Discovery and Study of Cutaneous Leishmaniasis in Karamay of Xinjiang, West China Li-Ren Guan1*, Yuan-Qing Yang1, Jing-Qi Qu1, Hao-Yuan Ren2 and Jun-Jie Chai3
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Glaciers in Xinjiang, China: Past Changes and Current Status
water Article Glaciers in Xinjiang, China: Past Changes and Current Status Puyu Wang 1,2,3,*, Zhongqin Li 1,3,4, Hongliang Li 1,2, Zhengyong Zhang 3, Liping Xu 3 and Xiaoying Yue 1 1 State Key Laboratory of Cryosphere Science/Tianshan Glaciological Station, Northwest Institute of Eco-Environment and Resources, Chinese Academy of Sciences, Lanzhou 730000, China; [email protected] (Z.L.); [email protected] (H.L.); [email protected] (X.Y.) 2 University of Chinese Academy of Sciences, Beijing 100049, China 3 College of Sciences, Shihezi University, Shihezi 832000, China; [email protected] (Z.Z.); [email protected] (L.X.) 4 College of Geography and Environment Sciences, Northwest Normal University, Lanzhou 730070, China * Correspondence: [email protected] Received: 18 June 2020; Accepted: 11 August 2020; Published: 24 August 2020 Abstract: The Xinjiang Uyghur Autonomous Region of China is the largest arid region in Central Asia, and is heavily dependent on glacier melt in high mountains for water supplies. In this paper, glacier and climate changes in Xinjiang during the past decades were comprehensively discussed based on glacier inventory data, individual monitored glacier observations, recent publications, as well as meteorological records. The results show that glaciers have been in continuous mass loss and dimensional shrinkage since the 1960s, although there are spatial differences between mountains and sub-regions, and the significant temperature increase is the dominant controlling factor of glacier change. The mass loss of monitored glaciers in the Tien Shan has accelerated since the late 1990s, but has a slight slowing after 2010. Remote sensing results also show a more negative mass balance in the 2000s and mass loss slowing in the latest decade (2010s) in most regions. -
![BILLING CODE 3510-33-P DEPARTMENT of COMMERCE Bureau of Industry and Security 15 CFR Part 744 [Docket No. 210617-0134] RIN 0694](https://docslib.b-cdn.net/cover/8282/billing-code-3510-33-p-department-of-commerce-bureau-of-industry-and-security-15-cfr-part-744-docket-no-210617-0134-rin-0694-278282.webp)
BILLING CODE 3510-33-P DEPARTMENT of COMMERCE Bureau of Industry and Security 15 CFR Part 744 [Docket No. 210617-0134] RIN 0694
This document is scheduled to be published in the Federal Register on 06/24/2021 and available online at BILLING CODE 3510-33-P federalregister.gov/d/2021-13395, and on govinfo.gov DEPARTMENT OF COMMERCE Bureau of Industry and Security 15 CFR Part 744 [Docket No. 210617-0134] RIN 0694-AI56 Addition of Certain Entities to the Entity List AGENCY: Bureau of Industry and Security, Commerce ACTION: Final rule. SUMMARY: This final rule amends the Export Administration Regulations (EAR) by adding five entities to the Entity List. These five entities have been determined by the United States Government to be acting contrary to the foreign policy interests of the United States and will be listed on the Entity List under the destination of the People’s Republic of China (China). DATE: This rule is effective [INSERT DATE OF PUBLICATION IN THE FEDERAL REGISTER]. FOR FURTHER INFORMATION CONTACT: Chair, End-User Review Committee, Office of the Assistant Secretary, Export Administration, Bureau of Industry and Security, Department of Commerce, Phone: (202) 482-5991, Email: [email protected]. SUPPLEMENTARY INFORMATION: Background The Entity List (supplement no. 4 to part 744 of the EAR) identifies entities reasonably believed to be involved in, or to pose a significant risk of being or becoming involved in, activities contrary to the national security or foreign policy interests of the United States. The Export Administration Regulations (EAR) (15 CFR parts 730-774) impose additional license requirements on, and limit the availability of most license exceptions for, exports, reexports, and transfers (in country) to listed entities. The license review policy for each listed entity is identified in the “License review policy” column on the Entity List, and the impact on the availability of license exceptions is described in the relevant Federal Register document adding entities to the Entity List. -

