Management of Cough
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
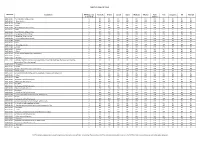
TARIFF SCHEDULE of CHILE Description MFN Base Rate
TARIFF SCHEDULE OF CHILE Tariff Line Description MFN Base rate Australia Brunei Canada Japan Malaysia Mexico New Peru Singapore US Vietnam (1 Jan 2010) Zealand 0101.10.00 -Pure-bred breeding animals 6 EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF 0101.90.11 ---Race horses 6 EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF 0101.90.19 ---Other 6 EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF 0101.90.90 --Other 6 EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF 0102.10.00 -Pure-bred breeding animals 6 EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF 0102.90.00 -Other 6 EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF 0103.10.00 -Pure-bred breeding animals 6 EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF 0103.91.00 --Weighing less than 50 kg 6 EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF 0103.92.00 --Weighing 50 kg or more 6 EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF 0104.10.10 --Pure-bred breeding animals 6 EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF 0104.10.90 --Other 6 EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF 0104.20.00 -Goats 6 EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF 0105.11.10 ---Breeding animals 6 EIF EIF B8 EIF EIF EIF EIF EIF EIF EIF EIF 0105.11.90 ---Other 6 EIF EIF B8 EIF EIF EIF EIF EIF EIF EIF EIF 0105.12.00 --Turkeys 6 EIF EIF B8 EIF EIF EIF EIF EIF EIF EIF EIF 0105.19.00 --Other 6 EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF 0105.94.00 --Fowls of the species Gallus domesticus 6 EIF EIF B8 EIF EIF EIF EIF EIF EIF EIF EIF 0105.99.00 --Other 6 EIF EIF B8 EIF EIF EIF EIF EIF EIF EIF EIF 0106.11.00 --Primates 6 EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF -

(12) Patent Application Publication (10) Pub. No.: US 2004/0224012 A1 Suvanprakorn Et Al
US 2004O224012A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2004/0224012 A1 Suvanprakorn et al. (43) Pub. Date: Nov. 11, 2004 (54) TOPICAL APPLICATION AND METHODS Related U.S. Application Data FOR ADMINISTRATION OF ACTIVE AGENTS USING LIPOSOME MACRO-BEADS (63) Continuation-in-part of application No. 10/264,205, filed on Oct. 3, 2002. (76) Inventors: Pichit Suvanprakorn, Bangkok (TH); (60) Provisional application No. 60/327,643, filed on Oct. Tanusin Ploysangam, Bangkok (TH); 5, 2001. Lerson Tanasugarn, Bangkok (TH); Suwalee Chandrkrachang, Bangkok Publication Classification (TH); Nardo Zaias, Miami Beach, FL (US) (51) Int. CI.7. A61K 9/127; A61K 9/14 (52) U.S. Cl. ............................................ 424/450; 424/489 Correspondence Address: (57) ABSTRACT Eric G. Masamori 6520 Ridgewood Drive A topical application and methods for administration of Castro Valley, CA 94.552 (US) active agents encapsulated within non-permeable macro beads to enable a wider range of delivery vehicles, to provide longer product shelf-life, to allow multiple active (21) Appl. No.: 10/864,149 agents within the composition, to allow the controlled use of the active agents, to provide protected and designable release features and to provide visual inspection for damage (22) Filed: Jun. 9, 2004 and inconsistency. US 2004/0224012 A1 Nov. 11, 2004 TOPCAL APPLICATION AND METHODS FOR 0006 Various limitations on the shelf-life and use of ADMINISTRATION OF ACTIVE AGENTS USING liposome compounds exist due to the relatively fragile LPOSOME MACRO-BEADS nature of liposomes. Major problems encountered during liposome drug Storage in vesicular Suspension are the chemi CROSS REFERENCE TO OTHER cal alterations of the lipoSome compounds, Such as phos APPLICATIONS pholipids, cholesterols, ceramides, leading to potentially toxic degradation of the products, leakage of the drug from 0001) This application claims the benefit of U.S. -

