUCTION The Van Lennep genealogy Smyrna Branch is a translation of a part of the book Genealogie van de familie Van Lennep by Henrick van Lennep. A book of 411 pages published in the Dutch language in December 2007. This book can be ordered from Uitgeverij Verloren, Hilversum, [email protected] at a price of Euro 19,- plus postal and transfer cost. After the publication in 2007 of this book many new details about the Smyrna Branch of the Van Lennep family were collected and included in this publication. Also the genealogies of the Levantine Branches of the families De Hochepied, De la Fontaine and Leytstar are inserted in this book. The biographical parts of the Van Lennep genealogy were translated by Alfred P. van Lennep. Willem Daniels was so kind as to correct the whole translation of the Van Lennep genealogy Smyrna Branch and to give some important suggestions. The Van Lennep genealogy Smyrna Branch and the three other genealogies were published together in a limited edition in bookform on the occasion of the Levantine Heritage Symposium in Izmir from 2 to 5 November 2010. Please send corrections and additional information to [email protected] 3 CONTENTS First six generations Van Lennep page 4 Merchant in Smyrna (David George van Lennep) page 6 An admirer of Mrs.van Lennep (Anna Maria van Lennep-Leytstar) page 8 Jacob van Lennep & Co. page 16 Scheme A. page 19 Painter and Sculptor (Eveline Maud Hildevan Lennep) page 22 Scheme B. -
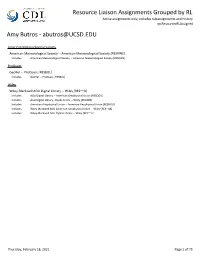
Resource Liaison Assignments Grouped by RL Active Assignments Only, Includes Subassignments and History Rptresourcexrlassigned Amy Butros - [email protected]
Resource Liaison Assignments Grouped by RL Active assignments only, includes subassignments and history rptResourcexRLAssigned Amy Butros - [email protected] American Meteorological Society American Meteorological Society -- American Meteorological Society [RESRWE] Includes American Meteorological Society -- American Meteorological Society [RESRWE] ProQuest GeoRef -- ProQuest [RESBUL] Includes GeoRef -- ProQuest [RESBUL] Wiley Wiley-Blackwell AGU Digital Library -- Wiley [RES~~A] Includes AGU Digital Library -- American Geophysical Union [RESQGU] Includes AGU Digital Library - Books Series -- Wiley [RESOB9] Includes American Geophysical Union -- American Geophysical Union [RESRGU] Includes Wiley-Blackwell AGU American Geophysical Union -- Wiley [RES~OA] Includes Wiley-Blackwell AGU Digital Library -- Wiley [RES~~A] Thursday, February 18, 2021 Page 1 of 75 Resource Liaison Assignments Grouped by RL Active assignments only, includes subassignments and history rptResourcexRLAssigned Andrea Duda - [email protected] American Institute of Physics Scitation Publications -- American Institute of Physics [RESRQS] Includes Acoustical Society of America Publications -- Acoustical Society of America [RESRAZ] Includes AIP Conference Proceedings -- American Institute of Physics [RESAEO] Includes American Association of Physicists in Medicine (AAPM) Publications -- American Association of Physicists in Medicine [RESPHY] Includes American Association of Physics Teachers (AAPT) Publications -- American Association of Physics Teachers [RESPHQ] Includes -

Download Thesis
This electronic thesis or dissertation has been downloaded from the King’s Research Portal at https://kclpure.kcl.ac.uk/portal/ Biomarker, Metabolomics and Doping A Novel Approach to Detect Drug Misuse Wang, Yaoyao Awarding institution: King's College London The copyright of this thesis rests with the author and no quotation from it or information derived from it may be published without proper acknowledgement. END USER LICENCE AGREEMENT Unless another licence is stated on the immediately following page this work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International licence. https://creativecommons.org/licenses/by-nc-nd/4.0/ You are free to copy, distribute and transmit the work Under the following conditions: Attribution: You must attribute the work in the manner specified by the author (but not in any way that suggests that they endorse you or your use of the work). Non Commercial: You may not use this work for commercial purposes. No Derivative Works - You may not alter, transform, or build upon this work. Any of these conditions can be waived if you receive permission from the author. Your fair dealings and other rights are in no way affected by the above. Take down policy If you believe that this document breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. Download date: 07. Oct. 2021 Biomarker, Metabolomics and Doping: A Novel Approach to Detect Drug Misuse By Yaoyao Wang A thesis submitted to King’s College London in partial fulfilment for the degree of Doctor of Philosophy Supervisors: Dr Cristina Legido-Quigley Professor David Cowan Institute of Pharmaceutical Science Faculty of Life Sciences & Medicine King’s College London 2016 Acknowledgements Acknowledgements First of all, I would like to thank my supervisor, Dr Cristina Legido-Quigley, for all of her advice and guidance throughout the project. -