Water Supply and Usage in Central Asia, Tian Shan Basin Polina Lemenkova
Water Supply and Usage in Central Asia, Tian Shan Basin Polina Lemenkova To cite this version: Polina Lemenkova. Water Supply and Usage in Central Asia, Tian Shan Basin. Civil Engineer- ing, Architecture and Environmental Protection. PhiDAC-2012, Sep 2012, Niš, Serbia. pp.331-338, 10.6084/m9.figshare.7211999. hal-02023017 HAL Id: hal-02023017 https://hal.archives-ouvertes.fr/hal-02023017 Submitted on 22 Mar 2019 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Distributed under a Creative Commons CC0 - Public Domain Dedication| 4.0 International License IV INTERNATIONAL SYMPOSIUM FOR STUDENTS OF DOCTORAL STUDIES IN THE FIELDS OF CIVIL ENGINEERING, ARCHITECTURE AND ENVIRONMENTAL PROTECTION Polina Lemenkova1 WATER SUPPLY AND USAGE IN CENTRAL ASIA, TIAN SHAN BASIN Abstract: The paper focuses on analysis of Central Asian hydro-energetic system and water usage in Tian Shan region. Tian Shan system is important water resource in Central Asia: mountains river waters are intensely taken for hydropower energy, urban systems, irrigation. But geopolitics in Tian Shan is difficult: it crosses five densely populated countries. Current problem consists in water delivery between territories located in the highlands with excellent water supply and those located in valleys with water shortage. -

Uyghur Dispossession, Culture Work and Terror Capitalism in a Chinese Global City Darren T. Byler a Dissertati
Spirit Breaking: Uyghur Dispossession, Culture Work and Terror Capitalism in a Chinese Global City Darren T. Byler A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy University of Washington 2018 Reading Committee: Sasha Su-Ling Welland, Chair Ann Anagnost Stevan Harrell Danny Hoffman Program Authorized to Offer Degree: Anthropology ©Copyright 2018 Darren T. Byler University of Washington Abstract Spirit Breaking: Uyghur Dispossession, Culture Work and Terror Capitalism in a Chinese Global City Darren T. Byler Chair of the Supervisory Committee: Sasha Su-Ling Welland, Department of Gender, Women, and Sexuality Studies This study argues that Uyghurs, a Turkic-Muslim group in contemporary Northwest China, and the city of Ürümchi have become the object of what the study names “terror capitalism.” This argument is supported by evidence of both the way state-directed economic investment and security infrastructures (pass-book systems, webs of technological surveillance, urban cleansing processes and mass internment camps) have shaped self-representation among Uyghur migrants and Han settlers in the city. It analyzes these human engineering and urban planning projects and the way their effects are contested in new media, film, television, photography and literature. It finds that this form of capitalist production utilizes the discourse of terror to justify state investment in a wide array of policing and social engineering systems that employs millions of state security workers. The project also presents a theoretical model for understanding how Uyghurs use cultural production to both build and refuse the development of this new economic formation and accompanying forms of gendered, ethno-racial violence. -

Late Cretaceous–Palaeogene Topography of the Chinese Tian Shan
Earth and Planetary Science Letters 499 (2018) 95–106 Contents lists available at ScienceDirect Earth and Planetary Science Letters www.elsevier.com/locate/epsl Late Cretaceous–Palaeogene topography of the Chinese Tian Shan: New insights from geomorphology and sedimentology ∗ Marc Jolivet a, , Laurie Barrier b, Olivier Dauteuil a, Amandine Laborde b, Qian Li c, Bettina Reichenbacher d, Speranta-Maria Popescu e, Jingeng Sha f, Zhaojie Guo c a Univ Rennes, CNRS, Géosciences Rennes, UMR 6118, CNRS, F-35000 Rennes, France b Institut de Physique du Globe de Paris, Sorbonne Paris Cité, Université Paris Diderot, UMR 7154 CNRS, Paris, France c Key Laboratory of Orogenic Belts and Crustal Evolution, Ministry of Education, School of Earth and Space Sciences, Peking University, Beijing, 100871, China d Department für Geo- und Umweltwissenschaften, Paläontologie & Geobiologie, Ludwig-Maximilians-Universität München, Richard-Wagner-Str. 10, 80333 München, Germany e Geobiostratadata