Field Project Reports
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Demand No : 7 - Police I
DEMAND NO : 7 - POLICE I. Estimates of the amount required for the year ending 31st March, 2021 to defray expenses in connection with POLICE (₹ in lakhs) Revised Estimates, 2019 - 20 Budget Estimates, 2020 - 21 Revenue Others Total Revenue Others Total Voted : 188797.52 2695.93 191493.45 231499.02 2696.93 234195.95 Charged : ... ... ... ... ... ... Grand Total : 188797.52 2695.93 191493.45 231499.02 2696.93 234195.95 II. The Heads under which this Grant/Appropriation is to be accounted for: (₹ in lakhs) Category of Actuals Budget Estimates Revised Estimates, 2019 - 20 Budget Estimates, 2020 - 21 Heads Code 2018 - 19 2019 - 20 Hill Valley Total Hill Valley Total Major Head 2055 Police Sub-Major 00 Minor 001 Direction and Administration Sub-Head 01 Direction Detailed 00 Object 01 Salaries 1276.66 ... 1102.20 1102.20 ... 1432.86 1432.86 05 Rewards 20.00 ... 20.00 20.00 ... 20.00 20.00 11 Domestic travel expenses 10.00 ... 25.00 25.00 ... 25.00 25.00 13 Office Expenses 15.00 ... 60.00 60.00 ... 60.00 60.00 24 P.O.L. 3334.78 ... 3584.78 3584.78 ... 3634.78 3634.78 28 Professional Services 40.00 ... 40.00 40.00 ... 40.00 40.00 41 Secret Service Expenditure 150.00 ... 150.00 150.00 ... 150.00 150.00 50 Other charges 20.00 ... 79.40 79.40 ... 79.40 79.40 Detailed 01 Election Expenses Object 50 Other charges 3000.00 ... 3000.00 3000.00 ... 10.00 10.00 Total : Election Expenses 3000.00 ... 3000.00 3000.00 ... 10.00 10.00 Detailed 02 Games and Sports Object 50 Other charges 0.70 .. -
Table of Contents Executive Summary
EIA Studies for Exploratory drilling at Pre-NELP Block AA-ONJ/2 DRAFT EIA/EMP REPORT M/s Oil and Natural Gas Corporation Ltd. EIA Studies for Pre-NELP Block AA- ONJ/2 (for Drilling 9 Exploratory Wells) For on and behalf of SENES Consultants India Ltd Approved by Mr. Salil Das Signed by Position held NABET-QCI Accredited EIA Coordinator for Offshore & Onshore Oil and Gas Exploration Development and Production Date December 10, 2013 The EIA report preparation have been undertaken in compliance with approved ToR issued by the MoEF vide letter no. J11011/91/2012-IAII (I) dated 13th July, 2012. Information and content provided in the report is factually correct for the purpose and objective of the study . SENES/K-20200/December 2013 b ONGC EIA Studies for Exploratory drilling at Pre-NELP Block AA-ONJ/2 Abbreviation ALARP As Low As Reasonably Practicable BOD Biological Oxygen Demand BOP Blow out Preventor Block Khoraghat Extension ML Block Cd Cadmium CGWB Central Ground Water Board COD Chemical Oxygen Demand CPCB Central Pollution Control Board Cr Chromium CSR Corporate Social Responsibility Cu Copper DG Diesel Generator DGH Directorate General of Hydrocarbons DMP Disaster Management Plan DO Dissolved Oxygen EC Environmental Clearance EIA Environmental Impact Assessment EMP Environment Management Plan ETP Effluent Treatment Plant FC Forest Clearance GGS Group Gathering Station GLC Ground Level Concentrations GoI Government of India HC Hydrocarbon HDPE High Density Polyethylene HSD High Speed Diesel HSE Health, Safety and Environmental IMD Indian -

Economic Survey, Manipur, 2016-17
