Volume 24 Number 1 January 2011
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

4` X ?4A @< Fuuyrg Rd 4>
3 4 768 9 ) 9 9 VRGR '%&((!1#VCEB R BP A"'!#$#1!$"#0$"T utqBVQWBuxy( (01#(!234) 8 567 &$ )69&: 8! 3.<4*4 514''&2N1&13' 8+.'&454 64*1+&235 (*38'(*+('45'. *' 18.4 14.4'<+4 .'&*1.'18+. &*'61<'.* (.'<<4.4' '..'1;48.38'<'46(=.+1'O 64*.'6+ *=64.'('6;1'=5'6' >& &.#/?@((,! #?A >'!)4' % & 5%56378 3) R + ('1 s the talks among the Shiv ASena, the Nationalist Congress Party (NCP) and the Congress over Government formation in Maharashtra remained “inconclusive” on Friday evening, NCP presi- dent Sharad Pawar said that there was “unanimity” among the three parties over Sena president Uddhav Thackeray’s choice as the Chief Minister. Senior leaders of the Congress and the NCP said they have reached “conclusions” on many issues. At the end of a two-hour meeting among the leaders of the Shiv Sena, the NCP and the Congress at the Nehru Centre here, there appeared to be loose ends regarding issues discussed and decisions taken % & - in matters relating to the $ . & * / & , Government formation. The leaders of the three 232'' here on Friday but it was the at five times their original it was a pink carpet welcome parties will meet once again on ing first, Pawar said, “The announcement about the con- anticipating a meeting with famously enthusiastic Kolkata prices, which start from Rs 150. for the invited dignitaries, Saturday to deliberate on the leadership issue settled now. sensus having been reached on the leaders of the three parties t was a party in pink at the fans, who gave the match its Spectators, a lot of them which included the two greats unfinished agenda and decide There is unanimity over his name as the Chief Minister during the weekend. -
Term-1-2017-Newsletter.Pdf
In this Issue Old Boys & Archives Main cover photograph courtesy of Mark Taylor and the Waikato Times ARCHIVES THE LODGE HBHS Back cover photograph courtesy of Hazel Marshall FOUNDATION GOLF We are currently in the process of digitally scanning all the year books TOURNAMENT Welcome to the first edition of the High Achiever, the newsletter that celebrates from 1919 to the present day and putting these on the school server everything excellent at HBHS, for 2017. In this edition we congratulate our Junior as searchable PDFs. They will be accessible to staff and students as March 21st saw 100 Old Boys’ and friends of the school line up and Prize-Winners from 2016 and celebrate the best Scholarship examination results in a resource on the school intranet; a major breakthrough in making tee off at the third annual Foundation Golf Tournament. The top eight our school’s history, along with all of the academic achievements from the end of last our archives accessible to everyone. They can also be individually HBHS