Chapter 128 – Thyroid and Adrenal Disorders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Congenital Adrenal Hyperplasia in the Newborn
The Leo Fung Center for CAH and Disorders of Sex Development Congenital Adrenal Hyperplasia in the Newborn Contents Introduction 1 What is congenital adrenal hyperplasia? 1 Types of CAH 3 Diagnosing CAH in newborns 4 Treating CAH 5 Untreated CAH 7 CAH in children and young adults 8 Frequently asked questions 9 Glossary 11 Resources 13 Acknowledgments 14 Congenital Adrenal Hyperplasia in the Newborn 1 Introduction This handbook will provide you and your family information about congenital adrenal hyperplasia (CAH). While this guide will not answer all of your questions, it will provide basic medical facts that will help you to talk to your doctors. It is important to know that CAH cannot be cured but it can be treated. Your child will need to take medicine for the rest of his or her life. If your child takes this medicine, he or she should have a completely normal life in every way. Successful treatment requires teamwork between you and your doctor. The doctor will monitor your child in order to know what dose of medicine is needed. We ask that you give your baby the medication on the schedule recommended by your doctor. Your family is not alone. The Leo Fung Center for CAH and Disorders of Sex Development (DSD) at University of Minnesota Amplatz Children’s Hospital, provides a large network of support, including medical specialists, therapists and counselors who all have expertise in caring for patients with CAH. What is congenital adrenal hyperplasia? Let’s begin by examining each word. • Congenital means existing at birth (inherited). • Adrenal means that the adrenal glands are involved. -

Thyroid Hormone Misuse and Abuse
Endocrine (2019) 66:79–86 https://doi.org/10.1007/s12020-019-02045-1 REVIEW Thyroid hormone misuse and abuse Victor J. Bernet 1,2 Received: 11 June 2019 / Accepted: 2 August 2019 © Springer Science+Business Media, LLC, part of Springer Nature 2019 Abstract Thyroid hormone (TH) plays an essential role in human physiology and maintenance of appropriate levels is important for good health. Unfortunately, there are instances in which TH is misused or abused. Such misuse may be intentional such as when individuals take thyroid hormone for unapproved indications like stimulation of weight loss or improved energy. There are instances where healthcare providers prescribe thyroid hormone for controversial or out of date uses and sometimes in supraphysiologic doses. Othertimes, unintentional exposure may occur through supplements or food that unknowingly contain TH. No matter the reason, exposure to exogenous forms of TH places the public at risk for potential adverse side effects. Keywords Thyrotoxicosis ● Thyroid hormone abuse ● Thyroid hormone misuse ● Factitious thyrotoxicosis ● Supplements ● 1234567890();,: 1234567890();,: Analogs Overdose Thyroid hormone misuse and abuse secondary to exogenous TH ingestion that may be unin- tentional or purposeful such as in some cases of Munch- Almost any substance that impacts body physiology and ausen syndrome. Instances of TH misuse can be associated function is at risk for misuse or frank abuse, usually in the with the development of significant side effects. There are misgiven belief that the particular agent whether it be a other instances of chronic, low-grade over treatment with herb, supplement, medication, or hormone has healing TH, which occur for various misreasoning such as weight properties beyond that of which it actually possesses. -

Conduct Protocol in Emergency: Acute Adrenal Insufficiency
