Multiple Roles for the Extracelllular Matrix Protein Tenascin-X in Nerve
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

V·M·I University Microfilms International a Bell & Howell Information Company 300 North Zeeb Road, Ann Arbor
Characterization of the cloned neurokinin A receptor transfected in murine fibroblasts Item Type text; Dissertation-Reproduction (electronic) Authors Henderson, Alden Keith. Publisher The University of Arizona. Rights Copyright © is held by the author. Digital access to this material is made possible by the University Libraries, University of Arizona. Further transmission, reproduction or presentation (such as public display or performance) of protected items is prohibited except with permission of the author. Download date 27/09/2021 18:29:56 Link to Item http://hdl.handle.net/10150/185828 1/. INFORMATION TO USERS This manuscript has been reproduced from the microfilm master. UMI films the text directly from the original or copy submitted. Thus, some thesis and dissertation copies are in typewriter face, while others may be from any type of computer printer. The quality of this reproduction is dependent upon the quality of the copy submitted. Broken or indistinct print, colored or poor quality illustrations and photographs, print bleed through, substandard margins, and improper alignment can adversely affect reproduction. In the unlikely event that the author did not send UMI a complete manuscript and there are missing pages, these will be noted. Also, if unauthorized copyright material had to be removed, a note. will indicate the deletion. Oversize materials (e.g., maps, drawings, charts) are reproduced by sectioning the original, beginning at the upper left-hand corner and continuing from left to right in equal sections with small overlaps. Each original is also photographed in one exposure and is included in reduced form at the back of the book. Photographs included in the original manuscript have been reproduced xerographically in this copy. -

The Extracellular Matrix: an Accomplice in Gastric Cancer Development and Progression
cells Review The Extracellular Matrix: An Accomplice in Gastric Cancer Development and Progression Ana Margarida Moreira 1,2,3, Joana Pereira 1,2,4, Soraia Melo 1,2,4 , Maria Sofia Fernandes 1,2, Patrícia Carneiro 1,2 , Raquel Seruca 1,2,4 and Joana Figueiredo 1,2,* 1 Epithelial Interactions in Cancer Group, i3S-Instituto de Investigação e Inovação em Saúde, Universidade do Porto, 4200-135 Porto, Portugal; [email protected] (A.M.M.); [email protected] (J.P.); [email protected] (S.M.); [email protected] (M.S.F.); [email protected] (P.C.); [email protected] (R.S.) 2 Institute of Molecular Pathology and Immunology of the University of Porto (IPATIMUP), 4200-135 Porto, Portugal 3 Institute of Biomedical Sciences Abel Salazar (ICBAS), University of Porto, 4050-313 Porto, Portugal 4 Medical Faculty, University of Porto, 4200-319 Porto, Portugal * Correspondence: jfi[email protected]; Tel.: +351-220408800; Fax: +351-225570799 Received: 15 January 2020; Accepted: 6 February 2020; Published: 8 February 2020 Abstract: The extracellular matrix (ECM) is a dynamic and highly organized tissue structure, providing support and maintaining normal epithelial architecture. In the last decade, increasing evidence has emerged demonstrating that alterations in ECM composition and assembly strongly affect cellular function and behavior. Even though the detailed mechanisms underlying cell-ECM crosstalk are yet to unravel, it is well established that ECM deregulation accompanies the development of many pathological conditions, such as gastric cancer. Notably, gastric cancer remains a worldwide concern, representing the third most frequent cause of cancer-associated deaths. Despite increased surveillance protocols, patients are usually diagnosed at advanced disease stages, urging the identification of novel diagnostic biomarkers and efficient therapeutic strategies. -