student golfers competed for the Foundation Cup and this year year. We check in with our outstanding cultural and sporting performers who have emailed. Each year book can be searched using the ‘Find’ function Tyler Wood took the trophy home. Goldie Rai and the team from already achieved so much before the end of this term. Since our last edition our tally of in Adobe, which makes looking for particular items or names easier. Little India took the top team honours, and for a number of others Regional and National titles and representatives has been added to and then some, and At the time of going to press, over 95 years of Hamiltonians are now golf was the winner on the day. -

12TOIDC COL 17R2.QXD (Page 1)
OID‰‹‰†KOID‰‹‰†OID‰‹‰†MOID‰‹‰†C The Times of India, New Delhi, Friday,September 12, 2003 Berger to say adieu Coria to sit out Fergie’s no to Chelsea Gerhard Berger, motorsport World No. five Guillermo Coria will Man United manager Alex Ferguson director of BMW at present, will not figure in next week’s Davis Cup is reported to have rejected an offer bring down the curtain on his 25 semifinal against Spain. According to take over as Chelsea boss. The years in racing at the Italian Grand to doctors, the top Argentine has United boss insists it would take Prix. The 44-year-old raced in no torn his adductors. Mariano something ‘catastrophic’ to make less than 210 Grand Prix races Zabaleta will be the replacement him leave Old Trafford. France, Sweden Bulgaria, Czech in Euro 2004 AFP Fans have always great to me — David Beckham Seniors in SPORTS DIGEST AFP the dock By Madhu Jawali CHALLENGER TROPHY TIMES NEWS NETWORK off 97 balls and was decorat- Bangalore: If Rohan ed with 13 hits to the fence Gavaskar and S Sriram of In- and one over it. dia ‘A’ had denied the Sourav Dravid and Agarkar, pro- Ganguly-led India Seniors moted to one-drop, com- on Wednesday,Rahul Dravid pounded the Seniors’ situa- and Co (India ‘B’) made them tion. The duo authored the miserable on Thursday. most productive partnership Leading the assault was cap- of the innings, 136 runs off tain Dravid himself, who 125 balls, which paved the carved a brilliant century. A way for a huge total. -

College Admission Result
BOARD OF INTERMEDIATE AND SECONDARY EDUCATION, DHAKA List of Students of HSC Admission (Session 2014-2015) COLLEGE/THANA/ZILLA (EIIN): BIRSHRESHTHA NOOR MOHAMMAD PUBLIC COLLEGE/LALBAG/DHAKA MAHANAGARI (108161) SHIFT: DAY (BANGLA) EXPECTED GROUP: SCIENCE SL NO ROLL NO SSC PASS BOARD SSC PASS YEAR NAME GPA SELECTION STATUS APPLIED QUOTA 00001 100198 RAJSHAHI 2014 TASNEEM AHMED 5.00 Merit 00002 100290 RAJSHAHI 2014 MD. MAHMUDUL HASSAN 5.00 Merit 00003 100302 DHAKA 2014 MD. MOINUL ISLAM KHAN 5.00 Merit 00004 101948 DHAKA 2014 MD. HASAN HAWLADER 5.00 Merit 00005 102535 JESSORE 2014 ANKON