Part Ii – Neurological Disorders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

An Occupational Therapy Guide for Entry
University of North Dakota UND Scholarly Commons Occupational Therapy Capstones Department of Occupational Therapy 2008 An Occupational Therapy Guide for Entry-Level Therapists not Specializing in the Treatment of Upper Extremity Dysfunction: Three Common Cumulative Trauma Injuries Ryan Edwards University of North Dakota Follow this and additional works at: https://commons.und.edu/ot-grad Part of the Occupational Therapy Commons Recommended Citation Edwards, Ryan, "An Occupational Therapy Guide for Entry-Level Therapists not Specializing in the Treatment of Upper Extremity Dysfunction: Three Common Cumulative Trauma Injuries" (2008). Occupational Therapy Capstones. 57. https://commons.und.edu/ot-grad/57 This Scholarly Project is brought to you for free and open access by the Department of Occupational Therapy at UND Scholarly Commons. It has been accepted for inclusion in Occupational Therapy Capstones by an authorized administrator of UND Scholarly Commons. For more information, please contact [email protected]. AN OCCUPATIONAL THERAPY GUIDE FOR ENTRY-LEVEL THERAPISTS NOT SPECIALIZING IN THE TREATMENT OF UPPER EXTREMITY DYSFUNCTION: THREE COMMON CUMULATIVE TRAUMA INJURIES by Ryan Edwards Advisor: Anne Haskins PhD, OTR/L A Scholarly Project Submitted to the Occupational Therapy Department of the University of North Dakota In partial fulfillment of the requirements for the degree of Master’s of Occupational Therapy Grand Forks, North Dakota August 1, 2008 This Scholarly Project Paper, submitted by Ryan Edwards in partial fulfillment of the requirement for the Degree of Master’s of Occupational Therapy from the University of North Dakota, has been read by the Faculty Advisor under whom the work has been done and is hereby approved. -

An Improved Technique for Radial Nerve Conduction Studies
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.30.4.332 on 1 August 1967. Downloaded from J. Neurol. Neurosurg. Psychiat., 1967, 30, 332 An improved technique for radial nerve conduction studies ALLAN W. DOWNIE1 AND THOMAS R. SCOTT From the Division of Neurology, Department of Medicine, School of Medicine, University ofNorth Carolina, Chapel Hill, North Carolina, U.S.A. A technique for recording evoked sensory potentials MATERIALS AND METHOD from the radial nerve has already been reported by us (Downie and Scott, 1964). This technique, The apparatus used was a TECA two-channel electro- myograph. The recording electrodes consisted of a pair although reliable, is time consuming and occasion- of chlorided silver discs 1 cm. in diameter, mounted ally difficult and the amplitude of potentials may be 2 5 cm. apart on a plastic base. The active recording as low as 1 to 2 microvolts. The purpose of this electrode was placed over the largest palpable branch communication is to describe a simpler technique by of the radial nerve as it crossed the tendon of the extensor which potentials of greater amplitude can be pollicis longus. The distal recording electrode was placed obtained. In addition, the segment of nerve tested is over the first dorsal interosseous muscle but not neces- Protected by copyright. one which can be readily identified and biopsied if sarily over the nerve, of which the position in this area so desired without causing unpleasant or disturbing cannot be precisely determined (Fig. 1). An experiment sensory loss to the subject. made to assess the importance of the position of this electrode showed no significant difference in latency to The location of a nerve which is to be tested is peak when it was placed in turn on three points along usually determined by stimulating its motor fibres a line between the tendons of the extensor pollicis and finding the stimulus site from which maximal longus and extensor indicis provided the interelectrode muscle contraction is obtained. -

Clinical Presentations of Lumbar Disc Degeneration and Lumbosacral Nerve Lesions
Hindawi International Journal of Rheumatology Volume 2020, Article ID 2919625, 13 pages https://doi.org/10.1155/2020/2919625 Review Article Clinical Presentations of Lumbar Disc Degeneration and Lumbosacral Nerve Lesions Worku Abie Liyew Biomedical Science Department, School of Medicine, Debre Markos University, Debre Markos, Ethiopia Correspondence should be addressed to Worku Abie Liyew; [email protected] Received 25 April 2020; Revised 26 June 2020; Accepted 13 July 2020; Published 29 August 2020 Academic Editor: Bruce M. Rothschild Copyright © 2020 Worku Abie Liyew. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Lumbar disc degeneration is defined as the wear and tear of lumbar intervertebral disc, and it is mainly occurring at L3-L4 and L4-S1 vertebrae. Lumbar disc degeneration may lead to disc bulging, osteophytes, loss of disc space, and compression and irritation of the adjacent nerve root. Clinical presentations associated with lumbar disc degeneration and lumbosacral nerve lesion are discogenic pain, radical pain, muscular weakness, and cutaneous. Discogenic pain is usually felt in the lumbar region, or sometimes, it may feel in the buttocks, down to the upper thighs, and it is typically presented with sudden forced flexion and/or rotational moment. Radical pain, muscular weakness, and sensory defects associated with lumbosacral nerve lesions are distributed on -