Consulting, 385 Route du Mas Rillier, 69140, Rillieux la Pape, France f Nanjing Institute of Geology and Palaeontology, Chinese Academy of Science, Nanjing 210008, China a r t i c l e i n f o a b s t r a c t Article history: The Cenozoic growth of the intra-continental Tian Shan Range initiated during the late Eocene–Oligocene, Received 12 April 2018 and led to a tectonic reactivation of the complex Palaeozoic and Mesozoic lithospheric structure. Due to Received in revised form 25 June 2018 the very low erosion rates linked to the semi-arid climate that characterised the Tian Shan region during Accepted 1 July 2018 most of the Cenozoic, the topography of the range is not at equilibrium with deformation. -
The Xinjiang Problem
THE XINJIANG PROBLEM Graham E. Fuller S. Frederick Starr © Central Asia-Caucasus Institute Paul H. Nitze School of Advanced International Studies The Johns Hopkins University Tel.: 1 202 663 7723 [email protected] The Xinjiang Problem 3 Table of Contents Introduction: The Xinjiang Project............................................. 1 I. What is the Problem in Xinjiang? ...........................................4 II. The Geopolitical Realities: a Primer......................................10 III. What Do The Key Players Want? .......................................16 Uyghur Grievances.................................................................................. 16 Uyghur Goals and Actions ........................................................................22 China’s Grievances..................................................................................26 China’s Goals and Actions ........................................................................30 IV. What Is At Stake? Why The Xinjiang Problem Matters ........33 Implications for Ethnic Minorities.............................................................. 33 Uyghurs and the Muslim World.................................................................34 Terrorism .............................................................................................. 40 China and Regional Geopolitics..................................................................43 Human Rights Issues................................................................................47 Economic -

Download Article
Advances in Economics, Business and Management Research, volume 165 Proceedings of the 6th International Conference on Economics, Management, Law and Education (EMLE 2020) Research on the Influences of Tourism on the Process of Local Urbanization in Western Regions Taking Heavenly Pond in Tianshan Scenic Spot of Xinjiang Province as an Example Min Liao1,* Tao Zhang1 1City University of Macau, Macau, China *Corresponding author. Email:[email protected] ABSTRACT In recent years, urbanization research has gradually become a research hotspot in academia, but there are few literatures on the influences of tourism development on urbanization in the western region. By consulting the relevant literature and materials of Heavenly Pond in Tianshan Scenic Spot in Xinjiang and Fukang City, this paper studies the regional and industrial reallocation of resources in Fukang City due to tourism development, the transfer of surplus rural labor force to urban employment, and the changes in space, economy and society based on the current situation of the research area by interview method. The research results show that tourism has a significant impact on population urbanization, economic urbanization, social and cultural urbanization and environmental development in Fukang City. Keywords: tourism, western region, urbanization process, Heavenly Pond in Tianshan Scenic Spot Spot on the urbanization process of Fukang City based I. INTRODUCTION on urbanization theory and stakeholder theory. In the academic circles, there is a general consensus that the development of tourism has a significant role in II. LITERATURE REVIEW promoting the process of local urbanization, which is based on the national level. However, China has a vast A. Research status in foreign countries territory, the economic development of each region is In the early 1970s, the level of urbanization in significantly different, and the development stage of developed countries in Europe and the United States urbanization process is also different. -