GHOSH ARGHO 5.00 Merit 00006 103206 DHAKA 2014 S.H.M. MUNTASIR RAHI 5.00 Merit-OWN 00007 103207 DHAKA 2014 S M FAHIM SHAHRIAR 5.00 Merit-OWN 00008 103208 DHAKA 2014 RAJAT CHAKRABORTY 5.00 Merit-OWN 00009 103209 DHAKA 2014 KAZI FAKHRUL ABEDIN 5.00 Merit-OWN 00010 103210 DHAKA 2014 MOHAIMENUL HASAN 5.00 Merit-OWN 00011 103211 DHAKA 2014 A.B.M. SHAMSUL BARI 5.00 Merit-OWN 00012 103212 DHAKA 2014 MAHIR ASHRAF 5.00 Merit-OWN 00013 103213 DHAKA 2014 MD. HASIBUL HASAN 5.00 Merit-OWN 00014 103214 DHAKA 2014 HASIBUL HOSSAIN 5.00 Merit-OWN 00015 103215 DHAKA 2014 SHAMIM AL MUSTAFIZ 5.00 Merit-OWN EQ 00016 103216 DHAKA 2014 MD. SHAKIBUL HASAN 5.00 Merit-OWN 00017 103217 DHAKA 2014 NAFIZ IMTIAZ KHAN 5.00 Merit-OWN 00018 103218 DHAKA 2014 MAHAMUDUL HASAN ASHIK 5.00 Merit-OWN 00019 103220 DHAKA 2014 FERDAOUS RASHID RAYEED 5.00 Merit-OWN 00020 103221 DHAKA 2014 MD. -

Tony Payne for Organising the Match and Tony for Co-Ordinating the Draw and Filling in for Me When I Had to Leave Early
1 PARKFIELD PRESS 2012-13 December Edition 2 Welcome to the Parkfield Press Welcome to the Parkfield Press, the publication that will keep Parkfield cricketers up to date with everything that is happening down at Dunblane Road this season. The Parkfield Press would like to present the opportunity for its readers to get involved. If you have any anecdotes, funny stories, pictures, photos or any other suggestions, please either put them in the Parkfield Press Box located at Dom’s Bar, Parkfield or email the editor at [email protected] Also check out the Parkfield website for regular updates including Teams, Poker and Fantasy Results and Event Info: http://parkfield.vic.cricket.com.au/ December Edition Contents Page 3: Parkfield Social Calender Page 34: Parkfield Funnies Page 4: The Prez’s Piece Page 35: Parkfield Congratulates Page 6: Player Profile Page 36: Parkfield Poker Page 8: Senior Report Page 40: Parkfield Fantasy League Page 18: Junior Report Page 42: Parkfield Greyhounds Page 20: Player Profile Page 44: Quizmaster Page 22: Pictures of Parkfield Page 46: Parkfield Sponsors Page 24: The Faz Files Page 48: Parkfield Contact Numbers Page 26: Player Profile Page 50: Parkfield Merchandise Page 29: Cooking With Bob Page 51: Quizmaster Competition Page 30: Parkfield’s Past Page 53: Parkfield Membership Fees 3 Parkfield Social Calender 2012/13 DECEMBER Sat Dec 15th, Round 6, Week 1. Sun Dec 16th. Round 1 rescheduled. TURF 1 @ Mordialloc, TURF 4 @ home. Tuesday Dec 18th. RAFFLE TICKETS & MONEY MUST BE RETURNED PLEASE, See Bek/Dags/Couttsy Committee meeting after training Sat Dec 22nd Round 6, 2nd week Raffle Drawn DDCA Radio show. -

Annual Report 2007 Chief Editor Alejandro Cravioto
