The Future of B-Cell Activating Factor Antagonists in the Treatment of Systemic Lupus Erythematosus
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

BAFF-Neutralizing Interaction of Belimumab Related to Its Therapeutic Efficacy for Treating Systemic Lupus Erythematosus
ARTICLE DOI: 10.1038/s41467-018-03620-2 OPEN BAFF-neutralizing interaction of belimumab related to its therapeutic efficacy for treating systemic lupus erythematosus Woori Shin1, Hyun Tae Lee1, Heejin Lim1, Sang Hyung Lee1, Ji Young Son1, Jee Un Lee1, Ki-Young Yoo1, Seong Eon Ryu2, Jaejun Rhie1, Ju Yeon Lee1 & Yong-Seok Heo1 1234567890():,; BAFF, a member of the TNF superfamily, has been recognized as a good target for auto- immune diseases. Belimumab, an anti-BAFF monoclonal antibody, was approved by the FDA for use in treating systemic lupus erythematosus. However, the molecular basis of BAFF neutralization by belimumab remains unclear. Here our crystal structure of the BAFF–belimumab Fab complex shows the precise epitope and the BAFF-neutralizing mechanism of belimumab, and demonstrates that the therapeutic activity of belimumab involves not only antagonizing the BAFF–receptor interaction, but also disrupting the for- mation of the more active BAFF 60-mer to favor the induction of the less active BAFF trimer through interaction with the flap region of BAFF. In addition, the belimumab HCDR3 loop mimics the DxL(V/L) motif of BAFF receptors, thereby binding to BAFF in a similar manner as endogenous BAFF receptors. Our data thus provides insights for the design of new drugs targeting BAFF for the treatment of autoimmune diseases. 1 Department of Chemistry, Konkuk University, 120 Neungdong-ro, Gwangjin-gu, Seoul 05029, Republic of Korea. 2 Department of Bio Engineering, Hanyang University, 222 Wangsimni-ro, Seongdong-gu, Seoul 04763, Republic of Korea. These authors contributed equally: Woori Shin, Hyun Tae Lee, Heejin Lim, Sang Hyung Lee. -

Distribution and Clinical Significance of Heparan Sulfate Proteoglycans in Ovarian Cancer
5178 Vol. 10, 5178–5186, August 1, 2004 Clinical Cancer Research Distribution and Clinical Significance of Heparan Sulfate Proteoglycans in Ovarian Cancer E. June Davies,1 Fiona H. Blackhall,1 decan-1 and glypican-1 were poor prognostic factors for Jonathan H. Shanks,2 Guido David,3 survival in univariate analysis. Alan T. McGown,4 Ric Swindell,5 Conclusion: We report for the first time distinct pat- 6 7 terns of expression of cell surface and extracellular matrix Richard J. Slade, Pierre Martin-Hirsch, heparan sulfate proteoglycans in normal ovary compared 1 1 John T. Gallagher, and Gordon C. Jayson with ovarian tumors. These data reinforce the role of the 1Cancer Research UK and University of Manchester Department of tumor stroma in ovarian adenocarcinoma and suggest that Medical Oncology, Paterson Institute for Cancer Research, stromal induction of syndecan-1 contributes to the patho- Manchester, England; 2Department of Histopathology, Christie Hospital NHS Trust, Manchester, England; 3Department of Medicine, genesis of this malignancy. University of Leuven, Leuven, Belgium.; 4Cancer Research UK Department of Experimental Pharmacology, Paterson Institute for Cancer Research, Manchester, England; 5Department of Medical INTRODUCTION Statistics, Christie Hospital NHS Trust, Manchester, England; The heparan sulfate proteoglycans (HSPGs) play diverse 6Department of Obstetrics and Gynaecology, Hope Hospital, Salford, Manchester, England; 7Department of Gynaecological Oncology, St. roles in tumor biology by mediating adhesion and migration -