P R E F A C E The ‘Economic Survey, Manipur, 2016-17’ presents a broad analysis of the latest economic situation of the state based on performance appraisal data collected from various sources. It is the 21st issue of the series. The salient feature of the State’s economy is briefly discussed in Part-I and supporting statistical tables are presented in Part-II. Some of the chapters/tables have been modified in the present issue on the basis of the data-base made available by the different Agencies/Departments. The district level data presented herein relates to the 9 (Nine) Districts which existed before the creation of the new 7 (Seven) Districts in December, 2016. Certain information are depicted in the form of charts. It is hoped that with the active co-operation of different Organisations/Departments, the Directorate will be able to make improvements in the quality and contents of the publication in its future issues. The co-operation and help extended spontaneously by different Departments of the Government, local bodies and private institutions are gratefully acknowledged. I also appreciate all the officers and staff of the Economic Analysis (EA) and Coordination and Publications (CoP) Units of the Directorate for their untiring efforts put in for preparation of the current issue of the publication. The co- operation extended by the Printing Unit of the Directorate in printing and binding of the publication is also gratefully acknowledged. The contributions of the Graphics Section in designing cover are also acknowledged with thanks. I hope that this publication will prove to be useful to the planners, policy makers, social workers and researcher and will help in enhancing their understanding on the socio- economic scenario of Manipur State. -

The Complexities of Tribal Land Rights and Conflict in Manipur: Issues and Recommendations 2
Issue Brief – June 2017 Vol: VIII Vivekananda International Foundation Brigadier Sushil Kumar Sharma The Complexities of Tribal Land Rights and Conflict in Manipur: Issues and Recommendations 2 About the Author Brigadier Sushil Kumar Sharma, YSM, commanded a Brigade in Manipur and served as the Deputy General Officer Commanding of a Mountain Division in Assam. He has been conferred with a PhD, for his study on North-East India. He is presently posted as Deputy Inspector General of Police, Central Reserve Police Force in Delhi. http://www.vifindia.org © Vivekananda International Foundation The Complexities of Tribal Land Rights and Conflict in Manipur: Issues and Recommendations 3 The Complexities of Tribal Land Rights and Conflict in Manipur: Issues and Recommendations Abstract Land is at the center of most conflicts in Northeast India because of its importance in the life of the people of the region, particularly its tribal communities. Manipur, the Land of Jewels, has been besieged with conflicts on issues ranging from exclusivity, integration and governance. All these have stemmed from the basic dispute over the land. The tribal people of the hills and the valley based people have different approaches and laws towards governance of their land which they consider their exclusive territories. This study attempts to track the issues concerning the land rights of various people in the state and the ethnic conflict surrounding it and attempts to identify land issues that are leading to ethnic conflict in Manipur and tries to address the issue of conflict and make suggestions thereof. Introduction The Study Over the landscape of the history of mankind that we know, since times which have been chronicled there has always been conflict amongst human beings to possess, cherish and control land. -