ORIGINAL ARTICLE FARES AND SANTOS Conduct protocol in emergency: Acute adrenal insufficiency ADIL BACHIR FARES1*, RÔMULO AUGUSTO DOS SANTOS2 1Medical Student, 6th year, Faculdade de Medicina de São José do Rio Preto (Famerp), São José do Rio Preto, SP, Brazil 2Degree in Endocrinology and Metabology from Sociedade Brasileira de Endocrinologia e Metabologia (SBEM). Assistant Physician at the Internal Medicine Service of Hospital de Base. Researcher at Centro Integrado de Pesquisa (CIP), Hospital de Base, São José do Rio Preto. Endocrinology Coordinator of the Specialties Outpatient Clinic (AME), São José do Rio Preto, SP, Brazil SUMMARY Introduction: Acute adrenal insufficiency or addisonian crisis is a rare comor- bidity in emergency; however, if not properly diagnosed and treated, it may progress unfavorably. Objective: To alert all health professionals about the diagnosis and correct treatment of this complication. Method: We performed an extensive search of the medical literature using spe- cific search tools, retrieving 20 articles on the topic. Results: Addisonian crisis is a difficult diagnosis due to the unspecificity of its signs and symptoms. Nevertheless, it can be suspected in patients who enter the emergency room with complaints of abdominal pain, hypotension unresponsive to volume or vasopressor agents, clouding, and torpor. This situation may be associated with symptoms suggestive of chronic adrenal insufficiency such as hyperpigmentation, salt craving, and association with autoimmune diseases such as vitiligo and Hashimoto’s thyroiditis. Hemodynamically stable patients Study conducted at Faculdade may undergo more accurate diagnostic methods to confirm or rule out addiso- de Medicina de São José do nian crisis. Delay to perform diagnostic tests should be avoided, in any circum- Rio Preto (Famerp), São José do Rio Preto, SP, Brazil stances, and unstable patients should be immediately medicated with intravenous glucocorticoid, even before confirmatory tests. -

Thyroid Disease Update
10/11/2017 Thyroid Disease Update • Donald Eagerton M.D. Disclosures I have served as a clinical investigator and/or speakers bureau member for the following: Abbott, Astra Zenica, BMS, Boehringer Ingelheim, Eli Lilly, Merck, Novartis, Novo Nordisk, Pfizer, and Sanofi Aventis Thyroid Disease Update • Hypothyroidism • Hyperthyroidism • Thyroid Nodules • Thyroid Cancer 1 10/11/2017 2 10/11/2017 Case 1 • 50 year old white female is seen for follow up. Notices cold intolerance, dry skin, and some fatigue. Cholesterol is higher than prior visits. • Family history; Mother had history of hypothyroidism. Sister has hypothyroidism. • TSH = 14 (0.30- 3.3) Free T4 = 1.0 (0.95- 1.45) • Weight 70 kg Case 1 • Next step should be • A. Check Free T3 • B. Check AntiMicrosomal Antibodies • C. Start Levothyroxine 112 mcg daily • D. Start Armour Thyroid 30 mg q day • E. Check Thyroid Ultrasound Case 1 Next step should be • A. Check Free T3 • B. Check AntiMicrosomal Antibodies • C. Start Levothyroxine 112 mcg daily • D. Start Armour Thyroid 30 mg q day • E. Check Thyroid Ultrasound 3 10/11/2017 Hypothyroidism • Incidence 0.1- 2.0 % of the population • Subclinical hypothyroidism in 4-10% of the adult population • 5-8 times higher in women An FT4 test can confirm hypothyroidism 13 • In the presence of high TSH and FT4 levels in relation to the thyroid function TSH, low FT4 (free thyroxine) usually signalsTSH primary hypothyroidism12 Overt Mild Mild Overt Euthyroidism FT4 Hypothyroidism Thyrotoxicosis* Thyrotoxicosis vs. hyperthyroidism¹ While these terms are often used interchangeably, thyrotoxicosis (toxic thyroid), describes presence of too much thyroid hormone, whether caused by thyroid overproduction (hyperthyroidism); by leakage of thyroid hormone into the bloodstream (thyroiditis); or by taking too much thyroid hormone medication. -

Preventable Deaths: Panhypopituitarism and Adrenal Insufficiency
Preventable Deaths: Panhypopituitarism and adrenal insufficiency. What you need to know What is panhypopituitarism? Your child has been diagnosed with a big scary sounding word, and all you can think is: 'What does this mean? and 'Why have I never heard of this?' Simply put, panhypopituitarism means that your child's pituitary gland does not function properly and as a result, your child is deficient in one or several hormones. Some children have congenital panhypopituitarism, meaning they are born with it. Others have acquired panhypopituitarism following an event such as head trauma, brain tumor surgery, or brain radiation. It is rare