North Central London JHOSC
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mill Hill and Burnt Oak Annunciation Church, 4 Thirleby Road, Burnt Oak HA8 0HQ Contact: 020 8906 3340 Or Email [email protected]
What’s On near you for over 55s Age UK Barnet and 12 other voluntary sector organisations provide activities and services for older people across the borough. Whether you are looking for an exercise class, information, support with IT or opportunities to make new friends, there’s something happening near to you. Find out about it here. Page Exercise 1—9 Computers and Technology 10—11 Social groups and lunch clubs 12—19 Interest groups 20—25 Dementia activities 26—28 Day services 28—29 Handyperson Service 29 Later Life Planning Service 29 Befriending 30 Practical help 31—33 Events 34—35 www.ageukbarnet.org.uk EXERCISE Barnet The Bull Theatre 68 High Street, Barnet EN5 5SJ Contact: Jane on 020 8441 5010 Cost: £3.00 Thursdays 4.30pm—5.3pm Movement/creative dance Ewen Hall Wood Street, Barnet EN5 4BW Contact: Richard on 020 8455 5463 Cost: £6.00 for each class Mondays 2pm—3.30pm Tai Chi—Advanced Wednesdays 1.30pm—3pm Tai Chi—Intermediate Fridays 12pm—1.30pm Tai Chi—Beginners 2pm—3.30pm Tai Chi—Intermediate Church House 2 Wood Street, High Barnet EN5 4BW Contact: Dee Cummins on 020 8445 6715 or 07882 281 670 Email: [email protected] Cost: £6.00 per class Tuesdays 2pm—3pm Tai Chi Underhill Baptist Church Elton Avenue, Barnet EN5 2EA Contact: 020 3675 7246 or email [email protected] Cost: £4.50 Tuesdays 10am—12pm Love to Dance* *Class incorporates various dance styles – Salsa, Line, Cha Cha Cha, Bollywood, Rock ‘n’ Roll and many more. Burnt Oak Annunciation Church Parish Centre 4 Thirleby Road, Burnt Oak HA8 0HQ Contact: Deborah on 020 8432 -

Hendon Campus
Middlesex University teaches 40,000 students Hendon Campus and surrounding buildings on Middlesex courses at our campuses in London, Dubai, Malta and Mauritius, as well as with prestigious partners across Welcome to the world. We have invested £200 million M1 MILE Hendon Campus developing one of London’s biggest and most LK / 1 Allianz Park N WA 0 MI 2016-17 Campus Map impressive campuses here at Hendon. 2 G R G E R E A Copthall N H L A Getting to Hendon Campus A M Playing Fields N D E S P L A A1 A Middlesex University is well R N E K Rail Copthall W G served by public transport. RE A AT N Sports Ground Fast and frequent rail Y ORTH There are a number of ways W AY to travel to Hendon Campus. services run via Hendon rail station to central London Accessibility and destinations such Sunny Hill Hendon Central Underground as Luton and Gatwick A41 station and Middlesex airports and Bedford. Park S U University Hendon campus ILE N 0.5 M Catch the 183 bus from ALK / N W MIN Y are both fully accessible. 0 Station Road directly to 1 G Colindale A the main entrance. Platt Beaufort Park R We advise that you arrive via Halls D VE E A N the main entrance. LE A S E DA RO L Bus N DR A Steps, pathways and building I O N OL M C E R E entrances are displayed on Buses 143, 183 and 326 OA D the campus map. -

Hendon Campus Map
Welcome to 2 Beaufort Park Contains Ordnance Survey Sunny Hill Vector Map OpenData © Crown copyright and Colindale Platt Park database rights 2010. Middlesex Northern line Halls Cartography by Steer Getting to Welcome to ve A le Ae Davies Gleave 2011 a rod University d r 1 lin om Hendon Campus Hendon Campus Co e Rd M 2013-14 Campus Map By Underground Middlesex University Silk Stream Middlesex University is well teaches 40,000 students Park served by public transport. Hendon Central station Gr There are a number of ways (Northern Line, Edgware on Middlesex courses at 1 Hendoneyh Campus oun Colin d Hill branch) is only 30 minutes our campuses in London, deep Lane to travel to Hendon Campus. Dubai, and Mauritius, as away from Central London. Colindeep Church Road s WATFORD WAY A41 h well as with prestigious g Accessibility u The walk from the station o r partners across the world. r u Hendon Central to Hendon Campus takes L B a n We have invested £200 