DSM-5 Part 2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
SOMATIC SYMPTOM, BODILY DISTRESS and RELATED DISORDERS in CHILDREN and ADOLESCENTS 2019 Edition
IACAPAP Textbook of Child and Adolescent Mental Health Chapter CHILD PSYCHIATRY & PEDIATRICS I.1 SOMATIC SYMPTOM, BODILY DISTRESS AND RELATED DISORDERS IN CHILDREN AND ADOLESCENTS 2019 edition Olivia Fiertag, Sharon Taylor, Amina Tareen & Elena Garralda Olivia Fiertag MBChB, MRCPsych, PGDip CBT Consultant Child and Adolescent Psychiatrist. Honorary Clinical Researcher, HPFT NHS Trust & collaboration with Imperial College London, UK Conflict of interest: none declared Sharon Taylor BSc, MBBS, MRCP, MRCPsych, CASLAT, PGDip Consultant Child and Adolescent Psychiatrist CNWL Foundation NHS Trust & Honorary Senior Clinical Lecturer Imperial College London, UK. Joint Program Director, St Mary’s Child Sick Girl. Psychiatry Training Scheme Christian Krogh, Conflict of interest: none (1880/1881) National declared Gallery of Norway This publication is intended for professionals training or practicing in mental health and not for the general public. The opinions expressed are those of the authors and do not necessarily represent the views of the Editor or IACAPAP. This publication seeks to describe the best treatments and practices based on the scientific evidence available at the time of writing as evaluated by the authors and may change as a result of new research. Readers need to apply this knowledge to patients in accordance with the guidelines and laws of their country of practice. Some medications may not be available in some countries and readers should consult the specific drug information since not all dosages and unwanted effects are mentioned. Organizations, publications and websites are cited or linked to illustrate issues or as a source of further information. This does not mean that authors, the Editor or IACAPAP endorse their content or recommendations, which should be critically assessed by the reader. -

Somatoform Disorders – September 2017
CrackCast Show Notes – Somatoform Disorders – September 2017 www.canadiem.org/crackcast Chapter 103 – Somatoform disorders Episode overview 1. List 5 somatic symptom and related disorders 2. List 5 common presentations of conversion disorders 3. List 6 ddx of somatic symptom disorder Wisecracks 1. List 6 organic diseases that may be mistaken for somatoform disorders 2. Describe the treatment goals of somatoform disorders Somatoform disorders as a diagnosis has been eliminated from the DSM-5! The patient with functional neurological symptom disorder, what was termed conversion disorder previously, requires a careful and complete neurological examination. Rather than miss the subtle presentation of a neurological disorder, it may be appropriate to perform imaging and obtain neurological and psychiatric consultation. Do not assume that the patient with neurological deficits has a psychiatric disorder. Success with the SSD patient depends on establishing rapport with the patient and legitimizing their complaints to avoid a dysfunctional physician-patient interaction. • Avoid telling the SSD patient “it is all in your head” or “there is nothing wrong with you.” These patients are very sensitive to the idea that their suffering is being dismissed. • A useful approach is to discuss recent stressors with the patient and suggest to them that at times our bodies can be smarter than we are, telling us with physical symptoms that we need assistance. This approach alone may transform the ED visit from a standoff between physician and patient, to a grateful patient who develops greater insight and is amenable to referral. • Avoid prescribing unnecessary or addictive medications to the SSD patient. • If you suspect a diagnosis of SSD, refer the patient to primary care or psychiatry for further evaluation and treatment. -