Details of 701 Functional One Stop Centres(Oscs)
FUNCTIONAL ONE STOP CENTRES Summary Sheet Sr. No. Name of State / UT Number of OSCs Functional 1. Andaman and Nicobar (UT) 03 2. Andhra Pradesh 13 3. Arunachal Pradesh 24 4. Assam 33 5. Bihar 38 6. Chandigarh (UT) 01 7. Chhattisgarh 27 8. Dadra and Nagar Haveli and 02 Daman & Diu (UT) 9. Delhi (UT) 11 10. Goa 02 11. Gujrat 33 12. Haryana 22 13. Himachal Pradesh 12 14. Jammu & Kashmir (UT) 18 15. Jharkhand 24 16. Karnataka 30 17. Kerala 14 18. Lakshadweep (UT) 01 19. Ladakh (UT) 01 20. Maharashtra 37 21. Madhya Pradesh 52 22. Manipur 16 23. Meghalaya 11 24. Mizoram 08 25. Nagaland 11 26. Odisha 31 27. Punjab 22 28. Puducherry (UT) 04 29. Rajasthan 33 30. Sikkim 04 31. Tamil Nadu 34 32. Telangana 33 33. Tripura 08 34. Uttar Pradesh 75 35. Uttarakhand 13 36. West Bengal 00 Total 701 One Stop Centre Details SI. NO District OSC Address Concerned CA OSC Phone Mail ID Number Andaman and Nicobar (UT) 1. South Andaman SAKHI One Stop Centre Ms. Reeta Devi 8900909396 [email protected] Near AYUSH Hospital, Type V, Quarter No:JG-6, Junglighat Port Blair, A&N Islands Pin Code 744103 2. North & Middle SAKHI One Stop Centre Mrs.Shvatha Priya 9940169132 [email protected] Andaman Old Zonal Library Maybunder North & Middle Andaman 3. Car Nicobar SAKHI One Stop Centre Mrs.Zareena Bibi 9434269836 [email protected] Perka Head Quarter Nicobar Car Nicobar Andhra Pradesh 4. East Godavari Disha (Sakhi) One Stop Sailaja Ranganadham . 9493270181/ [email protected]. -

Environmental Awareness Among the School Geography Teachers in Manipur
Journal of Interdisciplinary Cycle Research ISSN NO: 0022-1945 ENVIRONMENTAL AWARENESS AMONG THE SCHOOL GEOGRAPHY TEACHERS IN MANIPUR: A CASE OF IMPHAL EAST DISTRICT By: Dr Chirom Shantikumar Singh Assistant Professor, DM College of Teacher Education Email ID: [email protected] ABSTRACT Although environment has a great importance in modern times, yet environmental education has not been given due importance in our school education. Hence the present study is designed to assess the attitudes of geography teachers in Imphal East District, Manipur towards the environment change according to different variables, using ‘’Attitude Scale” for 240 geography teachers working in various high schools. The result revealed that the environmental attitudes of the geography teachers in the district are very high. It is also indicated that no significant differences among non-geographer geography teacher and geography teacher with geography at the graduation; and between male and female geography teachers towards environmental awareness. 1.1 Key Terms Used: Environment, Environmental education, Environmental awareness, Geography, and Pollution. 1.2 Introduction: the Study Area: Imphal East district lies between latitudes 24º39′49.09′′N and 25º4′5.45′′ N and longitudes 93º55′30′′ E and 94º8′42′′ E approximately and is one of the 16 districts of Manipur. It came into being with effect from 30th August, 1996 by bifurcating the erstwhile Imphal district into two districts namely Imphal East District and Imphal West District with its head quarters at Porompat. The district is bounded by Senapati district on the north and east; Thoubal district on the south and Imphal west district on the west. -
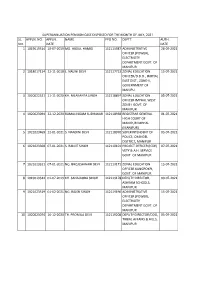
Sl. No. Appln. No. Appln. Date Name Ppo No. Deptt