Tabalumab for Systemic Lupus Erythematosus
Horizon Scanning Centre May 2014 Tabalumab for systemic lupus erythematosus SUMMARY NIHR HSC ID: 5581 Tabalumab (LY-2127399) is intended to be used as second line therapy for the treatment of systemic lupus erythematosus (SLE). If licensed, it would offer an additional treatment option for patients who have active moderate to severe SLE despite treatment with glucocorticoids, anti-malarials, and/or immunosuppressants; a group who currently have few effective therapies This briefing is available. Tabalumab is a human anti-B-cell activating factor (BAFF or B based on lymphocyte stimulator [BLyS]) monoclonal antibody. It is administered information subcutaneously, in contrast to the only existing licensed BAFF antagonist, which is administered via IV infusion. available at the time of research and a The annual incidence of SLE in the UK is between 3 and 4 cases per limited literature 100,000 population, which equates to approximately 1,600 and 2,100 new search. It is not cases in England per year. The estimated prevalence of SLE is 25-28 per intended to be a 100,000 population, commensurate with around 15,000 people in England definitive statement with the disease. SLE is associated with considerable morbidity and on the safety, mortality, with 10-year survival rates ranging from 70% to 92%. Around 40– efficacy or 70% of SLE patients develop renal involvement which confers a worse effectiveness of the prognosis for survival; and approximately 10% of patients with lupus nephritis health technology develop end-stage renal failure requiring dialysis or transplantation. covered and should Neuropsychiatric involvement occurs in 27% of people with SLE, and SLE is not be used for also characterised by haematological features and cardiovascular commercial complications. -

Study Protocol
PROTOCOL SYNOPSIS A Multicentre, Randomised, Double-blind, Placebo-controlled, Phase 3 Study Evaluating the Efficacy and Safety of Two Doses of Anifrolumab in Adult Subjects with Active Systemic Lupus Erythematosus International Coordinating Investigator Study site(s) and number of subjects planned Approximately 450 subjects are planned at approximately 173 sites. Study period Phase of development Estimated date of first subject enrolled Q2 2015 3 Estimated date of last subject completed Q2 2018 Study design This is a Phase 3, multicentre, multinational, randomised, double-blind, placebo-controlled study to evaluate the efficacy and safety of an intravenous treatment regimen of anifrolumab (150 mg or 300 mg) versus placebo in subjects with moderately to severely active, autoantibody-positive systemic lupus erythematosus (SLE) while receiving standard of care (SOC) treatment. The study will be performed in adult subjects aged 18 to 70 years of age. Approximately 450 subjects receiving SOC treatment will be randomised in a 1:2:2 ratio to receive a fixed intravenous dose of 150 mg anifrolumab, 300 mg anifrolumab, or placebo every 4 weeks (Q4W) for a total of 13 doses (Week 0 to Week 48), with the primary endpoint evaluated at the Week 52 visit. Investigational product will be administered as an intravenous (IV) infusion via an infusion pump over a minimum of 30 minutes, Q4W. Subjects must be taking either 1 or any combination of the following: oral corticosteroids (OCS), antimalarial, and/or immunosuppressants. Randomisation will be stratified using the following factors: SLE Disease Activity Index 2000 (SLEDAI-2K) score at screening (<10 points versus ≥10 points); Week 0 (Day 1) OCS dose 2(125) Revised Clinical Study Protocol Drug Substance Anifrolumab (MEDI-546) Study Code D3461C00005 Edition Number 5 Date 18 May 2016 (<10 mg/day versus ≥10 mg/day prednisone or equivalent); and results of a type 1 interferon (IFN) test (high versus low). -
BCMA-Targeted Immunotherapy for Multiple Myeloma Bo Yu1, Tianbo Jiang2 and Delong Liu2*
Yu et al. Journal of Hematology & Oncology (2020) 13:125 https://doi.org/10.1186/s13045-020-00962-7 REVIEW Open Access BCMA-targeted immunotherapy for multiple myeloma Bo Yu1, Tianbo Jiang2 and Delong Liu2* Abstract B cell maturation antigen (BCMA) is a novel treatment target for multiple myeloma (MM) due to its highly selective expression in malignant plasma cells (PCs). Multiple BCMA-targeted therapeutics, including antibody-drug conjugates (ADC), chimeric antigen receptor (CAR)-T cells, and bispecific T cell engagers (BiTE), have achieved remarkable clinical response in patients with relapsed and refractory MM. Belantamab mafodotin-blmf (GSK2857916), a BCMA-targeted ADC, has just been approved for highly refractory MM. In this article, we summarized the molecular and physiological properties of BCMA as well as BCMA-targeted immunotherapeutic agents in different stages of clinical development. Keywords: B cell maturation antigen, BCMA, Belantamab mafodotin, CAR-T, Antibody-drug conjugate, Bispecific T cell engager Introduction B cell maturation antigen (BCMA) Recent advances in novel therapeutics such as prote- BCMA is encoded by a 2.92-kb TNFRSF17 gene located asome inhibitors (PI) and immunomodulatory drugs on the short arm of chromosome 16 (16p13.13) and (IMiD) have significantly improved the treatment out- composed of 3 exons separated by 2 introns (Fig. 1). comes in patients with multiple myeloma (MM) [1–8]. BCMA is a 184 amino acid and 20.2-kDa type III trans- However, most MM patients eventually relapse due to membrane glycoprotein, with the extracellular N the development of drug resistance [9]. In addition, terminus containing a conserved motif of 6 cysteines many of the current popular target antigens, such as [18–21]. -
Rheumatology and CTD
Section 16 Section Editor: G Narsimulu Rheumatology and CTD 206. Refractory Rheumatoid Arthritis 214. Treatment of SLE beyond Steroids Rohini Handa Rathindra Nath Sarkar, Rudrajit Paul 207. Difficulties in Rheumatoid Arthritis 215. Gout Is the Only Enemy That I Do Not Rajan Kumar Wish to Have at My Feet Anjana Pandey, Ajay Maurya, PK Maheshwari 208. Monoarthritis—A Clinical Dilemma to Internists Arup Kumar Kundu, Abhishek Kundu 216. Liver Dysfunction and NAFLD in RA: 209. Oral Targeted Treatments in RA—Update 2021 Is MTX Really a Culprit? Ramakrishna Rao Uppuluri, Sripurna Deepti Challa Kartik Nikhil Balankhe, Rishabh Ramu Nayak, Pulin Kumar Gupta 210. Biosimilars: Bane or Boon for India 217. Sexual Dysfunction in Rheumatic Diseases Durga Prasanna Misra, Pallavi Patro, Vikas Agarwal Vinod Ravindran 211. An Approach to Vasculitis 218. Interpretation of Common Investigations Packiamary Jerome in Rheumatology 212. How to Manage DMARDs Failure in RA? Renu Saigal, Amit Kansal, Vikram Raj Jain N Subramanian 213. IgG4-related Disease Harpreet Singh, Somdatta Giri, Anju Arya MU-206 (Sec-16).indd 1321 29-01-2021 15:25:29 MU-206 (Sec-16).indd 1322 29-01-2021 15:25:30 CHAPTER 206 Refractory Rheumatoid Arthritis Rohini Handa Abstract A sizeable number of patients with rheumatoid arthritis (RA) are unable to attain low disease activity or remission despite treatment. These difficult to treat (D2T) patients are labeled as refractory RA. The troika of D2T RA, as outlined by the European League against Rheumatism, comprises of treatment failure history, presence of active/symptomatic disease, and clinical perception. The approach to refractory RA is evolving. -

Antagonist Antibodies Against Various Forms of BAFF: Trimer, 60-Mer, and Membrane-Bound S
Supplemental material to this article can be found at: http://jpet.aspetjournals.org/content/suppl/2016/07/19/jpet.116.236075.DC1 1521-0103/359/1/37–44$25.00 http://dx.doi.org/10.1124/jpet.116.236075 THE JOURNAL OF PHARMACOLOGY AND EXPERIMENTAL THERAPEUTICS J Pharmacol Exp Ther 359:37–44, October 2016 Copyright ª 2016 by The American Society for Pharmacology and Experimental Therapeutics Unexpected Potency Differences between B-Cell–Activating Factor (BAFF) Antagonist Antibodies against Various Forms of BAFF: Trimer, 60-Mer, and Membrane-Bound s Amy M. Nicoletti, Cynthia Hess Kenny, Ashraf M. Khalil, Qi Pan, Kerry L. M. Ralph, Julie Ritchie, Sathyadevi Venkataramani, David H. Presky, Scott M. DeWire, and Scott R. Brodeur Immune Modulation and Biotherapeutics Discovery, Boehringer Ingelheim Pharmaceuticals, Inc., Ridgefield, Connecticut Received June 20, 2016; accepted July 18, 2016 Downloaded from ABSTRACT Therapeutic agents antagonizing B-cell–activating factor/B- human B-cell proliferation assay and in nuclear factor kB reporter lymphocyte stimulator (BAFF/BLyS) are currently in clinical assay systems in Chinese hamster ovary cells expressing BAFF development for autoimmune diseases; belimumab is the first receptors and transmembrane activator and calcium-modulator Food and Drug Administration–approved drug in more than and cyclophilin ligand interactor (TACI). In contrast to the mouse jpet.aspetjournals.org 50 years for the treatment of lupus. As a member of the tumor system, we find that BAFF trimer activates the human TACI necrosis factor superfamily, BAFF promotes B-cell survival and receptor. Further, we profiled the activities of two clinically ad- homeostasis and is overexpressed in patients with systemic vanced BAFF antagonist antibodies, belimumab and tabalumab. -
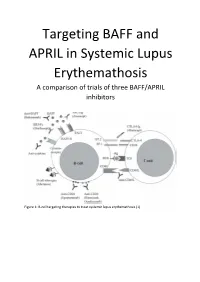
Targeting BAFF and APRIL in Systemic Lupus Erythemathosis a Comparison of Trials of Three BAFF/APRIL Inhibitors
Targeting BAFF and APRIL in Systemic Lupus Erythemathosis A comparison of trials of three BAFF/APRIL inhibitors Figure 1: B-cell targeting therapies to treat systemic lupus erythemathosis (1) Abstract: Systemic Lupus Erythemathosis (SLE) is a complex autoimmune disease. Diagnosis and prognosis are difficult and have a lot of confounders. Progress of the disease is thus followed by a number of measures, such as damage indices like SELENA/SLEDAI and BILAG, B-cell numbers, immunoglobulin levels, in particular autoantibodies such as anti-dsDNA antibodies, and complement C3 and C4 levels. B-cell proliferation and activation are overstimulated in SLE, particularly through the BAFF/APRIL stimulated pathways. A number of BAFF/APRIL targeting biologicals have been approved for use in treatment of SLE or are currently in clinical trials. Three of these are highlighted here: Belimumab, Blisibimod and Atacicept. Belimumab, a fully humanized anti-BAFF antibody, is already approved by the USFDA. In clinical studies it has been show to lower the damage index, B-cell numbers and immunoglobulin levels, it increases complement levels and may reduce the need for steroids. Blisibimod, a synthetic peptibody, is in stage II trials. Like Belimumab, Blisbimod lowers the damage index and B-cell numbers, increases complement levels and may reduce the need for steroids. Ataticept, a fusion protein, is in stage III trials. Atacicept also lowers the damage index, B-cell numbers and immunoglobulin levels, increases complement and may reduce the need for steroids. The differences are relatively small and to determine the most promising of these treatments close attention has to be paid to the data from trials. -