e e Rushgrove h Underground station and approximately 10 minutes. W T million developing one Park A T Middlesex University FO of London’s biggest and RD Turn right out of the station, A5 W Hendon campus are AY most impressive campuses E walk up the road to the main d both fully accessible. g 3 Colinhurst w junction and then turn right here at Hendon. a re We advise that you arrive via into The Burroughs. As Road W Our expertise is wide A T the main entrance. you approach the campus, Map Campus 2013-14 FO R ranging, from art and D Steps, pathways and the Hendon Town Hall and Rd W design, business, health ury 1 A sb Y Campus Hendon ing building entrances are Library are located on the K M E Road Buses to and education; to law, d g displayed on the campus left. -
Barnet Report
Alexandra Bulat Jose Javier Olivas Osuna Josh De Lyon Kuba Jablonowski Max Kiefel Diane Bolet Kira Gartzou-Katsouyanni Mary Kaldor UNDERSTANDING BREXIT IMPACTS AT A LOCAL LEVEL The London Borough of Barnet case study CONFLICT AND CIVIL SOCIETY RESEARCH UNIT Supported by the LSE Knowledge Exchange and Impact fund SEPTEMBER 2018 Summary of the project and its objectives The UK is in a critical juncture with regard to the process of negotiations to leave the European Union. Important discussions are taking place which will shape the future relation between Britain and the EU. The economic analyses published on the issue have, so far, largely failed to grasp the attention of the general public. Most of the discussions about Brexit have focused at a national level and there has been very little evidence-based discussion at a local level. This project aims at stimulating a reflexive participatory research process involving citizens, policy-makers, business people and civil-society representatives. It introduces an innovative methodology that contextualises quantitative data through expert interviews and the analysis of local sources. The reports and discussion panels organised within the framework of the project seek to increase our understanding about the impact of Brexit at a local level. Barnet Hospital main entrance Front cover: Hendon Town Hall 1 Understanding Brexit impacts at a local level London Borough of Barnet case study This report contributes to the broader research project co-ordinated by the Conflict and Civil Society Research Unit at the London School of Economics and Political Science (LSE). This study focuses on the perceived impact of Brexit on British local authorities. -

Download the Summer BACE Booklet Here. Full of Fun
Barnet Active Creative Engaging holidays - HOLIDAYS www.barnetyouth.uk Summer 2021 What’s on – Timetable Find out what’s on. PAGE 3 Healthy Eating Eating the rainbow and staying hydrated PAGE 4 Welcome to Summer Healthy Eating HOLIDAYS Choosing the right foods – food swaps PAGE 5 The school holidays are a time for children and young people to relax and have fun. Healthy Eating We believe that every family across Barnet Positive feedback from Easter Love food, hate waste PAGE 6 deserves a healthy and fulfilling holiday. Barnet Active, Creative and Engaging holidays Healthy Eating (BACE) was recently named by Barnet’s young Picnic time recipe ideas PAGE 7 people and highlights exactly what our holiday programme is all about! Healthy Eating Summer BBQ recipes PAGE 8 In our summer edition of the BACE Holidays booklet, you’ll find facts and useful tips for maintaining a healthy diet, information to support your mental wellbeing, fun activities Activity to do at home and links to online resources to learn about Colouring in and share your photos PAGE 9 healthy living. Get Active Get involved! After attending our Easter BACE Holiday Camps programme, Time to get moving PAGE 10 Sign up to one of our BACE Holiday Camps or one of parents have shared their feedback and thoughts: our enriching activity such as dance, circus skills, art, “All sessions were done very professionally so we really haven’t Get Active baking and much more by registering on our website got a favourite one. Face-to-face sessions were excellent” Time for green fingers PAGE 11 www.barnetyouth.uk/BACEHolidays. -