Peroneal Nerve Injury Associated with Sports-Related Knee Injury
Neurosurg Focus 31 (5):E11, 2011 Peroneal nerve injury associated with sports-related knee injury DOSANG CHO, M.D., PH.D.,1 KRIANGSAK SAETIA, M.D.,2 SANGKOOK LEE, M.D.,4 DAVID G. KLINE, M.D.,3 AND DANIEL H. KIM, M.D.4 1Department of Neurosurgery, School of Medicine, Ewha Womans University, Seoul, Korea; 2Division of Neurosurgery, Department of Surgery, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand; 3Department of Neurosurgery, Louisiana State University Health Sciences Center, New Orleans, Louisiana; and 4Department of Neurosurgery, Baylor College of Medicine, Houston, Texas Object. This study analyzes 84 cases of peroneal nerve injuries associated with sports-related knee injuries and their surgical outcome and management. Methods. The authors retrospectively reviewed the cases of peroneal nerve injury associated with sports between the years 1970 and 2010. Each patient was evaluated for injury mechanism, preoperative neurological status, electro- physiological studies, lesion type, and operative technique (neurolysis and graft repair). Preoperative status of injury was evaluated by using a grading system published by the senior authors. All lesions in continuity had intraoperative nerve action potential recordings. Results. Eighty-four (approximately 18%) of 448 cases of peroneal nerve injury were found to be sports related, which included skiing (42 cases), football (23 cases), soccer (8 cases), basketball (6 cases), ice hockey (2 cases), track (2 cases) and volleyball (1 case). Of these 84 cases, 48 were identified as not having fracture/dislocation and 36 cases were identified with fracture/dislocation for surgical interventions. Good functional outcomes from graft repair of graft length < 6 cm (70%) and neurolysis (85%) in low-intensity peroneal nerve injuries associated with sports were obtained. -

A Guide to Transthyretin Amyloidosis
A Guide to Transthyretin Amyloidosis Authored by Teresa Coelho, Bo-Goran Ericzon, Rodney Falk, Donna Grogan, Shu-ichi Ikeda, Mathew Maurer, Violaine Plante-Bordeneuve, Ole Suhr, Pedro Trigo 2016 Edition Edited by Merrill Benson, Mathew Maurer What is amyloidosis? Amyloidosis is a systemic disorder characterized by extra cellular deposition of a protein-derived material, known as amyloid, in multiple organs. Amyloidosis occurs when native or mutant poly- peptides misfold and aggregate as fibrils. The amyloid deposits cause local damage to the cells around which they are deposited leading to a variety of clinical symptoms. There are at least 23 different proteins associated with the amyloidoses. The most well-known type of amyloidosis is associated with a hematological disorder, in which amyloid fibrils are derived from monoclonal immunoglobulin light-chains (AL amyloidosis). This is associated with a clonal plasma cell disorder, closely related to and not uncommonly co-existing with multiple myeloma. Chronic inflammatory conditions such as rheumatoid arthritis or chronic infections such as bronchiectasis are associated with chronically elevated levels of the inflammatory protein, serum amyloid A, which may misfold and cause AA amyloidosis. The hereditary forms of amyloidosis are autosomal dominant diseases characterized by deposition of variant proteins, in dis- tinctive tissues. The most common hereditary form is transthyretin amyloidosis (ATTR) caused by the misfolding of protein monomers derived from the tetrameric protein transthyretin (TTR). Mutations in the gene for TTR frequently re- sult in instability of TTR and subsequent fibril formation. Closely related is wild-type TTR in which the native TTR protein, particu- larly in the elderly, can destabilize and re-aggregate causing non- familial cases of TTR amyloidosis. -