Pharmaceutical Manufacturing Formulations Liquid Products V () L UME Sarfaraz K
HANDBOOK OF Pharmaceutical Manufacturing Formulations Liquid Products V () L UME Sarfaraz K. Niazi CRC PRESS Boca Raton London New York Washington, D.C. Table of Contents PART I Regulatory and Manufacturing Guidance 1 Chapter 1 Current Good Manufacturing Practice Considerations in Liquid Manufacturing 3 I. Introduction 3 II. Facilities 3 III. Equipment 3 IV. Raw Materials 4 V. Compounding 4 VI. Microbiological Quality 4 VII. Oral Suspensions 5 VIII. Product Specifications 5 IX. Process Validation 5 X. Stability 5 XI. Packaging 6 Chapter 2 Stability Testing of New Drug Substances and Products 7 I. Introduction 7 II. Drug Substance 7 A. General Case 8 B. Drug Substances Intended for Storage in a Refrigerator 8 C. Drag Substances Intended for Storage in a Freezer 8 D. Drug Substances Intended for Storage below -20°C 9 HI. Drag Product 10 A. General Case •' B. Drag Products Packaged in Impermeable Containers 11 C. Drag Products Packaged in Semipermeable Containers 11 D. Drag Products Intended for Storage in a Refrigerator 12 E. Drag Products Intended for Storage in a Freezer 13 F. Drag Products Intended for Storage below -20"C 13 IV Glossary 14 References 1() Chapter 3 Container Closure Systems '7 I. Introduction '7 A. Definitions '7 B. Current Good Manufacturing Practice, the Consumer Product Safety Commission, and Requirements on Containers and Closures 17 C. Additional Considerations 17 II. Qualification and Quality Control of Packaging Components 18 A. Description 21 B. Information about Suitability 21 C. Stability Data (Packaging Concerns) 22 D. Inhalation Drag Products 23 E. Injection and Ophthalmic Drag Products 23 F. -

CONTROLLED SUBSTANCE, DRUG, DEVICE and COSMETIC ACT - SCHEDULE I CONTROLLED SUBSTANCES Act of Jun
CONTROLLED SUBSTANCE, DRUG, DEVICE AND COSMETIC ACT - SCHEDULE I CONTROLLED SUBSTANCES Act of Jun. 23, 2011, P.L. 36, No. 7 Cl. 35 Session of 2011 No. 2011-7 SB 1006 AN ACT Amending the act of April 14, 1972 (P.L.233, No.64), entitled "An act relating to the manufacture, sale and possession of controlled substances, other drugs, devices and cosmetics; conferring powers on the courts and the secretary and Department of Health, and a newly created Pennsylvania Drug, Device and Cosmetic Board; establishing schedules of controlled substances; providing penalties; requiring registration of persons engaged in the drug trade and for the revocation or suspension of certain licenses and registrations; and repealing an act," further providing for Schedule I controlled substances. The General Assembly of the Commonwealth of Pennsylvania hereby enacts as follows: Section 1. Section 4(1) of the act of April 14, 1972 (P.L.233, No.64), known as The Controlled Substance, Drug, Device and Cosmetic Act, amended November 24, 1999 (P.L.894, No.55), is amended to read: Section 4. Schedules of Controlled Substances.