HENDON RESIDENTS FORUM VENUE: Hendon Town Hall
HENDON RESIDENTS FORUM VENUE: Hendon Town Hall Thursday 6th June 2019 Chairman: Anthony Finn BSc (Econ) FCA Vice-Chairman: Councillor Nizza Fluss ISSUES TO BE CONSIDERED AT THE FORUM MEETING Items must be submitted to Governance Service ([email protected]) by 10am on the fifth working day before the meeting Issue Raised Response Resident: Mr Dnkov Kiril Issue: North Circle metal bridge I wanted to inform you about the dangers around the metal bridges up the north circle, both of these are without CCTV and without enough light. My friend was a victim of an attack and we have reported this to 1. the police. The bridges are very dangerous and scary places by night. Please ensure there are lights on both of the bridges over the north circle to Brent Cross station and please install cctv. Issue Raised Response Issue Raised Response Resident: Mrs Patel P Issue: Fly tipping on corners of Bertram Road, Audley Road, Graham Road and Sevington Road. Fly tipping increased especially on corners of Bertram Road, Audley Road, Graham Road and Sevington Road. It seems as a result of 2. increase in rentals. Campaign for residents not to fly tip look after local area, in which we live, should be carried. Its easy to fly tip as councils can't do much about it. Increase in labourers and flytipping behind best way and flip out. Notices campaigns flyers to look after local area for the benefit of all Resident: Mr Pau Chul Petition: Parking around Colindale Parking outside the existing single yellow line operating hours is getting worse with vehicles parked on both sides of Colindale Avenue between the Colindale Tube Station and Public Health England causing traffic joining Colindale Avenue from the minor roads extremely difficult, increased danger to all road users and unnecessary delays to the emergency services and buses. -

Hendon Resident Forum
HENDON RESIDENTS FORUM VENUE: Hendon Town Hall Thursday 5th September Chairman: Anthony Finn BSc (Econ) FCA Vice-Chairman: Councillor Nizza Fluss ISSUES TO BE CONSIDERED AT THE FORUM MEETING Items must be submitted to Governance Service ([email protected]) by 10am on the fifth working day before the Meeting The council is consulting on its draft Growth Strategy. The strategy sets out the council's role and priorities for regeneration, development and business, employment and skills activity across the borough from 2019 to 2030. For further information on the consultation and to provide your views, please visit https://engage.barnet.gov.uk/growth-strategy This page is intentionally left blank HENDON RESIDENTS FORUM VENUE: Hendon Town Hall Thursday 5th September Chairman: Anthony Finn BSc (Econ) FCA Vice-Chairman: Councillor Nizza Fluss ISSUES TO BE CONSIDERED AT THE FORUM MEETING Items must be submitted to Governance Service ([email protected]) by 10am on the fifth working day before the meeting The council is consulting on its draft Growth Strategy. The strategy sets out the council's role and priorities for regeneration, development and business, employment and skills activity across the borough from 2019 to 2030. For further information on the consultation and to provide your views, please visit https://engage.barnet.gov.uk/growth-strategy Issue Raised Response Resident: Charlotte Daus Petition: New Colindale Residents' Association seeking traffic The Lead Petitioner will be given three minutes to present the calming measures on Heybourne Crescent and Clayton Field/ petition to the Field Mead, NW9 Forum. Following the presentation, the Residents Forum Chairman Number of signatures: 120 will decide to: If the below measures are not implemented, we fear it will not be long - Take no action; before a fatality occurs, a scenario that must be avoided at all costs. -
FINAL DOCUMENT.Indd