"//6"-3&1035 KNOWLEDGE FOR GLOBAL LIFESAVING SOLUTIONS ICDDR,B www.icddrb.org annual report 2007 Chief Editor Alejandro Cravioto Managing Editor Jo Grzelinska Editors Henry Richards Peter Thorpe Design & Layout Syed Hasibul Hasan Photographs © ICDDR,B © ICDDR,B/Bitu/MAP, pages 7, 9, 10, 14, 15, 19, 22, 23, 24, 32, 33, 35, 42, 43, 44, 45, 57, 58, 64, 74, 88, 91, 97 © 2006 Aniela Batschari, Courtesy of Photoshare, page 76 © 2005 Virginia Lamprecht, Courtesy of Photoshare, page 77 © 2004 Peter de Lisle, Courtesy of Photoshare, page 78 © 2002 Joanna Sekula, Courtesy of Photoshare, page 78 Printer Print Link Printers © 2008 International Centre for Diarrhoeal Disease Research, Bangladesh June 2008 ISBN 978 984 551 294 7 ICDDR,B (International Centre for Diarrhoeal Disease Research, Bangladesh) GPO Box 128 Dhaka 1000 Bangladesh Phone: (880-2) 8860523-32, 8822467 Fax: (880-2) 8819133, 8823116 [email protected] www.icddrb.org ICDDR,B is committed to ethical development photography and obtained permission from photo subjects in this report whenever reasonable and practical Vision www.icddrb.org All people, especially the poor, can become healthier and can reach their full potential through the application of new knowledge Mission To develop and promote realistic solutions to the major health, population and nutrition problems facing the poor people of Bangladesh and other settings Guiding Values Excellence in research, training and service High ethical standards Gender equality Responsive to change Promote partnerships Prioritizes the needs -
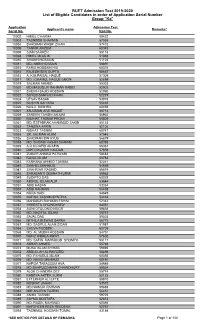
BUET Admission Test 2019-2020 List of Eligible Candidates in Order of Application Serial Number Group "Ka"
BUET Admission Test 2019-2020 List of Eligible Candidates in order of Application Serial Number Group "Ka" Application Admission Test Applicant's name Remarks* Serial No. Roll No. 10002 HIMEL CHAKMA 58422 10003 TASNEEM SHARMIN 57058 10004 SHADMAN WASIF ZIHAN 57418 10005 TANVIR ANZUM 60345 10006 SIAM SARKER 58116 10008 HIMEL MOULIK 51088 10010 SHAIKH HOSSAIN 51124 10011 MD. AMIN HOSSAIN 58891 10012 FARIA HOSSAIN HIA 60374 10014 RAJESH SEN GUPTA 50667 10015 A. K.M.FAISAL HAQUE 57309 10017 MD. IQRAMUL HAQUE EMON 52899 10018 SALMAN AHMED 55303 10020 MD.MASUDUR RAHMAN RABBI 52902 10021 SHEIKH SAJID HOSSAIN 52080 10022 SOYEB SANIYAD KHAN 52279 10024 UTSAV BASAK 53978 10025 NOSHIN SAIYARA 55465 10026 NAILA BUSHRA 60493 10027 ANJUMAN ARA HAQUE 50713 10029 ZAREEN TAHSIN ANJUM 56932 10030 NUZHAT TASNIM PROMI 55809 10031 MD. ESTABRAK AHAMMOD SAKIB 50153 10032 TANZINA AFRIN 52106 10033 NISHAT TASNIM 60747 10035 SK. SALMAN ALAM 57545 10036 SHADMAN BIN AYUB 56879 10038 MD. SHOAIB HASAN SHAMIM 60393 10039 A.R.M RAFID ARAFIN 56387 10040 DIPTO KUMAR HALDAR 57059 10041 ZUBAIR AHMAD PATWARI 58483 10042 RAISA ISLAM 50783 10043 FARHANA AHMED TONIMA 52241 10045 SHAHEL MAHMUD 54659 10047 SHAHRIAR RASHID 56619 10048 SHRABANTI DEBNATH URMI 59983 10049 SUDIPTO DAS 60028 10050 AMIRUL ISLAM ALIF 53644 10051 ABID HASAN 53354 10053 ASIB RAHMAN 54438 10054 NURA HADI 54649 10055 NAFISA TASNIM SYNTHIA 54432 10056 MAHABUR RAHMAN FAHIM 52342 10057 SHRESTA CHOWDHURY 54561 10058 AGNI OTULONIO NOOR 59858 10062 MD. NAZIFUL ISLAM 55747 10065 SAJAL DAS 59525 10066 MITHILA BISWAS SARNA 56772 10067 MD. SADRUL ALAM ZIDAN 51987 10068 SHUVA PODDER 60709 10069 MD. -