Expert Consensus Recommendations to Improve Diagnosis of ATTR Amyloidosis with Polyneuropathy
Journal of Neurology https://doi.org/10.1007/s00415-019-09688-0 REVIEW Expert consensus recommendations to improve diagnosis of ATTR amyloidosis with polyneuropathy David Adams1 · Yukio Ando2 · João Melo Beirão3 · Teresa Coelho4 · Morie A. Gertz5 · Julian D. Gillmore6 · Philip N. Hawkins6 · Isabelle Lousada7 · Ole B. Suhr8 · Giampaolo Merlini9,10 Received: 10 December 2019 / Revised: 20 December 2019 / Accepted: 23 December 2019 © The Author(s) 2020 Abstract Amyloid transthyretin (ATTR) amyloidosis with polyneuropathy (PN) is a progressive, debilitating, systemic disease wherein transthyretin protein misfolds to form amyloid, which is deposited in the endoneurium. ATTR amyloidosis with PN is the most serious hereditary polyneuropathy of adult onset. It arises from a hereditary mutation in the TTR gene and may involve the heart as well as other organs. It is critical to identify and diagnose the disease earlier because treatments are available to help slow the progression of neuropathy. Early diagnosis is complicated, however, because presentation may vary and family history is not always known. Symptoms may be mistakenly attributed to other diseases such as chronic infammatory demyelinating polyradiculoneuropathy (CIDP), idiopathic axonal polyneuropathy, lumbar spinal stenosis, and, more rarely, diabetic neuropathy and AL amyloidosis. In endemic countries (e.g., Portugal, Japan, Sweden, Brazil), ATTR amyloidosis with PN should be suspected in any patient who has length-dependent small-fber PN with autonomic dysfunction and a family history of ATTR amyloidosis, unexplained weight loss, heart rhythm disorders, vitreous opacities, or renal abnormali- ties. In nonendemic countries, the disease may present as idiopathic rapidly progressive sensory motor axonal neuropathy or atypical CIDP with any of the above symptoms or with bilateral carpal tunnel syndrome, gait disorders, or cardiac hypertro- phy. -

GBS/CIDP Foundation International
Guillain-Barré Syndrome GBS: An Acute Care Guide For Medical Professionals A publication of the GBS/CIDP Foundation International Guillain-Barré Syndrome: An Acute Care Guide For Medical Professionals A publication of the GBS/CIDP Foundation International 2012 Edition GBS/CIDP Foundation International The Holly Building 104 1/2 Forrest Avenue Narberth, PA 19072 Phone: 610.667.0131 Toll Free: 866.224.3301 Fax: 610.667.7036 [email protected] www.gbs-cidp.org Guillain-Barré Syndrome: An Acute Care Guide For Medical Professionals Contents Page Acknowledgements . i Introduction . 1 Initial Patient Evaluation . 4 Natural History of GBS: Implications for Patient Care . 6 Respiratory Complications . 8 Dysautonomia and Cardiovascular Complications . 12 Bladder, Bowel Dysfunction . 14 Metabolism: Nutrition, Hydration, Electrolytes . 14 Pain . 17 ICU Delirium . 18 Skin . 18 Musculo-Skeletal Issues, Occupational and Physical Therapy . 19 Infection . 22 Disorder Specific Treatments . 22 Appendix A. Checklist of Patient Issues to Monitor . 24 B. Diagnostic Criteria for GBS . 25 C. Prognosis . 26 References . 27 This pamphlet is provided as a service of the GBS/CIDP Foundation International Serving the medical community and patients with Guillain-Barré syndrome and related acute and chronic paralyzing disorders of the peripheral nerves. Acknowledgements Guillain-Barré syndrome (GBS) is a rare disorder. Some health professionals may not be familiar with treating it. A beautiful video by Tanya Ooraikul chronicled the superb care provided to her husband Kit during his recovery from GBS. His care at Gray Nuns Community Hospital in Edmonton, Alberta, Canada included 86 days in the intensive care unit. The video handsomely demonstrates the high quality of care that can be provided for this rare and complicated disorder in a community hospital. -