enough that is entirely possible, in fact, probable, that you will not initially know anyone else with this disorder. What will my child need? Although the diagnosis and condition can seem intimidating, it is very manageable once you understand what is needed. Unfortunately the condition cannot be cured or reversed, but again, it can be effectively managed. Your child will need to take medications to replace the missing hormones. These might include thyroid hormone, growth hormone, cortisol, and/or possibly others. Your doctor will go over these with you, as dosages vary from child to child. Most medications are taken orally, but growth hormone must be taken by daily injection. Your endocrinologist will work with you and your child to achieve the proper dosages and will guide you in how to administer any necessary medications. Why is it sometimes life threatening? What is adrenal insufficiency? Of the hormone deficiencies your child may have, the most critical is cortisol, also known as the 'stress hormone.' Cortisol is essential for life , and is therefore the central focus of this guide. -

The Subacute Thyroiditis, Since Its First Description by De Quervain (1904), Has Been Reported Under Many Synonyms
Endocrinol. Japon. 1964, 11 (2), 119~138 STUDIES ON SUBACUTE THYROIDITIS SHOZO SAITO Department of Radiology, School of Medicine, Gunma University, Maebashi The subacute thyroiditis, since its first description by de Quervain (1904), has been reported under many synonyms. Terms given with reference to the histo- logic features of this disease include "pseudotuberculous thyroiditis", "granulo- matous thyroiditis", "gaint-cell thyroiditis", "de Quervain's thyroiditis", "struma granulomatosa" or "struma fibrosa, giant cell variant". The clinical findings have given rise to such names as" acute and subacute nonsuppurative thyroiditis", "acute noninfectious thyroiditis"and"subacute thyroiditis" . In recent writings, the disease is most commonly referred to as subacute thyroiditis. Later, de Quervain and Giordanengo (1936) collected reports of 54 cases of the disease, appearing in the literature since de Quervain's original description, and clearly distinguished it from other forms of thyroiditis. Several years ago, the disease had been considered relatively rare, but with recent advance in endocrinology, more attentions have been drawn by it, and more reports published on it. For the past six years, the author has treated 51 cases of subacute thyroiditis, and obtained findings of interest, which are outlined in this paper. METHODS OF EXAMINATION The disease was confirmed by Silverman's needle biopsy (Crile and Rumsey, 1950; Crile and Hazard, 1951) of the thyroid in 36 of them, and the others were diagnosed by typical clinical symptoms, characteristic results of thyroidal function test and accelerated red cell sedimentation rate and its clinical course. Thyroid function test Basal metabolic rate (BMR) was examined by Knipping's method (normal range•}15%), and serum protein-bound iodine (PBI) by modification of Barker's method (Barker and Humphrey, 1950). -

A Case of Thyrotoxic Paralysis Caused by Consumption of Iodocaseine
Journal of Health and Social Sciences 2019; 4,2:277-282 CASE REPORT IN EMERGENCY MEDICINE A case of thyrotoxic paralysis caused by consumption of iodocaseine Antonio Villa1, Gabriella Nucera2 Affiliations: 1 M.D., Department of Emergency, ASST Monza, PO Desio, Monza, Italy 2 M.D., Department of Emergency Medicine, ASST Fatebenefratelli-Sacco, PO Fatebenefratelli, Milano, Italy Corresponding author: Dr Antonio Villa, ASST Monza, PO Desio. Via Fiuggi, 56 20159 Milan, Italy. E-mail: [email protected] Abstract Acute hypokalaemic paralysis is a rare but treatable cause of acute limb weakness. Thyrotoxic paralysis is an uncommon, potentially life-threatening endocrine emergency and it is a rare complication of hyperthyroidism. The most common causes of hyperthyroidism include Graves’ disease, multinodular goiters or solitary thyroid nodule, and iodine-induced thyrotoxicosis ( Jod-Basedow syndrome). Thyreotoxicosis factitia, which is caused by the excessive ingestion of exogenous thyroid hormone or iodine derivatives administration, has been rarely reported as a cause of thyrotoxic paralysis. We describe the case of a young Caucasian male with flaccid paralysis of all four limbs and severe hypokalaemia after inappropriate iodine derivatives (iodocasein) intake to show, in conclusion, how critical care physicians need to be aware of this rare but curable condition. KEY WORDS: Iodocaseine; hypokalaemia; thyrotoxic paralysis. 