Three Is a Crowd
TREPAR 1600 No. of Pages 12 Review Three Rosetting[403_TD$IF] in Plasmodium falciparum Xue Yan Yam,1,3 Makhtar Niang,2,3 Kripa Gopal Madnani,1,3 and Peter R. Preiser1,* The intracellular malaria parasites extensively modify host erythrocytes to allow Trends nutrient uptake, ensure homeostasis, and evade the host’s immune response. Rosetting, the binding of uninfected To achieve this, the parasite exports several proteins to the erythrocyte surface. RBCs to a parasite-infected RBC In Plasmodium falciparum, the parasite responsible for the most severe form of (iRBC), has been directly linked to human malaria, three major variant surface antigen families – PfEMP1, STE- the severity of clinical disease. VOR, and RIFIN – have been implicated in contributing to immune evasion, Three parasite protein families, parasite sequestration, and parasite-mediated rosetting of uninfected eryth- PfEMP1, STEVOR, and RIFIN, mediate rosetting in Plasmodium falciparum. rocytes. Sequestration and rosetting have been linked to parasite-mediated pathology, making the variant surface antigens of P. falciparum major virulence Sequential timing of surface expres- factors. Here we review our current understanding of rosetting mechanism, sion of PfEMP1, RIFIN, and STEVOR fi on iRBC suggests that the parasite has recent ndings of STEVOR, RIFIN-mediated rosetting, and their implication on developed three different rosette for- the severity and pathology of the disease. mation mechanisms, implicating a cri- tical function for parasite survival. Plasmodium Variant Surface Antigens of Parasites: A Role in Rosetting PfEMP1 mediates rosetting through Plasmodium parasites have a complex life cycle involving a mosquito vector and a mammalian CR1, heparan sulfate, and blood group host. -

1 the BAFF/APRIL System in SLE Pathogenesis. Fabien B Vincent1
. Fabien B Vincent1, Eric F Morand2, Pascal Schneider3 and Fabienne Mackay1 1 Department of Immunology, Monash University, Central Clinical School, Alfred Medical Research and Education Precinct (AMREP), 89 Commercial Road, Melbourne, Victoria 3004, Australia 2 Monash University Centre for Inflammatory Diseases, Southern Clinical School, Monash Medical Centre, 246 Clayton Road, Clayton, Victoria, 3168, Australia 3 Department of Biochemistry, University of Lausanne, Boveresses 155, 1066 Epalinges, Switzerland Abstract Systemic lupus erythematosus (SLE) is characterized by multisystem immune-mediated injury in the setting of autoimmunity to nuclear antigens. The clinical heterogeneity of SLE, the absence of universally agreed clinical trial end points, and the paucity of validated therapeutic targets have, historically, contributed to a lack of novel treatments for SLE. However, in 2011, a therapeutic monoclonal antibody that neutralizes the cytokine TNF ligand superfamily member 13B (also known as B-cell-activating factor of the TNF family [BAFF]), belimumab, became the first targeted therapy for SLE to have efficacy in a randomized clinical trial. Because of its specificity, the efficacy of belimumab provides an opportunity to increase understanding of SLE pathophysiology. Although belimumab depletes B cells, this effect is not as powerful as that of other B-cell-directed therapies that have not been proven efficacious in randomized clinical trials. In this article, therefore, we review results suggesting that neutralizing BAFF can have effects on the immune system other than depletion of B cells. We also identify aspects of the BAFF system for which data in relation to SLE are still missing, and we suggest studies to investigate the pathogenesis of SLE and ways to refine anti-BAFF therapies. -