Bruch's Membrane Abnormalities in PRDM5-Related Brittle Cornea
Porter et al. Orphanet Journal of Rare Diseases (2015) 10:145 DOI 10.1186/s13023-015-0360-4 RESEARCH Open Access Bruch’s membrane abnormalities in PRDM5-related brittle cornea syndrome Louise F. Porter1,2,3, Roberto Gallego-Pinazo4, Catherine L. Keeling5, Martyna Kamieniorz5, Nicoletta Zoppi6, Marina Colombi6, Cecilia Giunta7, Richard Bonshek2,8, Forbes D. Manson1 and Graeme C. Black1,9* Abstract Background: Brittle cornea syndrome (BCS) is a rare, generalized connective tissue disorder associated with extreme corneal thinning and a high risk of corneal rupture. Recessive mutations in transcription factors ZNF469 and PRDM5 cause BCS. Both transcription factors are suggested to act on a common pathway regulating extracellular matrix genes, particularly fibrillar collagens. We identified bilateral myopic choroidal neovascularization as the presenting feature of BCS in a 26-year-old-woman carrying a novel PRDM5 mutation (p.Glu134*). We performed immunohistochemistry of anterior and posterior segment ocular tissues, as expression of PRDM5 in the eye has not been described, or the effects of PRDM5-associated disease on the retina, particularly the extracellular matrix composition of Bruch’smembrane. Methods: Immunohistochemistry using antibodies against PRDM5, collagens type I, III, and IV was performed on the eyes of two unaffected controls and two patients (both with Δ9-14 PRDM5). Expression of collagens, integrins, tenascin and fibronectin in skin fibroblasts of a BCS patient with a novel p.Glu134* PRDM5 mutation was assessed using immunofluorescence. Results: PRDM5 is expressed in the corneal epithelium and retina. We observe reduced expression of major components of Bruch’s membrane in the eyes of two BCS patients with a PRDM5 Δ9-14 mutation. -

Three Rat Preprotachykinin Mrnas Encode the Neuropeptides Substance P and Neurokinin a (Corpus Striatum/Tachykinin Peptides/Differential RNA Splicing) J
Proc. Natl. Acad. Sci. USA Vol. 84, pp. 881-885, February 1987 Neurobiology Three rat preprotachykinin mRNAs encode the neuropeptides substance P and neurokinin A (corpus striatum/tachykinin peptides/differential RNA splicing) J. E. KRAUSE*, J. M. CHIRGWINt, M. S. CARTER, Z. S. XU, AND A. D. HERSHEY Department of Anatomy and Neurobiology, Washington University School of Medicine, 660 South Euclid Avenue, St. Louis, MO 63110 Communicated by Gerald D. Fischbach, September 17, 1986 ABSTRACT Synthetic oligonucleotides were used to yields the structural differences of these peptide precursors. screen a rat striatal cDNA library for sequences corresponding A preliminary account of this work has appeared (7). to the tachykinin peptides substance P and neurokinin A. The cDNA library was constructed from RNA isolated from the EXPERIMENTAL PROCEDURES rostral portion of the rat corpus striatum, the site of stri- atonigral cell bodies. Two types of cDNAs were isolated and Materials. Avian myeloblastosis reverse transcriptase was dermed by restriction enzyme analysis and DNA sequencing to obtained from J. Beard (Life Sciences, St. Petersburg, FL). encode both substance P and neurokinin A. The two predicted Restriction endonucleases, terminal nucleotidyltransferase, preprotachykinin protein precursors (130 and 115 amino acids DNA polymerase I and Klenow fragment of DNA polymer- in length) differ from each other by a pentadecapeptide ase I, T4 polynucleotide kinase, and SP6 polymerase were sequence between the two tachykinin sequences, and both purchased from Bethesda Research Laboratories, New En- precursors possess appropriate processing signals for sub- gland Biolabs, or Promega Biotec (Madison, WI). S1 nucle- stance P and neurokinin A production. The presence of a third ase was from Sigma, and oligo(dC)-tailed Sst I-digested preprotachykinin mRNA of minor abundance in rat striatum pUC19 was a gift of P. -