277 Journal of Health and Social Sciences 2019; 4,2:277-282 Riassunto La paralisi acuta ipokaliemica è una causa rara ma curabile di astenia acuta. La paralisi tireotossica è un'e- mergenza endocrina non comune e potenzialmente pericolosa per la vita ed è una rara complicanza dell'i- pertiroidismo. L'ipertiroidismo è causato prevalentemente dalla malattia di Graves, da gozzi singoli o multi- nodulari, e dalla malattia indotta da iodio ( Jod-Basedow). -

Beyond the Fixed Setpoint of the Hypothalamus–Pituitary–Thyroid Axis
E Fliers and others Hypothalamus–pituitary– 171:5 R197–R208 Review thyroid axis MECHANISMS IN ENDOCRINOLOGY Beyond the fixed setpoint of the hypothalamus–pituitary–thyroid axis Eric Fliers1, Andries Kalsbeek1,2 and Anita Boelen1 Correspondence should be addressed 1Department of Endocrinology and Metabolism, Academic Medical Center, University of Amsterdam, 1105 AZ to E Fliers Amsterdam, The Netherlands and 2Hypothalamic Integration Mechanisms, Netherlands Institute for Neuroscience, Email Amsterdam, The Netherlands e.fl[email protected] Abstract The hypothalamus–pituitary–thyroid (HPT) axis represents a classical example of an endocrine feedback loop. This review discusses dynamic changes in HPT axis setpoint regulation, identifying their molecular and cellular determinants, and speculates about their functional role. Hypothalamic thyrotropin-releasing hormone neurons were identified as key components of thyroid hormone (TH) setpoint regulation already in the 1980s, and this was followed by the demonstration of a pivotal role for the thyroid hormone receptor beta in negative feedback of TH on the hypothalamic and pituitary level. Gradually, the concept emerged of the HPT axis setpoint as a fixed entity, aiming at a particular TH serum concentration. However, TH serum concentrations appear to be variable and highly responsive to physiological and pathophysiological environmental factors, including the availability or absence of food, inflammation and clock time. During food deprivation and inflammation, TH serum concentrations decrease without a concomitant rise in serum TSH, reflecting a deviation from negative feedback regulation in the HPT axis. Surprisingly, TH action in peripheral organs in these conditions cannot be simply predicted by decreased serum TH concentrations. Instead, diverse environmental stimuli have differential effects on local TH metabolism, e.g. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Hypothyroidism
Hypothyroidism Alejandro Diaz, MD,*† Elizabeth G. Lipman Diaz, PhD, CPNP‡ *Miami Children’s Hospital, Miami, FL †The Herbert Wertheim College of Medicine, Florida International University, Miami, FL ‡University of Miami School of Nursing and Health Studies, Miami, FL Educational Gap Congenital hypothyroidism is one the most common causes of preventable intellectual disability. Awareness that not all cases are detected by the newborn screening is important, particularly because early diagnosis and treatment are essential in preserving cognitive abilities. Objectives After completing this article, readers should be able to: 1. Identify the causes of congenital and acquired hypothyroidism in infants and children. 2. Interpret an abnormal newborn screening result and understand indications for further evaluation and treatment. 3. Recognize clinical signs and symptoms of hypothyroidism. 4. Understand the importance of early diagnosis and treatment of congenital hypothyroidism. 5. Understand the presentation, diagnostic process, treatment, and prognosis of Hashimoto thyroiditis. 