Psychopathology and Somatic Complaints: a Cross-Sectional Study with Portuguese Adults
healthcare Article Psychopathology and Somatic Complaints: A Cross-Sectional Study with Portuguese Adults Joana Proença Becker 1,*, Rui Paixão 1 and Manuel João Quartilho 2 1 Faculty of Psychology and Education Sciences, University of Coimbra, 3000-115 Coimbra, Portugal; [email protected] 2 Faculty of Medicine, University of Coimbra, 3000-548 Coimbra, Portugal; [email protected] * Correspondence: [email protected] or [email protected]; Tel.: +351-910741887 Abstract: (1) Background: Functional somatic symptoms (FSS) are physical symptoms that cannot be fully explained by medical diagnosis, injuries, and medication intake. More than the presence of unexplained symptoms, this condition is associated with functional disabilities, psychological distress, increased use of health services, and it has been linked to depressive and anxiety disorders. Recognizing the difficulty of diagnosing individuals with FSS and the impact on public health systems, this study aimed to verify the concomitant incidence of psychopathological symptoms and FSS in Portugal. (2) Methods: For this purpose, 93 psychosomatic outpatients (91.4% women with a mean age of 53.9 years old) and 101 subjects from the general population (74.3% women with 37.8 years old) were evaluated. The survey questionnaire included the 15-item Patient Health Questionnaire, the 20-Item Short Form Survey, the Brief Symptom Inventory, the Depression, Anxiety and Stress Scale, and questions on sociodemographic and clinical characteristics. (3) Results: Increases in FSS severity were correlated with higher rates of depression, anxiety, and stress symptoms. The findings also suggest that increased rates of FSS are associated with lower educational level and Citation: Becker, J.P.; Paixão, R.; female gender. -

DEVELOPMENTAL DELAYS and REGRESSIONS Selective Mutism
CHALLENGING CASE: DEVELOPMENTAL DELAYS AND REGRESSIONS Selective Mutism* CASE Dr. Martin T. Stein Peter’s parents made an appointment with his pe- Selective mutism is an acquired disorder of inter- diatrician because of their increasing concern about personal communication in which a child does not his refusal to speak. After approximately 2 weeks speak in one or more environments where commu- following the start of a new preschool, Peter, 4 years nication typically occurs. These children most often 10 months old, refused to speak to other children or refuse to speak in school and to adults outside the the teacher. During the first week of school, he found home. Some children with selective mutism will not it difficult to separate from his mother or father. He speak to any child; others will use speech with only would cry and cling to them while asking to go a few other children. Parents report normal speech home. This difficult separation experience gradually within the home with at least one parent and some- subsided by the beginning of the third week and times with siblings. The onset of selective mutism is corresponded with the onset of mute behavior. At usually in the preschool or early school age period of home, he spoke only to his mother, with a clear development; often, it is associated with the start of speech pattern and full sentences. He limited his school. responses to his father or two older siblings with Although this disorder is uncommon (1% among body gestures. He appeared to hear well and under- children seen in mental health centers; 0.1% in the stand verbal directions. -
WHAT Is Selective Mutism?
WHAT is Selective Mutism? A GUIDE to Helping Parents, Educators and Treatment professionals Understand Selective Mutism as a Social Communication Anxiety Disorder Do you know a child who is mute, barely whispers to few others in school or other social settings, but is able to speak when comfortable such as at home? If so, this child may be suffering from Selective Mutism. “Copyright © [2013] Dr. Elisa Shipon-Blum and Selective Mutism Anxiety Research and Treatment Center, Inc. (SMart Center) – www.selectivemutismcenter.org. 215-887-5748 [email protected] All rights reserved. Selective Mutism is a complex childhood anxiety disorder characterized by a child’s inability to speak and communicate in a socially appropriate manner in select social settings, such as school. These children are able to speak and communicate in settings where they are comfortable, secure and relaxed, such as at home. To meet the diagnostic criteria for Selective Mutism (SM) a child has to be able to speak in at least one setting and be mute in at least one other setting. The typical presentation is the ‘timid’ child who can speak and act socially appropriate with family members, close peers and very familiar relatives, yet is mute or barely whispers to a few others in school or perhaps when addressed in public settings such as restaurants or stores More than 90% of children with Selective Mutism also have social anxiety. This disorder is quite debilitating and painful to the child. Children and adolescents with Selective Mutism have an actual FEAR of speaking and of social interactions where there is an expectation to speak and communicate. -