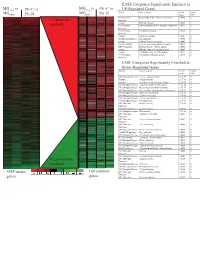
Supplement 1 Microarray Studies
EASE Categories Significantly Enriched in vs MG vs vs MGC4-2 Pt1-C vs C4-2 Pt1-C UP-Regulated Genes MG System Gene Category EASE Global MGRWV Pt1-N RWV Pt1-N Score FDR GO Molecular Extracellular matrix cellular construction 0.0008 0 110 genes up- Function Interpro EGF-like domain 0.0009 0 regulated GO Molecular Oxidoreductase activity\ acting on single dono 0.0015 0 Function GO Molecular Calcium ion binding 0.0018 0 Function Interpro Laminin-G domain 0.0025 0 GO Biological Process Cell Adhesion 0.0045 0 Interpro Collagen Triple helix repeat 0.0047 0 KEGG pathway Complement and coagulation cascades 0.0053 0 KEGG pathway Immune System – Homo sapiens 0.0053 0 Interpro Fibrillar collagen C-terminal domain 0.0062 0 Interpro Calcium-binding EGF-like domain 0.0077 0 GO Molecular Cell adhesion molecule activity 0.0105 0 Function EASE Categories Significantly Enriched in Down-Regulated Genes System Gene Category EASE Global Score FDR GO Biological Process Copper ion homeostasis 2.5E-09 0 Interpro Metallothionein 6.1E-08 0 Interpro Vertebrate metallothionein, Family 1 6.1E-08 0 GO Biological Process Transition metal ion homeostasis 8.5E-08 0 GO Biological Process Heavy metal sensitivity/resistance 1.9E-07 0 GO Biological Process Di-, tri-valent inorganic cation homeostasis 6.3E-07 0 GO Biological Process Metal ion homeostasis 6.3E-07 0 GO Biological Process Cation homeostasis 2.1E-06 0 GO Biological Process Cell ion homeostasis 2.1E-06 0 GO Biological Process Ion homeostasis 2.1E-06 0 GO Molecular Helicase activity 2.3E-06 0 Function GO Biological -

Binding of Recombinant Human Cytokeratin 19 to Laminin
CELL STRUCTURE AND FUNCTION 25: 171–175 (2000) © 2000 by Japan Society for Cell Biology Binding of Recombinant Human Cytokeratin 19 to Laminin: A Possible Role in Interaction between Intermediate Filament Derived from Epithelial Cells and Extracellular Matrixes Naomi Dobashi1, Jiro Fujita1,*, Masayuki Murota2, Yuji Ohtsuki3, Shuji Bandoh1, Yutaka Ueda1, Kazutaka Dohmoto1, Satoko Hojo1, Mikio Nishioka2, Toshihiko Ishida, and Jiro Takahara1 1First Department of Internal Medicine, Kagawa Medical University, Kagawa 2Third Department of Internal Medicine, Kagawa Medical University, Kagawa 3Department of Pathology, Kochi Medical School, Kochi, Japan ABSTRACT. Cytokeratin 8 (CK8) and cytokeratin 19 (CK19) is a specific cytoskeletal component of simple epi- thelia, including bronchial epithelial cells. We hypothesized that CK8 or CK19 released from epithelial cells may bind to and cause damage to extracellular matrixes through binding of anti-CK8 or anti-CK19 autoantibodies. In the present study, bindings of recombinant human CK8 and CK19 to laminin (both derived from mouse sarcoma cells and human), collagen, gelatin, and fibronectin were evaluated by a modified enzyme-linked immunosorbent assay (ELISA). In addition, binding of CK19 to laminin was also confirmed by inhibition assay. As a result, CK19 strongly bound to mouse laminin as well as human laminin. Pretreatment with laminin significantly reduced the binding of CK19 to laminin. However, binding of recombinant CK19 to laminin was not demonstrated by Western immunoblot, suggesting that SDS treatment of laminin diminished the binding. These results suggest that released CK19 from epithelial cells may have played a role in the damage of basement membrane by accumulation of an immune complex composed by CK19 and anti-CK19 autoantibody. -