2013-14 University of the Pacific
Pharmacy Programs Pharmacy Mission experiences in health care settings. More specific program information is provided in the section on the Doctor of Pharmacy program. Our mission is to provide an exemplary educational experience that Accreditation leads to highly competent and practice-ready caring pharmacists and pharmaceutical scientists who are accountable for improving the health Organized in 1955, the Thomas J. Long School of Pharmacy and Health and well-being of society. The programs seek to advance knowledge Sciences is a member of the American Association of Colleges of through collaborative education, science, research, service, patient care Pharmacy, and its Doctor of Pharmacy Program is fully accredited by and advocacy. The school strives to achieve academic and professional the Accreditation Council for Pharmacy Education (ACPE). Accreditation excellence. information can be found online at http://www.acpe-accredit.org/ or by contacting: By virtue of their innate abilities and their education and experiences at Pacific, our graduates are: ACPE 20 North Clark Street, Suite 2500 • accomplished and compassionate practitioners dedicated to improving Chicago, IL 60602-5109 inpatient care in traditional and emerging roles in all practice settings; Phone: (312) 664-3575 • capable of critical thinking, problem solving and strong individual and Fax: (312) 664-4652 team leadership; E-mail: [email protected] • filled with the desire, knowledge and skills to serve their diverse Pharmacy Licensure communities and professions locally, regionally, nationally and globally; For California pharmacy licensure requirements see http:// • able to advance the profession of pharmacy by providing high quality www.pharmacy.ca.gov/ or contact: health care, innovative practice models and leadership in healthcare policy to meet the needs of an increasingly diverse population; the California State Board of Pharmacy 1625 N. -

Btk Inhibition Treats TLR7/IFN Driven Murine Lupus
Clinical Immunology 164 (2016) 65–77 Contents lists available at ScienceDirect Clinical Immunology journal homepage: www.elsevier.com/locate/yclim Btk inhibition treats TLR7/IFN driven murine lupus Andrew T. Bender a,⁎, Albertina Pereira a,KaiFua,EileenSamya,YinWua, Lesley Liu-Bujalski b, Richard Caldwell b, Yi-Ying Chen b,HuiTianb, Federica Morandi c,JaredHeadc, Ursula Koehler d, Melinda Genest a, Shinji L. Okitsu a, Daigen Xu a, Roland Grenningloh a a TIP Immunology, EMD Serono Research and Development Institute, 45A Middlesex Turnpike, Billerica, MA 01821, USA b Medicinal Chemistry, EMD Serono Research and Development Institute, 45A Middlesex Turnpike, Billerica, MA 01821, USA c Biomolecular Pharmacology, EMD Serono Research and Development Institute, 45A Middlesex Turnpike, Billerica, MA 01821, USA d TIP Immunology Merck Serono, Frankfurter Strasse 250, A031/101 64293 Darmstadt, Germany article info abstract Article history: Bruton's tyrosine kinase (Btk) is expressed in a variety of immune cells and previous work has demonstrated that Received 18 December 2015 blocking Btk is a promising strategy for treating autoimmune diseases. Herein, we utilized a tool Btk inhibitor, Received in revised form 22 January 2016 M7583, to determine the therapeutic efficacy of Btk inhibition in two mouse lupus models driven by TLR7 acti- accepted with revision 23 January 2016 vation and type I interferon. In BXSB-Yaa lupus mice, Btk inhibition reduced autoantibodies, nephritis, and mor- Available online 25 January 2016 tality. In the pristane-induced DBA/1 lupus model, Btk inhibition suppressed arthritis, but autoantibodies and the IFN gene signature were not significantly affected; suggesting efficacy was mediated through inhibition of Fc re- Keywords: Lupus ceptors. -

Chicago Medical School 2015-2016 Academic Catalog
Chicago Medical School 2015-2016 Academic Catalog Rosalind Franklin University of Medicine and Science and the Chicago Medical School reserve the right to change, at any time and without notice, their requirements, regulations, course and program offerings, fees, charges, and other matters addressed in this catalog. RFUMS must reserve the right to modify or terminate programs described herein. However, modification of program requirements will not adversely affect those students already enrolled in a program, nor will termination of a program affect anything other than the closure of admission thereto. v. July 31, 2015 Chicago Medical School 2015-2016 Academic Catalog 1 TABLE OF CONTENTS General Content Letter from the Dean 4 Introduction 5 History 5 Mission 6 Vision 7 Core Competencies 7 Accreditation 7 Equal Opportunity 8 Location 8 Application Procedure 8 AMCAS 8 MCAT 8 Admission Requirements 9 Admissions Committee Procedures 9 Advanced Standing 10 Non-Immigrant International Students 10 Academic Performance Standards and Measurement 10 Grading 10 Professionalism Expectations 11 Student Records and Transcripts 11 Leave of Absence 11 Tuition and Other Educational Expenses 12 Tuition and Fee Payment Policy 12 Refunds and Withdrawals 12 Health Care and Health Insurance 13 Disability Insurance 13 Students with Disabilities 13 Technical Standards 13 Requirements for the MD Degree 15 Requirements for the Combined MD/PhD Degree 15 MD with Distinction in Research Program 16 MD with Distinction in Basic Science 16 Educational Competencies and -