London Councils' Directory 2007 A GUIDE TO LOCAL GOVERNMENT IN LONDON London Councils (formerly the Association of London Government) 591/2 Southwark Street, London SE1 0AL Tel: 020 7934 9999 Fax: 020 7934 9991 ISBN: 1 85494 121 6 Price £35.00* September 2006 *£17.50 to London boroughs & voluntary organisations 1 2 CONTENTS About us 7 Greater London Employment Forum 11 Grants Committee 12 Leaders’ Committee 10 Staff 14 Transport and Environment Committee 13 London Government A brief history 17 Recent changes to London’s government 17 The London boroughs 19 Borough election results 2006 21 Town Hall addresses 24 About the data 27 The London boroughs Barking and Dagenham 28 Barnet 33 Bexley 40 Brent 46 Bromley 52 Camden 58 Croydon 63 Ealing 69 Enfield 76 Greenwich 82 Hackney 89 Hammersmith and Fulham 95 Haringey 100 Harrow 107 Havering 113 Hillingdon 119 Hounslow 125 Islington 132 Kensington and Chelsea 137 Kingston upon Thames 143 Lambeth 150 Lewisham 156 Merton 161 Newham 166 3 CONTENTS The London boroughs (continued) Redbridge 173 Richmond upon Thames 181 Southwark 188 Sutton 195 Tower Hamlets 201 Waltham Forest 208 Wandsworth 214 Westminster 222 City of London 228 Greater London Authority 236 London Development Agency 239 London Fire and Emergency Planning Authority 241 Metropolitan Police Authority 244 Transport for London 246 London MPs 247 London MEPs 249 Government departments 250 London local government professional associations 253 Health care in London 256 London Learning and Skills Councils 262 Other useful addresses 265 Media -
London Government Directory Greater London Enterprise
London government directory Greater London Enterprise Property investment and development Programme management and consulting Commercial finance Enterprise development London’s economic development company bringing commercial know-how to public policy, and delivering economic regeneration .gle.co.uk For more information, please contact: Greater London Enterprise www 28 Park Street London SE1 9EQ Tel: 020 7403 0300 [email protected] www.gle.co.uk The London Government Directory 2006 A GUIDE TO LOCAL GOVERNMENT IN A A GUIDE TO LOCAL GOVERNMENT IN LONDON ©Association of London Government 591/2 Southwark Street, London SE1 0AL Tel: 020 7934 9999 Fax: 020 7934 9991 ISBN: 1 85494 165 8 Price £35.00* September 2005 *£17.50 to London boroughs & voluntary organisations 1 Minimum Environmental Impact for Maximum Printed Impact! Photograph by Jeff [email protected] Every year Sprinters looks at the way we affect our environment and how we can reduce waste when printing the literature our capital city needs. This year we have introduced a new press which operates on a waterless litho system with fully recyclable plates. The result is less chemistry and a more energy efficient output while still offering a full range of recycled papers and boards. For more information about Sprinters please call or visit our website. Sprinters (London) Limited Churchill House, 114 Windmill Road, Brentford, Middlesex TW8 9NB Tel: 020 8847 2128 Fax: 020 8569 8681 ISDN: 020 8560 9547 [email protected] www.sprinters.co.uk CONTENTS London Government A brief history -

1St Saturday of Each Month at New Barnet Community Centre, 48-50 Victoria Road, New Barnet EN4 9PF
How to contact your councillors for Brunswick Park Ward Lisa Rutter Andreas Tambourides Andreas Ioannidis Surgery Times 2nd Saturday every month, 10.30am-12noon. Osidge Library, Brunswick Park Road, N11 1EU. NO APPOINTMENT NECESSARY Write to your local councillor. You can write to your local councillor at this address: c/o Conservative Group (L Rutter & A Tambourides) Labour Group (A Ioannidis) Members Room Hendon Town Hall, The Burroughs, Hendon, NW4 4BG Email your councillor Email: [email protected] Email: [email protected] Email: [email protected] 1 How to contact your councillors for Burnt Oak Alex Brodkin Claire Farrier Charlie O’Macauley Surgery times Every Saturday at 10.30am to 11.30am at Burnt Oak Library & Customer Service Centre, 99 Watling Avenue, Burnt Oak HA8 OUB. NO APPOINTMENT NECESSARY Write to your local councillor. You can write to your local councillor at this address: c/o Labour Group Members Room Hendon Town Hall, The Burroughs, Hendon, NW4 4BG Email