Congenital Muscular Dystrophy Due to Laminin Α2 (Merosin) Deficiency (MDC1A) in an Ethnic Malay Girl 1MK Thong, 3Sofiah Ali,4 YE Park, 5DS Kim, 6KJ Goh, 2KT Wong
Neurology Asia 2017; 22(2) : 155 – 159 Congenital muscular dystrophy due to laminin α2 (merosin) deficiency (MDC1A) in an ethnic Malay girl 1MK Thong, 3Sofiah Ali, 4YE Park, 5DS Kim, 6KJ Goh, 2KT Wong 1Departments of Paediatrics, 2Pathology and 6Medicine, Faculty of Medicine, University of Malaya, Kuala Lumpur, Malaysia; 3Sime Darby Medical Centre, Subang Jaya, Selangor, Malaysia; 4Department of Neurology and Biomedical Research Institute, Pusan National University Hospital, Busan, Korea; 5Department of Neurology, Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Yangsan, Korea Abstract We report the first known ethnic Malay patient with laminin alpha-2 (merosin) deficiency (MDC1A), a subtype of congenital muscular dystrophy (CMD)as a result of novel LAMA2 gene mutations. The 21-month-old female presented with hypotonia at birth and gross motor delay of her distal lower limbs. Physical examination showed generalised hypotonia, hyporeflexia and myopathic facies but good cognitive functions. Serum creatine kinase was elevated and white matter changes were detected in the brain MRI. Muscle biopsy showed dystrophic changes with complete laminin α2 deficiency by immunohistochemistry. Mutation analysis of LAMA2 showed compound heterozygote at exon 21, c.2888delG(p.Gly963Alafs*111) and exon 34, c.4886dupC(p.Pro1629Profs*40) leading to premature stop codon for each of the frameshift mutations. Patient review at seven years of age showed satisfactory cognitive functions despite having contractures and weakness. Genetic testing of LAMA2 related muscular dystrophy facilitated the earlier diagnosis of MDC1A and genetic counselling for this family. Keywords: laminin alpha-2 deficiency; merosin deficiency. LAMA2, Malaysia, congenital muscular dystrophy, MDC1A INTRODUCTION mutations in the laminin alpha-2 (LAMA2)gene. -

Identification of a New Myotropic Decapeptide from the Skin Secretion of the Red-Eyed Leaf Frog, Agalychnis Callidryas
PLOS ONE RESEARCH ARTICLE Identification of a new myotropic decapeptide from the skin secretion of the red-eyed leaf frog, Agalychnis callidryas Yitian Gao1,2☯¤, Renjie Li2☯, Wenqing Yang1, Mei Zhou2, Lei Wang2, Chengbang Ma2, 2 2 2 3 Xinping Xi , Tianbao Chen , Chris Shaw , Di WuID * 1 College of Life and Environmental Science, Wenzhou University, Wenzhou, Zhejiang, China, 2 Natural Drug Discovery Group, School of Pharmacy, Queen's University Belfast, Belfast, Northern Ireland, United Kingdom, 3 Chemical Biology Research Center, School of Pharmaceutical Sciences, Wenzhou Medical a1111111111 University, Wenzhou, Zhejiang, China a1111111111 a1111111111 ☯ These authors contributed equally to this work. a1111111111 ¤ Current address: College of Life and Environmental Science, Wenzhou University, Wenzhou, Zhejiang, a1111111111 China * [email protected] Abstract OPEN ACCESS Bradykinin-related peptides (BRPs) family is one of the most significant myotropic peptide Citation: Gao Y, Li R, Yang W, Zhou M, Wang L, Ma C, et al. (2020) Identification of a new families derived from frog skin secretions. Here, a novel BRP callitide was isolated and iden- myotropic decapeptide from the skin secretion of tified from the red-eyed leaf frog, Agalychnis callidryas, with atypical primary structure the red-eyed leaf frog, Agalychnis callidryas. PLoS FRPAILVRPK-NH2. The mature peptide was cleaved N-terminally at a classic propeptide ONE 15(12): e0243326. https://doi.org/10.1371/ journal.pone.0243326 convertase cleavage site (-KR-) and at the C-terminus an unusual -GKGKGK sequence was removed using the first G residue as an amide donor for the C-terminally-located K resi- Editor: Joseph Banoub, Fisheries and Oceans Canada, CANADA due. -