LECTURE (SACRAL PLEXUS, SCIATIC NERVE and FEMORAL NERVE) Done By: Manar Al-Eid Reviewed By: Abdullah Alanazi
CNS-432 LECTURE (SACRAL PLEXUS, SCIATIC NERVE AND FEMORAL NERVE) Done by: Manar Al-Eid Reviewed by: Abdullah Alanazi If there is any mistake please feel free to contact us: [email protected] Both - Black Male Notes - BLUE Female Notes - GREEN Explanation and additional notes - ORANGE Very Important note - Red CNS-432 Objectives: By the end of the lecture, students should be able to: . Describe the formation of sacral plexus (site & root value). List the main branches of sacral plexus. Describe the course of the femoral & the sciatic nerves . List the motor and sensory distribution of femoral & sciatic nerves. Describe the effects of lesion of the femoral & the sciatic nerves (motor & sensory). CNS-432 The Mind Maps Lumber Plexus 1 Branches Iliohypogastric - obturator ilioinguinal Femoral Cutaneous branches Muscular branches to abdomen and lower limb 2 Sacral Plexus Branches Pudendal nerve. Pelvic Splanchnic Sciatic nerve (largest nerves nerve), divides into: Tibial and divides Fibular and divides into : into: Medial and lateral Deep peroneal Superficial planter nerves . peroneal CNS-432 Remember !! gastrocnemius Planter flexion – knee flexion. soleus Planter flexion Iliacus –sartorius- pectineus – Hip flexion psoas major Quadriceps femoris Knee extension Hamstring muscles Knee flexion and hip extension gracilis Hip flexion and aids in knee flexion *popliteal fossa structures (superficial to deep): 1-tibial nerve 2-popliteal vein 3-popliteal artery. *foot drop : planter flexed position Common peroneal nerve injury leads to Equinovarus Tibial nerve injury leads to Calcaneovalgus CNS-432 Lumbar Plexus Formation Ventral (anterior) rami of the upper 4 lumbar spinal nerves (L1,2,3 and L4). Site Within the substance of the psoas major muscle. -

Unilateral Foot Drop: an Unusual Presentation of a More Common
DOI: 10.7860/JCDR/2017/26249.10738 Case Report Unilateral Foot Drop: An Unusual Section Presentation of a more Common Internal Medicine Disease RAMESHWAR NATH CHAURASIA1, ABHISHEK PathaK2, VIJAY nath MISHRA3, DEEPIKA JOSHI4 ABSTRACT An isolated and unilateral foot drop due to intracranial lesion is quite rare. Presenting herein a case of a 14-year-old female who complained of inability to wear and hold slipper in her left foot. Detailed neurological examination revealed left foot dorsiflexion which had 1/5 muscle power along with brisk left ankle reflex. Magnetic resonance imaging of the brain revealed multiple conglomerate inflammatory granulomas in cerebrum and cerebellum, larger one in right parasagittal region with perifocal oedema. Magnetic resonance spectrum was suggestive of tuberculoma. Her chest X-ray chest revealed milliary shadowing. She was put on anti- tubercular drugs, steroid and a prophylactic anti-epileptic drug. The dorsiflexion improved to grade 4/5 after three weeks of treatment. The motor homunculus for foot is located in parasagittal area. Therefore, in patients with foot drop, we must keep high index of suspicion for parasagittal lesions, so that prompt diagnosis and early management can be done to prevent complications and improve the quality of life of patient. Keywords: Lower motor neuron, Magnetic resonance imaging, Spastic foot drop, Tuberculoma, Upper motor neuron CASE REPORT A 14-year-old female presented with history of difficulty in walking for last three days after left foot drop. She noticed difficulty in her left foot when she was trying to wear shoes go to school. Weakness gradually progressed within next two days so much so that she was unable to hold slipper and clear the ground without tripping by her left foot. -

Systemic Lupus Erythematosus Presenting with Finger Drop
DOI: 10.7860/JCDR/2018/36196.12107 Case Report Systemic Lupus Erythematosus Section Presenting with Finger Drop Internal Medicine MARJAN RAHIMI FARAHANI1, SAMIRA ALESAEIDI2 ABSTRACT Systemic Lupus Erythematosus (SLE) is an autoimmune disease with multiple organ involvement that can affect joints, skin, heart, lungs, kidneys and nervous system. SLE is a multisystem disorder resulting from abnormal immunological function. SLE affects women more than men. It affects both the central and the peripheral nervous system. Severe acute peripheral neuropathy in SLE is quite rare and it is always accompanied by evidence of active disease in other organs, including the central nervous system. The recognition of neurologic symptoms in SLE remains a clinical problem for physicians. Neurological manifestations are frequently present in SLE patients, although the peripheral nervous system involvement is rarer than the central one. Peripheral neuropathy is a known but uncommon presentation of SLE and the aim of this study is to report various forms of lupus-related neuropathies that may present as finger drop and discusses one of the rare neurological manifestations of lupus which remains a diagnostic challenge. Keywords: Autoimmune diseases, Nervous system, Pathology CASE REPORT A 33-year-old female was referred to the hospital with a chief compliant of symmetric finger drop of second, third and fourth fingers without any wrist drop for nine months before. She was able to use her fists but she had limitation on abduction of all fingers and also full extension of metacarpophalangeal and interphalangeal joints. The evaluation of sensation and reflexes were normal. The patient complained of shoulder, wrist, interphalangeal, knee, and elbow and ankle arthralgia. -