SUPERANNUATION PENSION CASE DISPOSED FOR THE MONTH OF JULY, 2021 SL. APPLN. NO. APPLN. NAME PPO NO. DEPTT. AUTH. NO. DATE DATE 1 1019019514 10-07-2019 MD. ABDUL HAMID 112115987 ADMINISTRATIVE 28-07-2021 OFFICER (POWER), ELECTRICITY DEPARTMENT GOVT. OF MANIPUR 2 1018017114 22-11-2018 L. NALINI DEVI 112117713 ZONAL EDUCATION 15-07-2021 OFFICER/D.D.O., IMPHAL EAST DIST., ZONE-II, GOVERNMENT OF MANIPU 3 1020022521 11-11-2020 KH. NILAKANTA SINGH 112118897 ZONAL EDUCATION 05-07-2021 OFFICER IMPHAL WEST ZONE-I GOVT. OF MANIPUR 4 1020023094 22-12-2020 RAMALINGAM SUDHAKAR 112118938 REGISTRAR GENERAL 01-07-2021 . HIGH COURT OF MANIPUR IMPHAL (MANIPUR) 5 1021023469 12-01-2021 S. NANDINI DEVI 112118970 SUPERINTENDENT OF 05-07-2021 POLICE, CHANDEL DISTRICT, MANIPUR 6 1021023308 07-01-2021 S. RANJIT SINGH 112119101 PROJECT OFFICER (ICDP) 07-07-2021 VETY & A.H. SERVICE GOVT. OF MANIPUR 7 1021023321 07-01-2021 NG. BROJESHWARI DEVI 112119171 ZONAL EDUCATION 15-07-2021 OFFICER KANGPOKPI, GOVT. OF MANIPUR 8 1019019344 01-07-2019 KH. SANAJAOBA SINGH 112119178 DEPUTY DIRECTOR, 09-07-2021 ASHRAM SCHOOLS, MANIPUR 9 1021023519 01-02-2021 NG. RAJEN SINGH 112119196 ADMINISTRATIVE 15-07-2021 OFFICER (POWER), ELECTRICITY DEPARTMENT GOVT. OF MANIPUR 10 1020023074 16-12-2020 TH. PROMILA DEVI 112119208 DEPUTY DIRECTOR/DDO, 05-07-2021 TRIBAL AFFAIRS & HILLS, MANIPUR 11 1020022843 08-12-2020 K. SWARNALATA DEVI 112119212 DY. DIRECTOR 01-07-2021 (HC)/DDO/HOO DIRECTORATE OF HANDLOOM & TEXTILES, GOVT. OF MANIPUR 12 1020022606 25-11-2020 S. KHAMBA SINGH 112119236 COMMANDANT 11TH 13-07-2021 BN. -

Paper Teplate
Volume-04 ISSN: 2455-3085 (Online) Issue-03 RESEARCH REVIEW International Journal of Multidisciplinary March-2019 www.rrjournals.com[UGC Listed Journal] Land Rights and Conflict in Manipur: A Critical Analysis Ngaranngam Keishing PhD Scholar, School of Development Studies, Ambedkar University Delhi (India) ARTICLE DETAILS ABSTRACT Article History For many years, Manipur has been in the throes of ethnic conflicts and violence. All these Published Online: 13 March 2019 ethnic conflicts in one way or another related to disputes over land and resources. The hill areas- mainly dominated by the tribal communities and the valley areas- mostly dominated Keywords by the non-tribal have distinct land use and management systems. Each system has its own Manipur, Ethnic conflicts, Tribal, Land enforcement mechanism as well as codification of rules and norms. This diversity in Alienation, Autonomy property rights is considered by many social scientists as the main cause of conflict among different ethnic communities in the state. Ethnic conflicts in the state are not only rooted on *Corresponding Author Email: ngaranngamk437[at]gmail.com the existing differences in land use and management between the hill and valley areas, but it is also a fall out of the systematic political manipulation by the politically dominant valley people to alienate tribals‟ land. 1. Introduction According to Sharma (2001), the history of India post Manipur, which is inhabited by different ethnic groups, has independence is full with examples of exploitation, deprivation witnessed severe turmoil and ethnic conflicts1 over the decade and marginalization of the tribal communities especially in the or so. All these ethnic conflicts in one way or another are form of land alienation. -
Sunday, August 15, 2021, Imphal in the SUPREME