1 Serious Emotional Disturbance (SED) Expert Panel
Serious Emotional Disturbance (SED) Expert Panel Meetings Substance Abuse and Mental Health Services Administration (SAMHSA) Center for Behavioral Health Statistics and Quality (CBHSQ) September 8 and November 12, 2014 Summary of Panel Discussions and Recommendations In September and November of 2014, SAMHSA/CBHSQ convened two expert panels to discuss several issues that are relevant to generating national and State estimates of childhood serious emotional disturbance (SED). Childhood SED is defined as the presence of a diagnosable mental, behavioral, or emotional disorder that resulted in functional impairment which substantially interferes with or limits the child's role or functioning in family, school, or community activities (SAMHSA, 1993). The September and November 2014 panels brought together experts with critical knowledge around the history of this federal SED definition as well as clinical and measurement expertise in childhood mental disorders and their associated functional impairments. The goals for the two expert panel meetings were to operationalize the definition of SED for the production of national and state prevalence estimates (Expert Panel 1, September 8, 2014) and discuss instrumentation and measurement issues for estimating national and state prevalence of SED (Expert Panel 2, November 12, 2014). This document provides an overarching summary of these two expert panel discussions and conclusions. More comprehensive summaries of both individual meetings’ discussions and recommendations are found in the appendices to this summary. Appendix A includes a summary of the September meeting and Appendix B includes a summary of the November meeting). The appendices of this document also contain additional information about child, adolescent, and young adult psychiatric diagnostic interviews, functional impairment measures, and shorter mental health measurement tools that may be necessary to predict SED in statistical models. -

Days out of Role and Somatic, Anxious-Depressive, Hypo-Manic, and Psychotic-Like Symptom Dimensions in a Community Sample of Young Adults Jacob J
Crouse et al. Translational Psychiatry (2021) 11:285 https://doi.org/10.1038/s41398-021-01390-y Translational Psychiatry ARTICLE Open Access Days out of role and somatic, anxious-depressive, hypo-manic, and psychotic-like symptom dimensions in a community sample of young adults Jacob J. Crouse 1, Nicholas Ho 1,JanScott 1,2,3,4, Nicholas G. Martin 5, Baptiste Couvy-Duchesne 5,6,7, Daniel F. Hermens 8,RichardParker 5, Nathan A. Gillespie 9, Sarah E. Medland 5 and Ian B. Hickie 1 Abstract Improving our understanding of the causes of functional impairment in young people is a major global challenge. Here, we investigated the relationships between self-reported days out of role and the total quantity and different patterns of self-reported somatic, anxious-depressive, psychotic-like, and hypomanic symptoms in a community-based cohort of young adults. We examined self-ratings of 23 symptoms ranging across the four dimensions and days out of role in >1900 young adult twins and non-twin siblings participating in the “19Up” wave of the Brisbane Longitudinal Twin Study. Adjusted prevalence ratios (APR) and 95% confidence intervals (95% CI) quantified associations between impairment and different symptom patterns. Three individual symptoms showed significant associations with days out of role, with the largest association for impaired concentration. When impairment was assessed according to each symptom dimension, there was a clear stepwise relationship between the total number of somatic symptoms and the 1234567890():,; 1234567890():,; 1234567890():,; 1234567890():,; likelihood of impairment, while individuals reporting ≥4 anxious-depressive symptoms or five hypomanic symptoms had greater likelihood of reporting days out of role. -