Anatomical, Clinical, and Electrodiagnostic Features of Radial Neuropathies
Anatomical, Clinical, and Electrodiagnostic Features of Radial Neuropathies a, b Leo H. Wang, MD, PhD *, Michael D. Weiss, MD KEYWORDS Radial Posterior interosseous Neuropathy Electrodiagnostic study KEY POINTS The radial nerve subserves the extensor compartment of the arm. Radial nerve lesions are common because of the length and winding course of the nerve. The radial nerve is in direct contact with bone at the midpoint and distal third of the humerus, and therefore most vulnerable to compression or contusion from fractures. Electrodiagnostic studies are useful to localize and characterize the injury as axonal or demyelinating. Radial neuropathies at the midhumeral shaft tend to have good prognosis. INTRODUCTION The radial nerve is the principal nerve in the upper extremity that subserves the extensor compartments of the arm. It has a long and winding course rendering it vulnerable to injury. Radial neuropathies are commonly a consequence of acute trau- matic injury and only rarely caused by entrapment in the absence of such an injury. This article reviews the anatomy of the radial nerve, common sites of injury and their presentation, and the electrodiagnostic approach to localizing the lesion. ANATOMY OF THE RADIAL NERVE Course of the Radial Nerve The radial nerve subserves the extensors of the arms and fingers and the sensory nerves of the extensor surface of the arm.1–3 Because it serves the sensory and motor Disclosures: Dr Wang has no relevant disclosures. Dr Weiss is a consultant for CSL-Behring and a speaker for Grifols Inc. and Walgreens. He has research support from the Northeast ALS Consortium and ALS Therapy Alliance. -
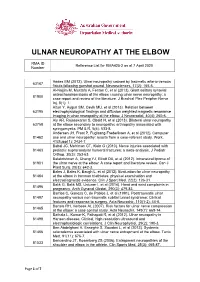
Reference List for RMA425-2 As at 7 April 2020 Number
ULNAR NEUROPATHY AT THE ELBOW RMA ID Reference List for RMA425-2 as at 7 April 2020 Number Addas BM (2012). Ulnar neuropathy caused by traumatic arterio-venous 63167 fistula following gunshot wound. Neurosciences, 17(2): 165-6. Al-Najjim M, Mustafa A, Fenton C, et al (2013). Giant solitary synovial osteochondromatosis of the elbow causing ulnar nerve neuropathy: a 81900 case report and review of the literature. J Brachial Plex Peripher Nerve Inj, 8(1): 1. Altun Y, Aygun SM, Cevik MU, et al (2013). Relation between 63195 electrophysiological findings and diffusion weighted magnetic resonance imaging in ulnar neuropathy at the elbow. J Neuroradiol, 40(4): 260-6. Aly AR, Rajasekaran S, Obaid H, et al (2013). Bilateral ulnar neuropathy 63758 at the elbow secondary to neuropathic arthropathy associated with syringomyelia. PM & R, 5(6): 533-8. Andersen JH, Frost P, Fuglsang-Frederiksen A, et al (2012). Computer 81462 use and ulnar neuropathy: results from a case-referent study. Work, 41(Suppl 1): 2434-7. Babal JC, Mehlman CT, Klein G (2010). Nerve injuries associated with 81463 pediatric supracondylar humeral fractures: a meta-analysis. J Pediatr Orthop, 30(3): 253-63. Balakrishnan A, Chang YJ, Elliott DA, et al (2012). Intraneural lipoma of 81901 the ulnar nerve at the elbow: A case report and literature review. Can J Plast Surg, 20(3): e42-3. Bales J, Bales K, Baugh L, et al (2012). Evaluation for ulnar neuropathy 81464 at the elbow in Ironman triathletes: physical examination and electrodiagnostic evidence. Clin J Sport Med, 22(2): 126-31. Balik G, Balik MS, Ustuner I, et al (2014).