College Admission Result
BOARD OF INTERMEDIATE AND SECONDARY EDUCATION, DHAKA List of Students of HSC Admission (Session 2013-2014) COLLEGE/THANA/ZILLA (EIIN): RAJUK UTTARA MODEL COLLEGE/UTTARA/DHAKA MAHANAGARI (108573) SHIFT: DAY (BANGLA) EXPECTED GROUP: SCIENCE SL NO ROLL NO SSC PASS BOARD SSC PASS YEAR NAME GPA SELECTION STATUS APPLIED QUOTA 00001 100110 SYLHET 2013 MD. TAUFIQUE SHAWON 5.00 Merit 00002 100147 RAJSHAHI 2013 TAHMIDUR RAHMAN 5.00 Merit-FQ FQ 00003 100166 RAJSHAHI 2013 AHNAF FAISAL 5.00 Merit 00004 100215 RAJSHAHI 2013 MD. NAIEM MOSADDEK MRIDUL 5.00 Merit 00005 100263 RAJSHAHI 2013 NURUZZAMAN 5.00 Merit 00006 100332 RAJSHAHI 2013 ROKEYA HAIDER 5.00 Merit 00007 100333 SYLHET 2013 AKIB IRFAN 5.00 Merit 00008 100405 RAJSHAHI 2013 SEJUTI SHABIN 5.00 Merit 00009 100467 RAJSHAHI 2013 NAZIA MUSTARY NAYNA 5.00 Merit 00010 100920 SYLHET 2013 SATYAKI BANIK 5.00 Merit-FQ FQ 00011 100992 RAJSHAHI 2013 TASNIM AHMED 5.00 Merit 00012 101371 RAJSHAHI 2013 HUMAIRA RAFI ZINNURAIN 5.00 Merit 00013 101427 SYLHET 2013 SUMAIA JAHAN MISHU 5.00 Merit 00014 101587 CHITTAGONG 2013 NUSHRAT AFRIN SHITHIL 5.00 Merit 00015 101621 CHITTAGONG 2013 MOHAMMAD TARIQUR RAHMAN 5.00 Merit 00016 101890 CHITTAGONG 2013 RAIHAN KABIR 5.00 Merit 00017 101898 CHITTAGONG 2013 MAHFUJUR RAHMAN SHAHIN 5.00 Merit 00018 101950 CHITTAGONG 2013 ANUPAM DEBASHIS ROY 5.00 Merit 00019 101951 CHITTAGONG 2013 IMTIAZ HASAN CHAYON 5.00 Merit 00020 101952 CHITTAGONG 2013 ASHIQUE-E-ELAHI 5.00 Merit 00021 101956 CHITTAGONG 2013 KAZI MD. JAHIDUL HASAN 5.00 Merit 00022 101972 CHITTAGONG 2013 MOHI MENUL MONTASER 5.00 Merit 00023 102014 CHITTAGONG 2013 MD. -
Bsc-List-2021.Pdf
Serial NO USER ID APPLICANT NAME FATHER NAME MOTHER NAME SSC ROLL SSC GPA HSC ROLL HSC GPA STATUS PROGRAM 1 PROGRAM 2 1 BWLBIAR ABDUL KARIM ABDUL JALIL ASRAFUN NAHAR PANNA 151941 5.00 135304 5.00 ELIGIBLE Avionics Aerospace 2 BCKZIWW MD. SADEKUZZAMAN NISHAT MD. NURUL ISLAM MOST. SAFURA BEGUM 197415 5.00 133445 5.00 ELIGIBLE Aerospace Avionics 3 BOZTVVP SYED JISAN KABIR SYED HUMAUN KABIR MST. SOHELA PARVIN 122848 4.78 117454 5.00 ELIGIBLE Aerospace Avionics 4 BTOYUFQ JUBAER AL- AMIN EMON MD. NURUL AMIN KHADIZA BEGUM 112310 5.00 134312 5.00 ELIGIBLE Aerospace Avionics 5 BQEEWWA KHONDOKER AMIMUL AHASAN KHONDOKER SHAHJAHAN HAIDER MOHUA AKTER RUMI 113572 5.00 126831 5.00 ELIGIBLE Aerospace Avionics 6 BAXLYGI NAZYA MUSTAFIZ MD. HASAN MUSTAFIZ MST. JEBUN NAHAR 132195 5.00 115611 5.00 ELIGIBLE Avionics Aerospace 7 BAHFMZO NOOR-E-TAOHEED ALAMIN NOOR-E-KHAJA ALAMIN SABRINA QUADIR 106558 4.94 144405 5.00 ELIGIBLE Aerospace Avionics 8 BKALAXP FAHMIDA YASMIN NISHI MD. RAFIQUL ISLAM MOSD. ROWSHAN ARA 116688 5.00 108880 4.50 ELIGIBLE Aerospace Avionics 9 BBQMHFL SAYERIN NURESHA ORTHI MD. JAHANGIR ALAM SABINA YASMIN 229105 5.00 120540 5.00 ELIGIBLE Avionics Aerospace 10 BSGBVMD AL IMRAN JAHID HASAN MD. DULAL UDDIN MOST. ZOLEKHA BEGUM 181532 5.00 607569 5.00 ELIGIBLE Aerospace Avionics 11 BYXRDVN TITHY RANI DAS MANILAL DAS RADHA RANI DAS 108244 5.00 105730 5.00 ELIGIBLE Aerospace Avionics 12 BOXPDSY MD. AWAL HADI MD. A. HAMID MST. ANJUARA BEGUM 134159 4.89 102828 5.00 ELIGIBLE Aerospace Avionics 13 BJNCFYD NOSHIN NAWAR MOHAMMAD SHAHJAHAN FARZANA MAINUDDIN 116353 5.00 100538 5.00 ELIGIBLE Avionics Aerospace 14 BAXBRUP MD RAFIUL ISLAM MD AMINUL ISLAM MST. -

Annual Report Annual
ANNUAL REPORT ANNUAL ANNUAL REPORT 2009 2009 ICDDR,B www.icddrb.org g r .o b (880-2) 8819133 (880-2) 8823116 (880-2) 8822467 GPO Box 128 Dhaka 1000 Bangladesh director@icddr Fax Phone (880-2) 8860523-32 ICDDR,B ICDDR,B annual report 2009 www.icddrb.org Board of Trustees www.icddrb.org Chairperson Dr Timothy G Evans, WHO Member-Secretary (ex-officio) Dr Alejandro Cravioto Executive Director, ICDDR,B Members Dr Mohammad Jalal Abbasi-Shavazi, Iran Mr Shaikh Altaf Ali, Bangladesh Mr M Musharraf Hossain Bhuiyan, Bangladesh Dr Thomas Cheasty, United Kingdom Prof AHM Towhidul Anowar Chowdhury, Bangladesh Datuk Dr Raj Bte Abdul Karim, Malaysia Dr Mary Ann D Lansang, Philippines Dr Ann Larson, Australia Dr Nicolaus Lorenz, Switzerland Dr Halima Abdullah Mwenesi, South Africa (left in June 2009) Dr José Ignacio Santos Preciado, México Mr Carel de Rooy, UNICEF Bangladesh Dr Suttilak Smitasiri, Thailand (left in June 2009) Dr Peter Tugwell, Canada Dr Haruo Watanabe, Japan (left in June 2009) Dr Mary Elizabeth Wilson, USA (since July 2009) Prof Charles Stephen Mgone, Tanzania (since July 2009) Dr Norma Binsztein, Argentina (since July 2009) Chief Editor Contributing Writer Photographs Alejandro Cravioto Sumona Liza © ICDDR,B Cover/Dr Jasim Uddin Managing Editor Design & Layout 6/Md Huzzatul Mursalin Jo Grzelinska Syed Hasibul Hasan 14, 17, 20, 82, 101, 111/Bitu/Map Mohammad Inamul Shahriar 33/Leah Sanderson 34/Dr Peter Kim Streatfield 79/Md Mahbubul Islam Bhuiyan 95/CDC/Dr WA Clark (PHIL #1617), 1977 89/www.lumaxart.com The full report is available -

HC Clears TSRTC Privatisation L VENKAT RAM REDDY