The Journal. College of Medicine Yearbook
University of Vermont ScholarWorks @ UVM University of Vermont College of Medicine University Libraries Yearbooks 1960 The ourJ nal. College of Medicine Yearbook University of Vermont Follow this and additional works at: https://scholarworks.uvm.edu/dmlyearbook Part of the Medicine and Health Sciences Commons Recommended Citation University of Vermont, "The ourJ nal. College of Medicine Yearbook" (1960). University of Vermont College of Medicine Yearbooks. 6. https://scholarworks.uvm.edu/dmlyearbook/6 This Book is brought to you for free and open access by the University Libraries at ScholarWorks @ UVM. It has been accepted for inclusion in University of Vermont College of Medicine Yearbooks by an authorized administrator of ScholarWorks @ UVM. For more information, please contact [email protected]. VERMONT COLLEGE OF MEDICINE vt. 1960 Med. Hist. W 19 U58p 1960 CHARLES A. DANA MEDICAL LB3ARY umîv:..3;ïy o? vûrmont BURLI KG ¡"ON, VERMONT 05405 SjTfa Journal OloLfA of UNIVERSITY OF VERMONT COLLEGE OF MEDICINE ÎÊÊÊÊmà^L ARTHUR A. GLADSTONE, M.D., F.A.C.S., F.A.Pr.S. In recognition of the kind friendship and wise counsel he has offer- ed so many students; of the perspicuous guidance he has given to the expansion of the staff and facilities of this medical center; and of the example he has provided of the selfless administrator, warm human being, and devoted physician - - the Class of 1960 dedicates this book. SENIORS ETIOLOGY The Class of 1960 of the University of Vermont College of Medicine came together for the first time in the fall of 1956. We represented the products of many Eastern states including Maine, New Hampshire, Massachusetts, Connecticut, New York, and, of course, Vermont. -

Classics Department and Offers USC Classicists a Window on the Ancient World
Fall 2003 William Thalmann, Amy Richlin and Thomas Habinek department is often very contempo- rary. Last spring, William Thalmann’s course on Homer’s “The Iliad” coin- cided with the onset of the U.S. war in Iraq. “As a result,” Thalmann says, “students ‘got’ this text like I’ve never seen before. On many levels, the poem is about how individuals come to terms with controlling and eradicating violence.” In the Classroom The comprehensive study of Latin and Greek is the foundation of the classics department and offers USC classicists a window on the ancient world. Thalmann, who began learn- ing Latin when he was 11 and was fluent in Greek by his 14th birthday, says John Milton’s “Paradise Lost” is one of his favorite texts to teach. “Language is a wonderful way into the ancient world. When you just read the translation, there is a real barrier between you and the text. There is a wonderful analytical aspect to learning the languages. It carries over to the way you think, read and write,” he says. Thalmann and Habinek are revising our understand- ing of the relationship between oral and written performance through their research on Latin and Greek lit- erature respectively. Classics professors and their grad- Classics: Back to the Future uate students often find themselves in the midst of unusual research projects that link two seemingly ith a roster of only eight faculty, the USC College classics guage, philosophy and archaeology unrelated topics. Take associate pro- department is small but mighty. As its professors fessor Vincent Farenga’s study of continuously engage ancient examples to explain communication and psychology. -