Cenozoic Deformation of the Tarim Plate and the Implications for Mountain Building in the Tibetan Plateau and the Tian Shan
TECTONICS, VOL. 21, NO. 6, 1059, doi:10.1029/2001TC001300, 2002 Cenozoic deformation of the Tarim plate and the implications for mountain building in the Tibetan Plateau and the Tian Shan Youqing Yang and Mian Liu Department of Geological Sciences, University of Missouri, Columbia, Missouri, USA Received 11 May 2001; revised 14 March 2002; accepted 8 June 2002; published 17 December 2002. [1] The Tarim basin in NW China developed as a the geology and tectonics of the Himalayan-Tibetan orogen complex foreland basin in the Cenozoic in association [Dewey and Burke, 1973; Molnar and Tapponnier, 1975; with mountain building in the Tibetan Plateau to the Allegre et al., 1984; Armijo et al., 1986; Burchfiel et al., south and the Tian Shan orogen to the north. We 1992; Harrison et al., 1992; Avouac and Tapponnier, 1993; reconstructed the Cenozoic deformation history of the Nelson et al., 1996; England and Molnar, 1997; Larson et Tarim basement by backstripping the sedimentary al., 1999; Yin and Harrison, 2000]. However, some funda- mental questions, such as how stress has propagated across rocks. Two-dimensional and three-dimensional finite the collisional zone and how strain was partitioned between element models are then used to simulate the flexural crustal thickening and lateral extruding of the lithosphere, deformation of the Tarim basement in response to the remain controversial. One end-member model, approximat- sedimentary loads and additional tectonic loads ing the Eurasia continent as a viscous thin sheet indented by associated with overthrusting of the surrounding the rigid Indian plate [e.g., England and McKenzie, 1982; mountain belts. -

Chinese Historian Su Beihai's Manuscript About the History Of
UDC 908 Вестник СПбГУ. Востоковедение и африканистика. 2020. Т. 12. Вып. 4 Chinese Historian Su Beihai’s Manuscript about the History of Kazakh People in Central Asia: Historical and Source Study Analysis* T. Z. Kaiyrken, D. A. Makhat, A. Kadyskyzy L. N. Gumilyov Eurasian National University, 2, ul. Satpayeva, Nur-Sultan, 010008, Kazakhstan For citation: Kaiyrken T. Z., Makhat D. A., Kadyskyzy A. Chinese Historian Su Beihai’s Manuscript about the History of Kazakh People in Central Asia: Historical and Source Study Analysis. Vestnik of Saint Petersburg University. Asian and African Studies, 2020, vol. 12, issue 4, pp. 556–572. https://doi.org/10.21638/spbu13.2020.406 The article analyses the research work of Chinese scientist Su Beihai on Kazakh history, one of the oldest nationalities in Eurasia. This work has been preserved as a manuscript and its main merit is the study of Kazakh history from early times to the present. Moreover, it shows Chinese scientists’ attitude to Kazakh history. Su Beihai’s scientific analysis was writ- ten in the late 1980s in China. At that time, Kazakhstan was not yet an independent country. Su Beihai drew on various works, on his distant expedition materials and demonstrated with facts that Kazakh people living in their modern settlements have a 2,500-year history. Although the book was written in accordance with the principles of Chinese communist historiography, Chinese censorship prevented its publication. Today, Kazakh scientists are approaching the end of their study and translation of Su Beihai’s manuscript. Therefore, the article first analyses the most important and innovative aspects of this work for Kazakh history. -

Major Controls on Streamflow of the Glacierized Urumqi River Basin in the Arid Region of Northwest China
water Article Major Controls on Streamflow of the Glacierized Urumqi River Basin in the Arid Region of Northwest China Muattar Saydi, Guoping Tang and Hong Fang * School of Geography and Planning, Sun Yat-Sen University, Guangzhou 510275, China; [email protected] (M.S.); [email protected] (G.T.) * Correspondence: [email protected] Received: 10 October 2020; Accepted: 27 October 2020; Published: 1 November 2020 Abstract: Understanding the main drivers of runoff availability has important implications for water-limited inland basins, where snow and ice melt provide essential input to the surface runoff. This paper presents an analysis on the runoff response to changes in climatic and other controls