--The following schedules include the controlled substances listed or to be listed by whatever official name, common or usual name, chemical name, or trade name designated. (1) Schedule I--In determining that a substance comes within this schedule, the secretary shall find: a high potential for abuse, no currently accepted medical use in the United States, and a lack of accepted safety for use under medical supervision. The following controlled substances are included in this schedule: (i) Any of the following opiates, including their isomers, esters, ethers, salts, and salts of isomers, esters, and ethers, unless specifically excepted, whenever the existence of such isomers, esters, ethers and salts is possible within the specific chemical designation: 1. -

2. Study Report Synopsis of Protocol 7164-L-01
Clinical Trial Report - Study 7164L01 Pholcodine 2. STUDY REPORT SYNOPSIS OF PROTOCOL 7164-L-01 Name of Sponsor Company Individual Study Table referring to the dossier (for National Authority use only) Zambon Group S.p.A. PART: [……] Name of finished product VOLUME: [……] Name of active ingredient Pholcodine PAGE: [……] Title of the study A MULTICENTER, RANDOMIZED, PARALLEL GROUP, CONTROLLED, DOUBLE-BLIND STUDY TO EVALUATE EFFICACY AND SAFETY OF PHOLCODINE AS ANTITUSSIVE AGENT VS DEXTROMETORPHAN IN NON-PRODUCTIVE COUGH Principal Investigators and study sites The study took place in Italy and involved 20 recruiters General Practitioners. 101: M. Acciarresi (v. Ponti, Foligno, PG); 102: P. Bonifazi (v. Ponti, Foligno, PG); 103: R. Equinozzi (v. Roma 84/, Foligno, PG); 104: R. Falcinelli (v. Carducci 3, Montefalco, PG); 105: M. Montironi (v. Flaminia Km 182, Gualdo Tadino, PG), 106 L. Pisell (v. Arco di Druso 5, Spoleto, PG); 201 G. Amoretti (v. Repubblica 9, Imperia, IM); 202: A. Astorino, v. Cipressa 32, San Lorenzo al Mare, IM); 203: R. Buccelli (v. S. Antonio 11, Imperia, IM); 204: F. Dolmetta (v. Vignasse 68, San Lorenzo al Mare , IM); 205; G. Lanteri( v. Carducci 1, Imperia, IM); 206: A. Novaro (v. Nazionale 29, Imperia, IM); 207: M. Pinelli (v. Parini 34, Imperia, IM); 301 GL Balderi (v. Carducci 33, Marina di Pietrasanta, LU); 302: F. Bertuccelli (v. Leopardi 35, Viareggio, LU); 303: C. Bonin (v. Montemagno,2, Montemagno, LU); 304: PL Franceschi (v. Misericordia 89, Stiava, LU); 305: M. Pardini (v. Garibaldi 29, Viareggio, LU); 306: M. Pardini (v. Italica 70, Lido di Camaiore, LU); 307: A. -

(12) United States Patent (10) Patent No.: US 9,314.465 B2 Brew Et Al
US009314465B2 (12) United States Patent (10) Patent No.: US 9,314.465 B2 Brew et al. (45) Date of Patent: *Apr. 19, 2016 (54) DRUG COMBINATIONS AND USES IN 2008.0003280 A1 1/2008 Levine et al. ................. 424/456 TREATING A COUGHING CONDITION 2008/O176955 A1 7/2008 Hecket al. 2008, 0220078 A1 9, 2008 Morton et al. (71) Applicant: Infirst Healthcare Limited 2009, O136427 A1 5/2009 Croft et al. 2009, O220594 A1 9, 2009 Field (72) Inventors: John Brew, London (GB); Robin Mark 2012/O128738 A1 5, 2012 Brew et al. Bannister, London (GB) 2012fO252824 A1 10/2012 Brew et al. (73) Assignee: Infirst Healthcare Limited, London FOREIGN PATENT DOCUMENTS (GB) CN 1593451 3, 2005 CN 101024.014 A 8, 2007 (*) Notice: Subject to any disclaimer, the term of this CN 101112383 B 5, 2010 patent is extended or adjusted under 35 DE 4420708 A1 12, 1995 U.S.C. 154(b) by 0 days. EP 2050435 B1 4/2009 GB 2114001 A 8, 1983 This patent is Subject to a terminal dis GB 2284761 A 6, 1995 claimer. GB 2424.185 B 9, 2006 GB 2442828 A 4/2008 JP 62-249924 A 10, 1987 (21) Appl. No.: 14/287,014 JP H1O-316568 A 12/1998 JP 2001-518928 A 10, 2001 (22) Filed: May 24, 2014 JP 200219.3839. A T 2002 JP 2003-012514 A 1, 2003 (65) Prior Publication Data JP 20030552.58 A 2, 2003 JP 2003128549 A 5, 2003 US 2014/O256750 A1 Sep. 11, 2014 JP 2003-321357 A 11, 2003 JP 2005-516917 A 6, 2005 JP 2008O31146 A 2, 2008 Related U.S. -