Follow us on: RNI No. TELENG/2018/76469 @TheDailyPioneer facebook.com/dailypioneer Established 1864 Published From ANALYSIS 7 MONEY 8 SPORTS 12 HYDERABAD DELHI LUCKNOW TOO LITTLE AND A GOVT RELIEF MAY NOT ISHANT BHOPAL RAIPUR CHANDIGARH LITTLE TOO LATE SAVE TELCOS IN PINK MODE BHUBANESWAR RANCHI DEHRADUN VIJAYAWADA *LATE CITY VOL. 2 ISSUE 44 HYDERABAD, SATURDAY NOVEMBER 23, 2019; PAGES 12 `3 *Air Surcharge Extra if Applicable POOR SCREENPLAY, DRY ACTING MAKE GEORGE REDDY A DULL WATCH { Page 11 } www.dailypioneer.com Maha mayoral polls Sena-Cong- HC clears TSRTC privatisation Axe hangs over 50% jobs in TSRTC NCP combine L VENKAT RAM REDDY PNS n HYDERABAD Dismisses PIL opposing privatization of 5,100 routes n HYDERABAD outsmart BJP In a massive relief to the state With the High Court PNS n MUMBAI government, a division bench The CS Dr SK Joshi upholding the decision of of the Telangana High Court the Telangana state govern- The BJP was outsmarted on on Friday dismissed the Public stated that the cabinet ment to privatise 50 per Friday by emerging political Interest Litigation (PIL) plea decision taken on Nov 2 cent of RTC bus routes on combinations in Maharashtra filed by the vice president of to give permits to 5,100 Friday, there is an air of and lost mayoral polls in Telangana Jana Samithi (TJS) pvt bus operators per se uncertainty over the future Latur and Ulhasnagar despite Prof PL Vishweshwar Rao chal- of 48,000-strong employees having a majority in both lenging the decision of the state might not be open to who have been on strike till civic bodies. -

MARINE CADET ADMISSION TEST Total Passed : 1728
Department of Shipping MARINE CADET ADMISSION TEST Admission Session : 2020-2021 Passed Candidate List Total Passed : 1728 # Roll No Full Name 1 0001 SAIDUL ISLAM 2 0002 ABDULLAH AL MREENMAY 3 0006 ARAFATH EASIN 4 0009 MD. NAHIYAN INAM 5 0010 TAFSIR HOSSIN PARTHO 6 0012 KAZI AFRAIM AHMED 7 0013 MD. ARIFUR RAHMAN 8 0014 MAHBUBA HAQUE AYSHA 9 0015 MD. IMAM HASAN 10 0016 REAJUL ISLAM RATUL 11 0017 GAZI SAZZAD HOSSAIN 12 0018 ABDULLAH-AL-SHABAB 13 0019 RANA ROY 14 0020 MD. MUSFIKUR RAHMAN 15 0021 REYZUL ISLAM RIFAT 16 0022 MD. MANNAFI MOLLAH 17 0023 MD. MEHEDI HASAN 18 0024 MD. MEHEDI HASAN RAKIB 19 0027 MD. RASHIDUL ISLAM 20 0030 MD. SABBER SALEHIN 21 0031 HIJBULLAH HUMAYON CHOWDHURY 22 0032 SIAM AHMED 23 0033 ORIQUL ISLAM OYON 24 0035 SAMIUL ISLAM SOURAV 25 0036 RAIYAN TAMIM 26 0040 MD. MEHADI HASAN MAZUMDAR SHAHIN 27 0042 MAHFUZUR RAHMAN 28 0043 MD.METHUN ALI 29 0047 MD. JANNATUL NAYEM 30 0048 SANID HASAN 31 0049 TANVIR MAHTAB SADMAN 32 0051 ABU BAKAR SIDDIQUE MAHI N.B: Instructions for Physical ,orals, medical and eye sight test will be informed soon. # Roll No Full Name 33 0052 GOLAM SHAHRIAR MAHMUD 34 0055 MAMUNUR ROSHID 35 0056 MD. FAHIM IMTIAZ 36 0058 TANZID MORSHED 37 0059 SAEED SARWAR ANAS 38 0064 AHASON HABIBUR RAHMAN 39 0066 MD. SHAHRIAR JAHAN 40 0068 RAHAMATULLA SHOHAN 41 0070 OMAR HASAN JABED 42 0071 MD. AHASAN HABIB SABBIR 43 0072 MIZANUR RAHMAN SOGIB 44 0076 SHAHAREAR HOSSAIN SADUN 45 0077 EMAM HOSSAIN 46 0078 MD.