Aggrecan (A1960)
Aggrecan from bovine articular cartilage Catalog Number A1960 Storage Temperature –20 °C Product Description References Aggrecan is the major structural proteoglycan found in 1. Hardingham, T.E., and Muir, H., Biochim. Biophys. the extracellular matrix of cartilage. It has a molecular Acta, 279, 401-405 (1972). mass >2,500 kDa. The core protein (210–250 kDa) has 2. Hedlund, H., et al., Association of the aggrecan 100–150 glycosaminoglycan (GAG) chains attached to keratan sulfate-rich region with collagen in bovine it. The majority of the GAG chains are chondroitin/ articular cartilage. J. Biol. Chem., 274, 5777-5781 dermatan sulfate with the remainder being keratan (1999). sulfate. This structural molecule produces a rigid, 3. Cao, L., and Yang, B.B., Chondrocyte apoptosis reversibly deformable gel that resists compression. It induced by aggrecan G1 domain as a result of combines with hyaluronic acid to form very large decreased cell adhesion. Exp. Cell Res., 246, 527- macromolecular complexes. Addition of small amounts 537 (1999). (0.1–2% w/w) of hyaluronic acid to a solution of 4. Bolton, M.C., et al., Age-related changes in the aggrecan (2 mg/ml) results in the formation of a synthesis of link protein and aggrecan in human complex with an increased hydrodynamic volume and articular cartilage: implications for aggregate in a significant increase (30–40%) in the relative stability. Biochem. J., 337, 77-82 (1999). viscosity of the solution. 5. Arner, E.C., et al., Generation and Characterization of Aggrecanase. A soluble, cartilage-derived Aggrecan is a critical component for cartilage structure aggrecan-degrading activity. -

Mucins: the Old, the New and the Promising Factors in Hepatobiliary Carcinogenesis
International Journal of Molecular Sciences Review Mucins: the Old, the New and the Promising Factors in Hepatobiliary Carcinogenesis Aldona Kasprzak 1,* and Agnieszka Adamek 2 1 Department of Histology and Embryology, Poznan University of Medical Sciences, Swiecicki Street 6, 60-781 Pozna´n,Poland 2 Department of Infectious Diseases, Hepatology and Acquired Immunodeficiencies, University of Medical Sciences, Szwajcarska Street 3, 61-285 Pozna´n,Poland; [email protected] * Correspondence: [email protected]; Tel.: +48-61-8546441; Fax: +48-61-8546440 Received: 25 February 2019; Accepted: 10 March 2019; Published: 14 March 2019 Abstract: Mucins are large O-glycoproteins with high carbohydrate content and marked diversity in both the apoprotein and the oligosaccharide moieties. All three mucin types, trans-membrane (e.g., MUC1, MUC4, MUC16), secreted (gel-forming) (e.g., MUC2, MUC5AC, MUC6) and soluble (non-gel-forming) (e.g., MUC7, MUC8, MUC9, MUC20), are critical in maintaining cellular functions, particularly those of epithelial surfaces. Their aberrant expression and/or altered subcellular localization is a factor of tumour growth and apoptosis induced by oxidative stress and several anti-cancer agents. Abnormal expression of mucins was observed in human carcinomas that arise in various gastrointestinal organs. It was widely believed that hepatocellular carcinoma (HCC) does not produce mucins, whereas cholangiocarcinoma (CC) or combined HCC-CC may produce these glycoproteins. However, a growing number of reports shows that mucins can be produced by HCC cells that do not exhibit or are yet to undergo, morphological differentiation to biliary phenotypes. Evaluation of mucin expression levels in precursors and early lesions of CC, as well as other types of primary liver cancer (PLC), conducted in in vitro and in vivo models, allowed to discover the mechanisms of their action, as well as their participation in the most important signalling pathways of liver cystogenesis and carcinogenesis.