Paranoid – Suspicious; Argumentative; Paranoid; Continually on the Lookout for Trickery and Abuse; Jealous; Tendency to Blame Others; Cold and Humorless
Personality Disturbance Gathering, nr.49 (key to possible disturbances) Every person may be used only once, except “by proxy” will overlap another person/condition, and there is one condition which will not be assigned to characters. 1. Agoraphobia – Fear of being out in the open or in public places; nervous; anxious 2. Autophobia/Monophobia – Extreme dislike or anger of oneself, or of an ethnic group from which one descends. 3. Anti-Social Personality Disorder – Failure to conform to societal norms; lack of remorse or indifferent; impulsivity or failure to plan ahead; consistent irresponsibility; deceitfulness. 4. Avoidant Personality Disorder – Socially awkward; fear of criticism, disapproval or rejection; views self as socially inept; reluctant to take personal risks or to engage in new activities because they may prove embarrassing. 5. Body Dysmorphic Disorder – A perceived defect of oneself. 6. Borderline – Very unstable relationships; erratic emotions; self-damaging behavior; impulsive; unpredictable aggressive and sexual behavior; sometimes similar to Autophobia/Monophobia; easily angered. 7. Brief Psychotic Disorder – Delusions, hallucination, disorganized speech or catatonic behavior which last between one and four weeks. 8. “…by Proxy” – Any condition where someone uses another (adult, children) to achieve their needs. 9. Cognitive Dissonance – the wrestling with opposing viewpoints in our mind, and determine which decision to make; our effort to fundamentally strive for harmony in our thinking. 10. Compulsive – Perfectionists, preoccupied with details, rules and schedules; more concerned about work than pleasure; serious and formal; cannot express tender feelings. 11. Compulsive Hoarding – Excessive acquisition of possessions, and failure to use or discard them, even if the items are worthless, hazardous or unsanitary. -

Selective Mutism and the Anxiety Spectrum – a Long-Term Case Report
Cartas aos Editores 172 K-SADS), she met diagnostic criteria for Separation Anxiety Financiamento: Inexistente Disorder (in the past), current diagnosis of Specific Phobia. She Conflito de interesses: Inexistente didn’t have any other anxious (including social anxiety), affective or psychotic symptoms. Before her referral, she was treated with psychodynamic Referências therapy and took paroxetine (20 mg/daily) for 12 months without 1. Aggege S. Sem hospícios, morrem mais doentes mentais. O Globo,Rio de Janeiro. 2007 09 dez/set; Seção O País: 14. improvement. At our service, she was treated with cognitive- 2. Datasus. Informações de Saúde: Estatísticas vitais - mortalidade behavioral therapy (CBT) for 10 months with poor outcome. e nascidos vivos. citado 10 dez 2007. Disponível em: http:www. Then, CBT was associated with sertraline (150 mg/daily). After datasus.gov.br. 3 months, the level of anxiety on CBT exposures lowered. She 3. Laurenti R, Mello Jorge MHP, Gotlieb SLD. A confiabilidade dos dados started to shout when playing handball, she talks louder to de mortalidade e morbidade por doenças crônicas não-transmissíveis. Cienc Saude Coletiva. 2004;9(4):909-20. her mother in public places, and talks to friends through lips 4. Mello Jorge MHP, Gotlieb SLD, Laurenti R. O sistema de informações sobre movements. Though she isn’t talking to many people yet, she mortalidade: problemas e propostas para o seu enfrentamento I — Mortes is clearly less anxious. por causas naturais. Rev Bras Epidemiol. 2002;5(2):197-211. There is some controversy whether SM is an anxiety disorder 5. Sampaio ALP, Caetano D. Mortalidade em pacientes psiquiátricos: (AD) or an independent diagnosis. -