Pharmacology on Your Palms CLASSIFICATION of the DRUGS
Pharmacology on your palms CLASSIFICATION OF THE DRUGS DRUGS FROM DRUGS AFFECTING THE ORGANS CHEMOTHERAPEUTIC DIFFERENT DRUGS AFFECTING THE NERVOUS SYSTEM AND TISSUES DRUGS PHARMACOLOGICAL GROUPS Drugs affecting peripheral Antitumor drugs Drugs affecting the cardiovascular Antimicrobial, antiviral, Drugs affecting the nervous system Antiallergic drugs system antiparasitic drugs central nervous system Drugs affecting the sensory Antidotes nerve endings Cardiac glycosides Antibiotics CNS DEPRESSANTS (AFFECTING THE Antihypertensive drugs Sulfonamides Analgesics (opioid, AFFERENT INNERVATION) Antianginal drugs Antituberculous drugs analgesics-antipyretics, Antiarrhythmic drugs Antihelminthic drugs NSAIDs) Local anaesthetics Antihyperlipidemic drugs Antifungal drugs Sedative and hypnotic Coating drugs Spasmolytics Antiviral drugs drugs Adsorbents Drugs affecting the excretory system Antimalarial drugs Tranquilizers Astringents Diuretics Antisyphilitic drugs Neuroleptics Expectorants Drugs affecting the hemopoietic system Antiseptics Anticonvulsants Irritant drugs Drugs affecting blood coagulation Disinfectants Antiparkinsonian drugs Drugs affecting peripheral Drugs affecting erythro- and leukopoiesis General anaesthetics neurotransmitter processes Drugs affecting the digestive system CNS STIMULANTS (AFFECTING THE Anorectic drugs Psychomotor stimulants EFFERENT PART OF THE Bitter stuffs. Drugs for replacement therapy Analeptics NERVOUS SYSTEM) Antiacid drugs Antidepressants Direct-acting-cholinomimetics Antiulcer drugs Nootropics (Cognitive -

UNIVERSITE DE NANTES Thomas Gelineau
UNIVERSITE DE NANTES __________ FACULTE DE MEDECINE __________ Année 2011 N° 139 THESE pour le DIPLÔME D’ÉTAT DE DOCTEUR EN MÉDECINE DES de médecine générale par Thomas Gelineau né le 29 janvier 1983 à Cholet __________ Présentée et soutenue publiquement le 06/12/2011 __________ LE RHUME DE L'ENFANT ET SON TRAITEMENT: DECISION PARTAGEE AVEC LES PARENTS D'APRES UN QUESTIONNAIRE __________ Président : Monsieur le Professeur Olivier MALARD Directeur de thèse : Madame le Professeur Jacqueline LACAILLE 1 Table des matières IIntroduction................................................................................................................ 7 IIDéfinition, état des connaissances...........................................................................8 1Le rhume.......................................................................................................................................8 APhysiopathologie............................................................................................................................. 8 aL'origine virale.................................................................................................................................... 8 bLa saisonnalité................................................................................................................................... 8 cL'âge de survenue.............................................................................................................................. 9 dLe sexe.................................................................................................................................................. -