Sunday, August 15, 2021, Imphal 8 H U E I Y E N LANPAO Delivery Mode: Registered MR. CHANDAN KUMAR (ADV.) FOR R[64] 105 RAJKUMARI SANJUKTA W/O ARVIND SOUGAIJAM, PID: 85150/2021 FOR R[105] IN WA NO 20-A LAWYERS CHAMBER SUPREME COURT OF INIDA, DISTRICT- NEW DELHI, DELHI R/O. SINGJAMEI MATHAK THOKCHOM LEIKAI, P.O. AND P.S. - 19/2017 AND R[106] IN RP NO. 3 65 SHENYAI LEIMA ANGOM D/O NARAYAN ANGOM, BRAHMAPUR PID: 85110/2021 FOR R[65] IN WA NO SINGJAMEI, IMPHAL WEST DISTRICT, MANIPUR - 795001., OF 2020 (SEC XIV) IN THE SUPREME COURT OF INDIA BHEIGYABATI LEIKAI, IMPHAL MUNICIPAL COUNCIL P/0 AND 19/2017 AND R[70] IN RP NO. 3 DISTRICT- , MANIPUR P/S POROMPAT, IMPHAL EAST DISTRICT, MANIPUR, 795005., OF 2020 (SEC XIV) THROUGH DISTRICT- , MANIPUR MR. CHANDAN KUMAR (ADV.) FOR R[105] EXTRA-ORDINARY APPELLATE JURISDICTION THROUGH 20-A LAWYERS CHAMBER SUPREME COURT OF INIDA, DISTRICT- NEW DELHI, DELHI MR. CHANDAN KUMAR (ADV.) FOR R[65] 106 VICTORIA HUIDROM D/O HUIDROM MANGI SINGH, PID: 85151/2021 FOR R[106] IN WA NO Petition for Special Leave to Appeal (Civil) No. 7244 OF 2021 20-A LAWYERS CHAMBER SUPREME COURT OF INIDA, DISTRICT- NEW DELHI, DELHI R/O. HAOBAM MARAK NGANGOM LEIKAI, P.O.-IMPHAL, 19/2017 AND R[107] IN RP NO. 3 66 KHWAIRAKPAM TOMPOK SINGH S/O KH. SUBHAS SINGH, PID: 85111/2021 FOR R[66] IN WA NO PS.-SINGJAMEI, IMPHAL WEST DISTRICT, MANIPUR — OF 2020 (SEC XIV) WITH PRAYER FOR INTERIM RELIEF WANGKHEI ANGOM LEIKAI, IMPHAL EAST, P.O. -

One Stop Centre Directory (20.05.2020)
ONE STOP CENTRE DIRECTORY (20.05.2020) 1 S.No State/UT District Name Sakhi-One Stop Centre Contact Email Address Date of Address Details Operations 1. Andaman and Nicobars One Stop Centre, Perka, 03193-265121 [email protected] 6th September, Nicobar Islands Headquarters, Car Nicobar, om 2019 (UT) (3) Nicobars- 744301 2. North & One Stop Centre, Old DRDA 03192-273009 sakhiandaman@g 6th September, Middle Office, O/o. The Deputy mail.com 2019 Andaman Commissioner, Near State Library, Mayabunder, North & Middle Andaman-744204 3. South One Stop Centre, JG 6-Type, 0319-2230504 sakhiandaman@g 1st January,2016 Andaman V Quarter, Near Ayush, mail.com (Govt.) Hospital, Junglighat, Port Blair, South Andaman District, Andaman & Nicobar Islands 4. Andhra Pradesh Krishna One Stop Centre, Shaik Raja 9398914772, [email protected] 29th August, (13) Sahib Municipal Maternity 9949397133, m 2015 Hospital, Kothapet, 9440280053, Vijaywada City, Krishna 9398914772 District, Andhra Pradesh 5. Chittoor One Stop Centre, RIMS- 9959776697, [email protected] 15th December, General Hospital, Municipal 8897600654, m 2016 Maternity Ward, Chittoor 9951909222 City, Chittoor District, Andhra Pradesh 2 6. Andhra Pradesh Srikakulam One Stop Centre, RIMS- 9110793708, [email protected] 15th December, General Hospital, Balaga, 7386965008, m 2016 Srikakulam City, Srikakulam 7997879976, District, Andhra Pradesh- 532001 7. Anantapur One Stop Centre, Room 8008053408, [email protected] 15th December, No.12 & 13, Trauma Care, 6281298026, m 2016 Upstairs, Emergency Centre, 9110793708 Govt. General Hospital, Anantapur City, Anantapur District, Andhra Pradesh- 515001 8. Kurnool One Stop Centre, Room 08518-255057, [email protected] 15th December, No.214, Upstairs, 08008471794, m 2016 NtrVidyaSeva, Karyalayam, 09441303332, Govt. -

Media Factsheet on Issues of Citizenship in the Northeast (Educational Materials)