Selective Mutism: a Three-Tiered Approach to Prevention and Intervention
53 Selective Mutism: A Three-Tiered Approach to Prevention and Intervention R.T. Busse and Jenna Downey, Chapman University Selective mutism is a rare anxiety disorder that prevents a child from speaking at school or other community settings, and can be detrimental to a child’s social development. School psy- chologists can play an important role in the prevention and treatment of selective mutism. As an advocate for students, school psychologists can work with teachers, parent caregivers, speech pathologists, and other support staff toward helping children who may develop or have selec- tive mutism. The purpose of this article is to present school-based prevention and intervention approaches within a three-tiered approach that may reduce the incidence and severity of selec- tive mutism. We present theories and research on the etiology and prevalence of the disorder, followed by a review of intervention methods and research at each tier. Based on the theoretical and research literature base, we conclude that early intervention may result in the prevention and amelioration of many occurrences of selective mutism. KEYWORDS: Selective Mutism, Childhood Anxiety Disorders, Social Phobia, Prevention, Treatment The purpose of this article is to present school-based prevention and intervention approaches within a three-tiered approach that may reduce the prevalence and severity of selective mutism. Children with selective mutism (SM) experience a “consistent failure to speak in specific social situations (in which there is an expectation for -

Selective Mutism
Selective Mutism Communication Profile In comfortable situations, children with selective mutism usually demonstrate age- appropriate language and communication skills. If a child is not in a comfortable environment, The current Diagnostic and Statistical Manual of he or she generally will be unable to speak at all. Mental Disorders (DSM.5) classifies selective With select individuals, the child may be able to mutism as an anxiety disorder. speak at a whisper. Characteristics include: In specific situations leading to mutism, a child may: Consistent failure to speak in specific Be motionless or expressionless social situations (in which there is an Avoid eye contact expectation for speaking, such as at school) despite speaking in other situations. Have stiff posture or body language Be slow to respond (even nonverbally) or Not speaking interferes with school or have trouble initiating work, or with social communication. Withdraw or turn away Lasts at least 1 month (not limited to the first month of school). Communication Concerns Failure to speak is not due to the lack of Children with selective mutism vary in their knowledge with the spoken language use of nonverbal communication, such as that is required in a social situation. pointing or using pictures. Though some may use gestures or facial expressions, others may Not due to a communication disorder seem paralyzed. (e.g., stuttering) and it does not only This poses significant health and safety occur during the course of a pervasive concerns, because a child may not be able to developmental disorder, schizophrenia, or express their needs. For example, children at other psychotic disorders. -
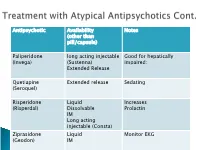
Antipsychotic Availability (Other Than Pill/Capsule) Notes Paliperidone
Antipsychotic Availability Notes (other than pill/capsule) Paliperidone long acting injectable Good for hepatically (Invega) (Sustenna) impaired; Extended Release Quetiapine Extended release Sedating (Seroquel) Risperidone Liquid Increases (Risperdal) Dissolvable Prolactin IM Long acting injectable (Consta) Ziprasidone Liquid Monitor EKG (Geodon) IM Supportive Psychotherapy Club House ACT services NAMI Vocational Rehab Nicotine counseling 1 (or more ) delusions Duration: 1 month or longer Criterion A for Schizophrenia has never been met. Functioning is not markedly impaired Behavior is not obviously odd or bizarre Features: Differential Diagnosis Prevalence: Obsessive-compulsive and ◦ lifetime 0.2 % related disorders ◦ Most frequent is persecutory Delirium • Males > females for Jealous major neurocognitive d/o type psychotic disorder due to • Function is generally better another medical condition than in schizophrenia substance-medication- • Familiar relationship with induced psychotic disorder schizophrenia and Schizophrenia & schizotypal Schizophreniform Depressive and bipolar d/o Schizoaffective Disorder Delusion types Erotomanic Grandiose Jealous Persecutory Somatic Mixed Unspecified • Substance Abuse • Dependence • Withdrawal ◦ Alcohol Divided into 2 ◦ Caffeine groups: ◦ Cannabis ◦ Hallucinogens (with separate ◦ Substance use categories for phencyclidine and other disorders hallucinogens) ◦ Substance-induced ◦ Inhalants disorders ◦ Opioids ◦ Sedatives, hypnotics, and anxiolytics ◦ Stimulants (amphetamine-type