Blood Vitronectin Is a Major Activator of LIF and IL-6 in the Brain Through Integrin–FAK and Upar Signaling Matthew P
© 2018. Published by The Company of Biologists Ltd | Journal of Cell Science (2018) 131, jcs202580. doi:10.1242/jcs.202580 RESEARCH ARTICLE Blood vitronectin is a major activator of LIF and IL-6 in the brain through integrin–FAK and uPAR signaling Matthew P. Keasey1, Cuihong Jia1, Lylyan F. Pimentel1,2, Richard R. Sante1, Chiharu Lovins1 and Theo Hagg1,* ABSTRACT Microglia and astrocytes express the VTN receptors αvβ3 and α β We defined how blood-derived vitronectin (VTN) rapidly and potently v 5 integrin (Herrera-Molina et al., 2012; Kang et al., 2008; activates leukemia inhibitory factor (LIF) and pro-inflammatory Milner, 2009; Welser-Alves et al., 2011). Microglia and astrocytes, interleukin 6 (IL-6) in vitro and after vascular injury in the brain. as well as endothelial cells, are major producers of pro- α in vitro Treatment with VTN (but not fibrinogen, fibronectin, laminin-111 or inflammatory cytokines, such as IL-6 and TNF , and collagen-I) substantially increased LIF and IL-6 within 4 h in after traumatic or ischemic injury to the brain (Banner et al., 1997; C6-astroglioma cells, while VTN−/− mouse plasma was less effective Erta et al., 2012; Lau and Yu, 2001) or upon self-induction by IL-6 than that from wild-type mice. LIF and IL-6 were induced by (Van Wagoner and Benveniste, 1999). IL-6 is a major regulator of a intracerebral injection of recombinant human (rh)VTN in mice, but variety of inflammatory disorders and a target for therapies (Hunter induction seen upon intracerebral hemorrhage was less in VTN−/− and Jones, 2015). -

WES Gene Package Multiple Congenital Anomalie.Xlsx
Whole Exome Sequencing Gene package Multiple congenital anomalie, version 5, 1‐2‐2018 Technical information DNA was enriched using Agilent SureSelect Clinical Research Exome V2 capture and paired‐end sequenced on the Illumina platform (outsourced). The aim is to obtain 8.1 Giga base pairs per exome with a mapped fraction of 0.99. The average coverage of the exome is ~50x. Duplicate reads are excluded. Data are demultiplexed with bcl2fastq Conversion Software from Illumina. Reads are mapped to the genome using the BWA‐MEM algorithm (reference: http://bio‐bwa.sourceforge.net/). Variant detection is performed by the Genome Analysis Toolkit HaplotypeCaller (reference: http://www.broadinstitute.org/gatk/). The detected variants are filtered and annotated with Cartagenia software and classified with Alamut Visual. It is not excluded that pathogenic mutations are being missed using this technology. At this moment, there is not enough information about the sensitivity of this technique with respect to the detection of deletions and duplications of more than 5 nucleotides and of somatic mosaic mutations (all types of sequence changes). HGNC approved Phenotype description including OMIM phenotype ID(s) OMIM median depth % covered % covered % covered gene symbol gene ID >10x >20x >30x A4GALT [Blood group, P1Pk system, P(2) phenotype], 111400 607922 101 100 100 99 [Blood group, P1Pk system, p phenotype], 111400 NOR polyagglutination syndrome, 111400 AAAS Achalasia‐addisonianism‐alacrimia syndrome, 231550 605378 73 100 100 100 AAGAB Keratoderma, palmoplantar, -

Proquest Dissertations