Department of Health
DEPARTMENT OF HEALTH National Drug Policy - Pharmaceutical Management Unit 50 National Formulary Committee Philippine National Drug Formulary EssentialEssential MedicinesMedicines ListList Volume I, 7th Edition ( 2008 ) Published by: The National Formulary Committee National Drug Policy ‐ Pharmaceutical Management Unit 50 DEPARTMENT OF HEALTH Manila, Philippines All rights reserved 2008 The National Formulary Committee National Drug Policy‐Pharmaceutical Management Unit 50 (NDP‐PMU 50) Department of Health San Lazaro Cmpd., Rizal Ave., Sta. Cruz, Manila, Philippines 1003 ISBN 978‐971‐91620‐7‐0 Any part or the whole book may be reproduced or transmitted without any alteration, in any form or by any means, with permission from DOH provided it is not sold commercially. ii PHILIPPINE NATIONAL DRUG FORMULARY Volume I, 7th Edition 2 0 0 8 Francisco T. Duque III, MD, MSc Secretary of Health Alexander A. Padilla Undersecretary of Health, Office for External Affairs Robert Louie P. So, MD Program Manager, NDP-PMU 50 Dennis S. Quiambao, MD Proj. Mgmt. Operating Officer & Coordinator (PMOOC) NDP-PMU 50 NATIONAL FORMULARY COMMITTEE Estrella B. Paje-Villar, MD, DTM & H Chairperson Jose M. Acuin, MD, MSc Alma L. Jimenez, MD Alejandro C. Baroque II, MD Marieta B. de Luna, MD Bu C. Castro, MD Nelia P. Cortes-Maramba, MD Dina V. Diaz, MD Yolanda R. Robles, PhD Pharm Mario R. Festin, MD, MS, MHPEd Isidro C. Sia, MD BFAD Representative SECRETARIAT Luzviminda O. Marquez, RPh, RMT Mary Love C. Victoria, RPh Michael D. Junsay, RPh Ermalyn M. Magturo iii Republic of the Philippines DEPARTMENT OF HEALTH OFFICE OF THE SECRETARY 2/F Bldg. 1, San Lazaro Cmpd., Rizal Avenue, Sta. -

Malta Medicines List April 08
Defined Daily Doses Pharmacological Dispensing Active Ingredients Trade Name Dosage strength Dosage form ATC Code Comments (WHO) Classification Class Glucobay 50 50mg Alpha Glucosidase Inhibitor - Blood Acarbose Tablet 300mg A10BF01 PoM Glucose Lowering Glucobay 100 100mg Medicine Rantudil® Forte 60mg Capsule hard Anti-inflammatory and Acemetacine 0.12g anti rheumatic, non M01AB11 PoM steroidal Rantudil® Retard 90mg Slow release capsule Carbonic Anhydrase Inhibitor - Acetazolamide Diamox 250mg Tablet 750mg S01EC01 PoM Antiglaucoma Preparation Parasympatho- Powder and solvent for solution for mimetic - Acetylcholine Chloride Miovisin® 10mg/ml Refer to PIL S01EB09 PoM eye irrigation Antiglaucoma Preparation Acetylcysteine 200mg/ml Concentrate for solution for Acetylcysteine 200mg/ml Refer to PIL Antidote PoM Injection injection V03AB23 Zovirax™ Suspension 200mg/5ml Oral suspension Aciclovir Medovir 200 200mg Tablet Virucid 200 Zovirax® 200mg Dispersible film-coated tablets 4g Antiviral J05AB01 PoM Zovirax® 800mg Aciclovir Medovir 800 800mg Tablet Aciclovir Virucid 800 Virucid 400 400mg Tablet Aciclovir Merck 250mg Powder for solution for inj Immunovir® Zovirax® Cream PoM PoM Numark Cold Sore Cream 5% w/w (5g/100g)Cream Refer to PIL Antiviral D06BB03 Vitasorb Cold Sore OTC Cream Medovir PoM Neotigason® 10mg Acitretin Capsule 35mg Retinoid - Antipsoriatic D05BB02 PoM Neotigason® 25mg Acrivastine Benadryl® Allergy Relief 8mg Capsule 24mg Antihistamine R06AX18 OTC Carbomix 81.3%w/w Granules for oral suspension Antidiarrhoeal and Activated Charcoal -