of water-energy balance in an inland glacierized basin, the Urumqi River basin, located in the arid region of northwest China, and identifies the major control to which runoff is sensitive across the basin’s heterogeneous subzones. The results indicate that the runoff is more sensitive to change in precipitation in the mountainous headwaters zone of the upper reach, and followed by the impact of basin characteristics. In contrast, the runoff is more sensitive to changes in the basin characteristics in the semiarid and arid zones of the mid and lower reaches. In addition, the change in basin characteristics might be represented by the distinct glacier recession in the mountainous upper reach zone and the increasing human interferences, i.e., changes in land surface condition and population growth, across the mid and lower reach zones. The glacier wasting contributed around 7% on average to the annual runoff between 1960 and 2012, with an augmentation beginning in the mid-1990s. -

Uyghur Religious Freedom and Cultural Values Under Siege
.•.WORLD ♦ ._ It"◊ UNAEPRUltNT'ED UYGHUR • ~ • NATIONS A PEOPU:S rnmmm • • ORGANIZATION I \ HIH 111! \\'- , I< Jlt, 11 )II< I CONGRESS ~ -~ ♦ • • ♦ unpo.(?1'9 Uyghur Religious Freedom and Cultural Values Under Siege 26 February 2018 10:30 am - 12:30 pm Cannon House Office Building Room 121 Washington, DC 20515 U You're invited to join the Uyghur Human Rights Project on February 26th 2018 at 1.0:30 a.m. to 12:30 p.m. in the Cannon House Office Building, Washington, D.t. RSVP here ATEventbrite.com Religious freedom and cultural values are under siege in East Turkestan, the homeland of the Uyghurs. Advanced technologies are being deploye·d against the Uyghurs in the name of security, creating what amounts to the world's most advanced police state, with serious implications for the future of China. and the world. Chinese authorities consider religious diversity a threat to the country's stabili~d, as~: result, implement an autocratic monopoly over freedom of religion. The Uyghurs' language ar@'.cu1tur~} are also being systematically marginalized and actively suppressed by the Chinese government. l:i.oder tti'e" pretense of "antHerrorism", Chinese authorities crackdown ruthlessly on Uyghur communit~ actii~;. East Turkestan, depriving them of their fundamental human rights. Under the pretense of thel1:,culfore and religious practice being a security threat, a security crackdown has intensified in recent moFiths, with more than 1;10,000 of Uyghurs being detained in re-education camps, study abroad students beliig forced_ to return home for political assessment, with widespread political campaigns and militarizatio~reatin~ a climate of fear. -
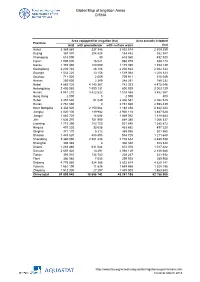
Global Map of Irrigation Areas CHINA
Global Map of Irrigation Areas CHINA Area equipped for irrigation (ha) Area actually irrigated Province total with groundwater with surface water (ha) Anhui 3 369 860 337 346 3 032 514 2 309 259 Beijing 367 870 204 428 163 442 352 387 Chongqing 618 090 30 618 060 432 520 Fujian 1 005 000 16 021 988 979 938 174 Gansu 1 355 480 180 090 1 175 390 1 153 139 Guangdong 2 230 740 28 106 2 202 634 2 042 344 Guangxi 1 532 220 13 156 1 519 064 1 208 323 Guizhou 711 920 2 009 709 911 515 049 Hainan 250 600 2 349 248 251 189 232 Hebei 4 885 720 4 143 367 742 353 4 475 046 Heilongjiang 2 400 060 1 599 131 800 929 2 003 129 Henan 4 941 210 3 422 622 1 518 588 3 862 567 Hong Kong 2 000 0 2 000 800 Hubei 2 457 630 51 049 2 406 581 2 082 525 Hunan 2 761 660 0 2 761 660 2 598 439 Inner Mongolia 3 332 520 2 150 064 1 182 456 2 842 223 Jiangsu 4 020 100 119 982 3 900 118 3 487 628 Jiangxi 1 883 720 14 688 1 869 032 1 818 684 Jilin 1 636 370 751 990 884 380 1 066 337 Liaoning 1 715 390 783 750 931 640 1 385 872 Ningxia 497 220 33 538 463 682 497 220 Qinghai 371 170 5 212 365 958 301 560 Shaanxi 1 443 620 488 895 954 725 1 211 648 Shandong 5 360 090 2 581 448 2 778 642 4 485 538 Shanghai 308 340 0 308 340 308 340 Shanxi 1 283 460 611 084 672 376 1 017 422 Sichuan 2 607 420 13 291 2 594 129 2 140 680 Tianjin 393 010 134 743 258 267 321 932 Tibet 306 980 7 055 299 925 289 908 Xinjiang 4 776 980 924 366 3 852 614 4 629 141 Yunnan 1 561 190 11 635 1 549 555 1 328 186 Zhejiang 1 512 300 27 297 1 485 003 1 463 653 China total 61 899 940 18 658 742 43 241 198 52