Localization of tachykinins and their receptormRNAs in the human hypothalamus and basal forebrain Item Type text; Dissertation-Reproduction (electronic) Authors Chawla, Monica Kapoor, 1950- Publisher The University of Arizona. Rights Copyright © is held by the author. Digital access to this material is made possible by the University Libraries, University of Arizona. Further transmission, reproduction or presentation (such as public display or performance) of protected items is prohibited except with permission of the author. Download date 25/09/2021 04:06:48 Link to Item http://hdl.handle.net/10150/282168 INFORMATION TO USERS This manuscript has been reproduced from the microfihn master. UMI fihns the text directly from the original or copy submitted. Thus, some thesis and dissertation copies are in typewriter face, while others may be from any type of computer printer. The quality of this reproduction is dependent upon the quality of the copy submitted. Broken or indistinct print, colored or poor quality illustrations and photographs, print bleedthrough, substandard margins, and improper alignment can adversely afifect reproduction. In the unlikely event that the author did not send UMI a complete manuscript and there are missing pages, these will be noted. Also, if unauthorized copyright material had to be removed, a note will indicate the deletion. Oversize materials (e.g., maps, drawings, charts) are reproduced by sectioning the original, beginning at the upper left-hand comer and continuing from left to right in equal sections with small overlaps. Each original is also photographed in one exposure and is included in reduced form at the back of the book. Photographs included in the original manuscript have been reproduced xerographically in this copy. -
![Functional Expression of a Novel Human Neurokinin-3 Receptor Homolog That Binds [3H]Senktide and [125I-Mephe7]Neurokinin B](https://docslib.b-cdn.net/cover/2790/functional-expression-of-a-novel-human-neurokinin-3-receptor-homolog-that-binds-3h-senktide-and-125i-mephe7-neurokinin-b-1002790.webp)
Functional Expression of a Novel Human Neurokinin-3 Receptor Homolog That Binds [3H]Senktide and [125I-Mephe7]Neurokinin B
Proc. Natl. Acad. Sci. USA Vol. 94, pp. 310–315, January 1997 Pharmacology Functional expression of a novel human neurokinin-3 receptor homolog that binds [3H]senktide and [125I-MePhe7]neurokinin B, and is responsive to tachykinin peptide agonists J. E. KRAUSE*, P. T. STAVETEIG,J.NAVE MENTZER,S.K.SCHMIDT,J.B.TUCKER,R.M.BRODBECK, J.-Y. BU, AND V. V. KARPITSKIY Department of Anatomy and Neurobiology, Washington University School of Medicine, 660 South Euclid Avenue, Box 8108, St. Louis, MO 63110 Communicated by Avram Goldstein, Stanford University, Stanford, CA, November 8, 1996 (received for review September 21, 1996) ABSTRACT In 1992, Xie et al. identified a cDNA sequence Due to the homology among receptors in the G-protein- in the expression cloning search for the k opioid receptor. coupled receptor superfamily, several putative receptor se- When the cDNA was expressed in Cos-7 cells, binding of opioid quences have been cloned in which the natural ligand has not compounds was observed to be of low affinity and without k, been identified (4). In addition, various genetic strategies have m,ordselectivity [Xie, G.-X., Miyajima, A. and Goldstein, A. resulted in the identification of receptor-like sequences in (1992) Proc. Natl. Acad. Sci. USA 89, 4124–4128]. This cDNA which no known ligand has been determined (e.g., see ref. 5). was highly homologous to the human neurokinin-3 (NK-3) The identification of these so-called ‘‘orphan’’ receptors has receptor sequence, and displayed lower homology to NK-1 and also come about in the search for other receptors using more NK-2 sequences.