CALCUTTA RESEARCH GROUP 2020 NRC FACTSHEET Media Factsheet on Issues of Citizenship in the Northeast (Educational Materials) Compiled and Introduced by SUBIR BHAUMIK SAMIR PURKAYASTHA SAMRAT CHAUDHURY NRC FACTSHEET Media Factsheet on Issues of Citizenship in the Northeast (Educational Material) Compiled and Introduced by Subir Bhaumik Samir Purkayastha Samrat Chaudhury Calcutta Research Group 2020 1 The factsheet is for limited internal circulation within CRG and its partners, primarily to be used for purposes of education and as ready reference for resource persons and participants who join CRG’s annual Winter Migration Workshop and other CRG Orientation Programmes on related issues. CRG and the editors gratefully acknowledge their indebtedness to following media outlets / journals / websites which were all reaccessed between December 2019-March 2020: 1. PangSau 2. East Wind Journal 3. The Wire 4. Scroll.in 5. The Print 6. Firstpost 7. Caravan Magazine 8. NE Now 9. News18 10. Times of India 11. Hindustan Times 12. The Telegraph (Kolkata) 13. The Hindu 14. Frontline 15. Indian Express 16. Economic Times 17. NDTV 18. Business Standard 19. BBC 20. New York Times 21. The Guardian 22. Al Jazeera 23. Vice News 24. Amnesty International 25. India Today 26. Raiot 27. Newslaundry 28. Livemint 29. Countercurrents 30. The Federal 31. Quartz India 32. The Week 33. The Diplomat 34. DailyO 35. Himal Magazine The compilation is part of the material of the orientation programme in migration and forced migration studies. The programme is conducted by -
A Critical Analysis of Rural Industries in Manipur
International Journal of Humanities and Social Science Invention (IJHSSI) ISSN (Online): 2319 – 7722, ISSN (Print): 2319 – 7714 www.ijhssi.org ||Volume 9 Issue 9 Ser. II || September 2020 || PP 22-26 A Critical Analysis of Rural Industries in Manipur. H.Andrew Zimik Research, ScholarDepartment of Sociology, William Carey University Shillong, Meghalaya. ABSTRACT: The economy of Manipur is based on Agriculture, forest products, industries, mining and tourism sector. The state is divided into two geographical areas, i.e. the hills and the plains. The main economy of the hill areas is the agriculture and allied activities and forest products with prospects of tourism. Economically, the hill area which is inhabited by the tribal consisting of the Nagas and the Kukis are more backward, while the valley predominantly inhabited by the Meiteis are more advance and developed. Rural industries, if developed and planned properly will enhance the economy of the hill people of Manipur.The present paper is an attempt to criticallyanalyze the presence of rural industries in Ukhrul District of Manipur. It is also an attempt to study the factors for lack of rural industries in Ukhrul district. The various impacts resulting out of this problem in the economic growth and sustainable development of Ukhrul District is also critically analyze in the present paper. KEYWORDS:Rural industries, Ukhrul District, economic growth, sustainable development. --------------------------------------------------------------------------------------------------------------------------------------- Date of Submission: 04-09-2020 Date of Acceptance: 19-09-2020 --------------------------------------------------------------------------------------------------------------------------------------- I. INTRODUCTION Manipur, the “Land of Jewels” and “Switzerland of India”, an expression coined by Lord Irwin, is one of the 29 states of India located in the north-eastern part of India.