Chicago Medical School ACADEMIC CATALOGUE 2010-2011
Chicago Medical School ACADEMIC CATALOGUE 2010-2011 1 CHICAGO MEDICAL SCHOOL Academic Catalogue 2010 – 2011 Rosalind Franklin University of Medicine and Science and the Chicago Medical School reserve the right to change, at any time and without notice, their requirements, regulations, course and program offerings, fees, charges, and other matters addressed in this catalogue. RFUMS must reserve the right to modify or terminate programs described herein. However, modification of program requirements will not adversely affect those students already enrolled in a program, nor will termination of a program affect anything other than the closure of admission thereto. Chicago Medical School 2 TABLE OF CONTENTS General Content Letter from the Dean ............................................................................................................................................. 4 Introduction ........................................................................................................................................................... 5 History ................................................................................................................................................................... 5 Mission .................................................................................................................................................................. 6 Vision ................................................................................................................................................................... -
Dr. Richard J. Charnigo, Jr
1 Dr. Richard J. Charnigo, Jr. Curriculum Vitae – July 2020 Basic Information Contact Information Mail: Multidisciplinary Science Building 325a 725 Rose Street, University of Kentucky Lexington, Kentucky 40536-0082 E-Mail: [email protected] Internet: http://www.richardcharnigo.net Employment (University of Kentucky) Professor 2013- I hold this rank both in my primary appointment (Department of Biostatistics, College of Public Health) and in my secondary appointment (Dr. Bing Zhang Department of Statistics, College of Arts and Sciences). Some other information: Chair of Biostatistics, 1/1/2017-8/15/2017 University Research Professor, 2014-2015 Veterans Affairs WOC Appointee, 2014- Associate Professor 2009-2013 Assistant Professor 2003-2009 Graduate Faculty Status (University of Kentucky) Full Member Data Science 2020- Epidemiology and Biostatistics 2010- Statistics, Preventive Medicine (Public Health) 2009- Education Ph.D. in Statistics 1999-2003 Case Western Reserve University Dissertation: “Testing Homogeneity in Finite Mixtures and a Semi-Local Paradigm for Wavelet Denoising” Advisor: Jiayang Sun M.S. in Mathematics 1997-1999 Case Western Reserve University B.S. in Mathematics 1994-1997 Case Western Reserve University Minor fields: Statistics and Economics Research Interests, Publications, and Presentations Selected Research Interests (historical and current) Mixture modeling + application to perinatal and microarray data analyses Dimension reduction + application to discovering gene-gene interactions Nonparametric regression + application to nanoparticle characterization and imaging Cardiovascular health 2 Publications 1. Smith, Toni; Charnigo, Richard (2002). “On the Nonoptimality of the Compensation System in Major League Baseball.” Compensation and Working Conditions: Volume 6, pp. 19 – 25. 2. Charnigo, Richard; Sun, Jiayang (2004). “Testing for Homogeneity in Mixture Distributions via the L2 Distance Between Competing Models.” Journal of the American Statistical Association: Volume 99, pp. -

Census Men Ready to Start Making Calls Here April 1 Field
fah in almost circular ,ording to the Ency- Nature has given us two Itannlea. ears but only tole mouth. VI hell IMO Meal combine BENJAMIN DISRAELI the g I must lie...late. — EDMUND 111111:e; re HOUSE, 0 SEE, WA/RING, / ANDOVER, MASSACHUSETTS, MARCH 30, 1950 PRICE, 5 CENTS Census Men Ready To Start Making ipx Calls Here April 1 Will Have Many Questions To Ask About Each Individual But All Are Authorized By The Government A group of 1.1 census takers will start Apr. 1 in Andover on a Plan Observance house to house canvass to obtain information for Uncle Sam. Of Memorial Day The enumerators will be operat- ing under Arthur E. McCabe of Committee Considers Porter rd., district supervisor, with Some Revision Of The Thome A. Welch. crew leader, in direct charge of the Andover op- Former Procedure erations. The first meeting of the Memor- The questions they will ask are ial Day Observances committee standardized. There will be no was held Monday night in the post snoopers to ask questions not rooms of the American Legion. authorized by the government. The committee is made up of mem- Each enumerator will carry cre- bers of the four veterans organiza- dentials and the public is urged to tions in Andover and the following insist upon seeing them before in- representatives of each unit at- viting anyone into the house. tended the meeting: for the Vet- There are about 45 basic ques- erans of Foreign Wars; Comman- tions in the 1950 population cen- der Thomas Eldred, Commander- sus but of these only eight will elect William Hulse, Vice Com- be asked about all individuals. -

Download PDF of This Page
PHARMACY PROGRAMS semesters, which is completed in approximately two and two-thirds Pharmacy Mission years. This has been made possible by utilizing the summer months for Our mission is to provide an exemplary educational experience that instruction, thus providing the same number of instructional semesters leads to highly competent and practice-ready caring pharmacists and as in four academic years. The first two years of the program include on pharmaceutical scientists who are accountable for improving the health campus course work plus introductory pharmacy practice experiences. and well-being of society. The programs seek to advance knowledge The final year of the program consists of advanced pharmacy practice through collaborative education, science, research, service, patient care experiences in health care settings. More specific program information is and advocacy. The school strives to achieve academic and professional provided in the section on the Doctor of Pharmacy program. excellence. Accreditation By virtue of their innate abilities and their education and experiences at Organized in 1955, the Thomas J. Long School of Pharmacy and Health Pacific, our graduates are: Sciences is a member of the American Association of Colleges of Pharmacy, and its Doctor of Pharmacy Program is fully accredited by • accomplished and compassionate practitioners dedicated to the Accreditation Council for Pharmacy Education (ACPE). Accreditation improving inpatient care in traditional and emerging roles in all information can be found online at