6. Differentiate thyroid-binding globulin deficiency from central hypothyroidism. AUTHOR DISCLOSURE Drs Diaz and Lipman Diaz have disclosed no financial relationships 7. Identify sick euthyroid syndrome and other causes of abnormal thyroid relevant to this article. This commentary does function test results. not contain a discussion of an unapproved/ investigative use of a commercial product/ device. ABBREVIATIONS CH congenital hypothyroidism BACKGROUND FT3 free triiodothyronine FT4 free thyroxine The thyroid gland produces hormones that have important functions related to energy HT Hashimoto thyroiditis metabolism, control of body temperature, growth, bone development, and maturation LT4 levothyroxine of the central nervous system, among other metabolic processes throughout the body. rT3 reverse triiodothyronine The thyroid gland develops from the endodermal pharynx. -
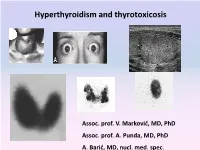
Hyperthyroidism and Thyrotoxicosis
Hyperthyroidism and thyrotoxicosis Assoc. prof. V. Marković, MD, PhD Assoc. prof. A. Punda, MD, PhD A. Barić, MD, nucl. med. spec. Hyperthyroidism- Thyrotoxicosis Hyperthyroidism- elevated serum levels of thyroid hormones caused by overproduction of thyroid hormones Thyrotoxicosis: elevated serum level of thyroid hormones/ excessive amount of circulating thyroid hormone Hyperthyreoidism includes thyreotoxycosis but Thyrotoxicosis is not exclusively caused by hyperthyroidism Classification of thyrotoxicosis Hyperthyroidism Thyrotoxicosis without hyperthyroidism Mb Basedow-Graves Thyrotoxicosis factitia Multinodular toxic goiter Subacute thyroiditis (painfull) Toxic adenoma Subacute thyroiditis (painless) Elevated TSH levels Ectopic thyroid tissue Trophoblastic tumors Iod-Basedow Diffuse toxic goiter (Mb Basedow, Graves) Diffuse toxic goiter Mb. Graves-Basedow Epidemiology and etiology Diffuse toxic goiter (Mb. Graves- Basedow) is an autoimune, multysistemic dissease, wich includes the thyoid gland, infiltrative ophthalmopathy, dermopathy and acropathy. World wide prevalence is about 0,4-2% in women, 0,1% in men, includes 60-90% of hyperthyroidism cases*. It is complex disease with predominant genetic component.& Sex hormones, stress. Disease is caused by TSH receptor stimulating antibodies/ TSH stimulating antibodies (TSAb), in 80-100% patients. *Taunbridge WMG, Vanderpump MPJ. Population screening for autoimmune thyroid disease. Endocriol Metab Clin North Am. 2000;29:239-253. &Brix TH, Kyvik KO, Christensen K, et al. Evdence for a major -

Mechanisms and Clinical Consequences of Critical Illness Associated Adrenal Insufficiency Paul E
Mechanisms and clinical consequences of critical illness associated adrenal insufficiency Paul E. Marik Purpose of review Abbreviations Adrenal insufficiency is being diagnosed with increasing ACTH adrenocorticotrophic hormone frequency in critically ill patients. There exists, however, ARDS acute respiratory distress syndrome CBG corticosteroid-binding globulin much controversy in the literature as to the nature of this CIRCI critical illness-related corticosteroid insufficiency entity, including its pathophysiology, epidemiology, CRH corticotrophin-releasing hormone HDL high-density lipoprotein diagnosis and treatment. The review summarizes our HPA hypothalamic–pituitary–adrenal current understanding of the causes and consequences of SAS sympatho-adrenal system TNF tumor necrosis factor adrenal insufficiency in critically ill patients. Relevant findings Activation of the hypothalamic–pituitary–adrenal axis with ß 2007 Lippincott Williams & Wilkins the production of cortisol is a fundamental component of 1070-5295 the stress response and is essential for survival of the host. Dysfunction of the hypothalamic–pituitary–adrenal axis with decreased glucocorticoid activity is being increasingly Introduction recognized in critically ill patients, particularly those with The stress system receives and integrates a diversity of sepsis. This condition is best referred to as ‘critical illness- cognitive, emotional, neurosensory and peripheral related corticosteroid insufficiency’. Critical illness-related somatic signals that arrive through distinct