Use of Antitussives After the Initiation of Angiotensin-Converting Enzyme Inhibitors
저작자표시-비영리-변경금지 2.0 대한민국 이용자는 아래의 조건을 따르는 경우에 한하여 자유롭게 l 이 저작물을 복제, 배포, 전송, 전시, 공연 및 방송할 수 있습니다. 다음과 같은 조건을 따라야 합니다: 저작자표시. 귀하는 원저작자를 표시하여야 합니다. 비영리. 귀하는 이 저작물을 영리 목적으로 이용할 수 없습니다. 변경금지. 귀하는 이 저작물을 개작, 변형 또는 가공할 수 없습니다. l 귀하는, 이 저작물의 재이용이나 배포의 경우, 이 저작물에 적용된 이용허락조건 을 명확하게 나타내어야 합니다. l 저작권자로부터 별도의 허가를 받으면 이러한 조건들은 적용되지 않습니다. 저작권법에 따른 이용자의 권리는 위의 내용에 의하여 영향을 받지 않습니다. 이것은 이용허락규약(Legal Code)을 이해하기 쉽게 요약한 것입니다. Disclaimer 약학 석사학위 논문 안지오텐신 전환 효소 억제제 개시 이후 진해제의 사용 분석 Use of Antitussives After the Initiation of Angiotensin-Converting Enzyme Inhibitors 2017년 8월 서울대학교 대학원 약학과 사회약학전공 권 익 태 안지오텐신 전환 효소 억제제 개시 이후 진해제의 사용 분석 Use of Antitussives After the Initiation of Angiotensin-Converting Enzyme Inhibitors 지도교수 홍 송 희 이 논문을 권익태 석사학위논문으로 제출함 2017년 4월 서울대학교 대학원 약학과 사회약학전공 권 익 태 권익태의 석사학위논문을 인준함 2017년 6월 위 원 장 (인) 부 위 원 장 (인) 위 원 (인) Abstract Use of Antitussives After the Initiation of Angiotensin-Converting Enzyme Inhibitors Ik Tae Kwon Department of Social Pharmacy College of Pharmacy, Seoul National University Background Angiotensin-converting enzyme inhibitors (ACEI) can induce a dry cough, more frequently among Asians. If healthcare professionals fail to detect coughs induced by an ACEI, patients are at risk of getting antitussives inappropriately instead of discontinuing ACEI. The purpose of this study was to examine how the initiation of ACEI affects the likelihood of antitussive uses compared with the initiation of Angiotensin Receptor Blocker (ARB) and to determine the effect of the antitussive use on the duration and adherence of therapy in a Korean population. -

General Pharmacology
GENERAL PHARMACOLOGY Winners of “Nobel” prize for their contribution to pharmacology Year Name Contribution 1923 Frederick Banting Discovery of insulin John McLeod 1939 Gerhard Domagk Discovery of antibacterial effects of prontosil 1945 Sir Alexander Fleming Discovery of penicillin & its purification Ernst Boris Chain Sir Howard Walter Florey 1952 Selman Abraham Waksman Discovery of streptomycin 1982 Sir John R.Vane Discovery of prostaglandins 1999 Alfred G.Gilman Discovery of G proteins & their role in signal transduction in cells Martin Rodbell 1999 Arvid Carlson Discovery that dopamine is neurotransmitter in the brain whose depletion leads to symptoms of Parkinson’s disease Drug nomenclature: i. Chemical name ii. Non-proprietary name iii. Proprietary (Brand) name Source of drugs: Natural – plant /animal derivatives Synthetic/semisynthetic Plant Part Drug obtained Pilocarpus microphyllus Leaflets Pilocarpine Atropa belladonna Atropine Datura stramonium Physostigma venenosum dried, ripe seed Physostigmine Ephedra vulgaris Ephedrine Digitalis lanata Digoxin Strychnos toxifera Curare group of drugs Chondrodendron tomentosum Cannabis indica (Marijuana) Various parts are used ∆9Tetrahydrocannabinol (THC) Bhang - the dried leaves Ganja - the dried female inflorescence Charas- is the dried resinous extract from the flowering tops & leaves Papaver somniferum, P album Poppy seed pod/ Capsule Natural opiates such as morphine, codeine, thebaine Cinchona bark Quinine Vinca rosea periwinkle plant Vinca alkaloids Podophyllum peltatum the mayapple