your councillor Email: [email protected] Email: [email protected] Email: [email protected] 2 How to contact your councillors for Childs Hill Jack Cohen Lord Palmer Sussette Palmer Surgery Times 1st Thursday of each month 7pm-8pm. Childs Hill Library, Cricklewood Lane, London NW2. NO APPOINTMENT NECESSARY Write to your local councillor. You can write to your local councillor at this address: c/o Lib Dem Group Members Room Hendon Town Hall, The Burroughs, Hendon, NW4 4BG Email your councillor Email: [email protected] Email: [email protected] Email: [email protected] 3 How to contact your councillors for Colindale Geoffery Johnson Gill Sargeant Zakia Zubairi Surgery times Every Saturday at Grahame Park Library, The Concourse, Colindale, NW9 5XL. -
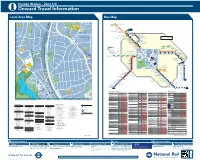
Local Area Map Bus Map
Hendon Station – Zone 3/4 i Onward Travel Information Local Area Map Bus Map 2 WROUGHTON TERRACE 32 A MMiddlesex L Playground W S H MDX 142 Y E 25 S N T Universitynniversiversityrsity H B N O A 1 Allotments B I N G 1 G T Rushgrove Park E O N N MDX G R O A D A D E Middlesex University R G 10 R Watford Junction U 56 D A Grove A 35 M S BONVILLE BABINGTON ROAD Colindale GARDENS (Hatchcroft) 33 R WATFORD U W E G MDX N D O S Y Park E Primary School N E S N F Hendon Fire N N N MDX R E O R R S D Watford High Street D Station O E 24 R R H B G A A C L A MDX G U V O R N E 107 L C 23 D S D N I E MDX N B I N O A O MDX Bushey L 58 C S W Middlesex O R 1 E L E C S University I Hendon E C C L S E E N O (Grove) N Library Bushey Heath V T D 1 ST . EGERTON GARDENS J O S E E W E N L O C K G D P H S E O Three Crowns 32 G R O 3 63 E V E H E R U P NS T N Stanmore Broadway N5 N16 E G L Hendon S V Our Lady of A E N 102 E A COLIN DEEP S D H S N O Town Hall E G E R T R L O N G A Dolours RC Church N 79 N BRIDGE E C 64 E O E D U S Edgware R N T D Subway Stanmore A E K V N R 2 U C Our Lady of A Y A I 51 L R STANMORE D G Hendon L Dolours E R I N Canons Corner F I Methodist D G Social Centre O L O Silk Stream R O W O Church C EDGWARE V E 41 7 G W S 34 N A 44 E R H W D A Chapel E W N T (Private) G 43 Watling Avenue Gunter Grove A S BRAMPTON GROVE Y Tennis Courts M 1 THHHE 18 F Burnt Oak R E U O N O 65 58 D E D E Edgware Community Hospital Burnt Oak Leisure Centre A E I G H G A R N S 1 R S R St. -

Inter Faith Week 2014 Event List
List of events ‐ Inter Faith Week 2014 ID: 1 Date of event: 16 November 2014 End date: 16 November 2014 Name of Event: Inter Faith Mitzvah Day ‐ Food Collection Organisation(s) holding the event: Edgware and District Reform Synagogue Husaini Islamic Centre Short description of event: Collecting food for Sufra NW London Foodbank outside Stanmore Sainsbury's Location: 1 The Broadway STANMORE HA7 4DA Local authority: London Borough of Harrow Nation/ region: LONDON Town: Stanmore ID: 13 Date of event: 16 November 2014 End date: 16 November 2014 Name of Event: Inter Faith Mitzvah Day ‐ Food Collection Organisation(s) holding the event: Sha'arei Tsedek Palmer's Green Mosque All Saints Friern Barnet Short description of event: Collecting food outside Waitrose Whetstone for Homeless Action Location: 1305 High Rd, Whetstone, London N20 9HX Local authority: Whetstone Parish Council Nation/ region: LONDON Town: Whetstone ID: 16 Date of event: 16 November 2014 End date: 16 November 2014 Name of Event: Interfaith Mitzvah Day ‐ Food and Toiletries Collection Organisation(s) holding the event: New London Synagogue, Abbey Road Ladbroke Grove Mosque Short description of event: Collecting food and toiletries outside Sainsbury's Ladbroke Grove for Dashwood House women's refuge Location: Ladbroke Grove London W10 5AA Local authority: Royal Borough of Kensington and Chelsea Council Nation/ region: LONDON Town: Ladbroke Grove 26 June 2015 Page 1 of 146 ID: 17 Date of event: 16 November 2014 End date: 16 November 2014 Name of Event: Inter Faith Mitzvah Day ‐ Give away your lunch Organisation(s) holding the event: Ernst & Young Ernst & Young Muslim Network Short description of event: Give away your Lunch to a local homeless shelter.