Appendix 5A – Shortlist of 8 Options Evaluation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Destination Management Plan 2014/17 a Good Place to Live Is A
Telford and Wrekin Destination Management Plan 2014/17 A good place to live is a good place to visit Telford and Wrekin Destination Management Plan 2014/17 Contents 1 Introduction & Background 3 2 National, Strategic & Local Context 6 3 Telford’s Visitor Economy: Perceptions, Profile & Performance 17 4 Key Findings & Strategic Priorities 68 5 Action Plan (see separate document) 77 6 Appendices 78 7 List of Reference Documents 82 Maps 83 2 3 1 Introduction & background 1.1 Telford and Wrekin Madeley forms the eastern gateway of the Ironbridge Gorge WHS. Recorded in Domesday Offering the best of urban and rural, this destination it hid the future King Charles II after the Battle of has it all; from its award winning World Heritage Worcester in 1651 and is on the South Telford Site Museums and Convention Centre to charming Heritage Trail. market towns and villages. A destination located in the Heart of England; easy to reach, but still largely Only 3 miles away from the Gorge is the historic undiscovered. town of Much Wenlock celebrated for its role in the rebirth of the modern Olympic Games through Dr The Telford and Wrekin area in Shropshire celebrates William Penny Brookes, who started the Wenlock the best of old and new, much to the surprise of many Olympian Games in 1850. of its visitors. It is partly bordered by Staffordshire to the east with the M54 going east to the Black Country About 90% of Telford and Wrekin is covered by and Birmingham and west to Shrewsbury and Wales. green open space and natural features and includes The River Severn flows south east from Shrewsbury, attractive villages and market towns some of which cutting a dramatic swathe through what was known as were amalgamated into the new town of Telford Coalbrookdale and today forms the southern boundary almost 50 years ago. -

Telford & Wrekin Council
TELFORD & WREKIN COUNCIL West Midlands Property Alliance Using assets for growth Introduction Background Telford and Wrekin is a unitary district with borough status in the West Midlands. The district was created in 1974 as The Wrekin, then a non-metropolitan district of Shropshire. In 1998 the district became a unitary authority and was renamed Telford and Wrekin. It remains part of the Shropshire ceremonial county and shares institutions such as the Fire and Rescue Service with the rest of Shropshire. The borough’s major settlement is Telford, a new town designated in the 1960s incorporating the existing towns of Dawley, Madeley, Oakengates and Wellington. Telford was a new town run by the Telford Development Corporation (TDC) from the 1960s to the changes in 1974. Telford is located in central England with excellent connectivity by road and rail to Birmingham, Manchester, London and other centres. This connectivity includes an international railfreight park serving businesses looking to move goods across the UK and to air and sea ports. The population of the borough is 173,000 set to rise to 200,000 by 2030. The town was designed to accommodate a population of 200,000 and so has the necessary space and infrastructure for a growth area. Telford is home to more than 5,000 companies of which 150 are international. It has a strong automotive and engineering base as well as a broad range of other companies. There is a ready workforce of 350,000 within a 30 minute drive of Telford. Situated just 12 miles from the new Jaguar Landrover plant at i54 Telford is well placed to capitalise on supply chain opportunities. -
RBC Mixed Use Sheet.Indd
The following are examples of projects we have recently completed Chiltern Street London RBC were appointed by Galliard Homes to provide full Building Control services for a development known as The Chilterns. This is a prestigious development which consists of 44 exquisite apartments that have been expertly designed to combine the highest technical specifications; a gymnasium, cinema, shops, library and car parking. Mixed Use & Shopping Centres Mixed Newbury Parkway Berkshire RBC worked with the Building Design Partnership headed by the Shearer Property Group and Standard Life Investments, for a major mixed-use regeneration scheme of Newbury town centre. The £120 million redevelopment of the 5.7 acre site includes 270,000 sq ft of retail space comprising major department stores for Debenhams, John Lewis, large fashion stores, a mix of medium and smaller retail units, and catering outlets. There is also a major residential component and car parking for up to 600 cars. Shopping Centres Nationwide RBC have worked on many high profile shopping centres, providing building control services for retail clients, below is a small selection of these: Arndale Centre Swan Shopping Centre Manchester Eastleigh Brentcross Shopping Centre Telford Shopping Centre London Shropshire Bullring Shopping Centre The Chimes Shopping Centre Birmingham Middlesex Churchill Square Shopping Centre The Cornbow Shopping Centre Brighton Halesowen Eagles Meadow Shopping Centre The Gracechurch Centre Wrexham West Midlands Eastgate Shopping Centre The Oracle Shopping Centre -

Telford Central Station I Onward Travel Information Buses and Taxis Local Area Map
Telford Central Station i Onward Travel Information Buses and Taxis Local area map Key A Bus Stop Rail replacement Bus Stop Station Entrance/Exit Taxi Rank U Telford Central Station FR Telford Central Station Key A B CW Cineworld Imax Cinema FR The Forge Retail Park IC The International Centre, Telford OC Odeon Cinema TB TW OC SC Telford Shopping Centre TB Telford Bridge Retail Park TI Telford Ice Rink TW Telford & Wrekin Council University of Wolverhampton U (Telford Campus) SC Cycle routes Footpaths Bus Station CW TI Telford is a area PlusBus ICContains Ordnance Survey data © Crown copyright and database right 2018 & also map data © OpenStreetMap contributors, CC BY-SA In the event of engineering work, the bus or coach will collect from the PlusBus is a discount price ‘bus pass’ that you buy with your train ticket. It gives you unlimited bus travel around your forecourt at the front of the station at the end of Euston Way. chosen town, on participating buses. Visit www.plusbus.info Main destinations by bus (Data correct at June 2019) DESTINATION BUS ROUTES BUS STOP DESTINATION BUS ROUTES BUS STOP DESTINATION BUS ROUTES BUS STOP ^ 891 Bus Station Lilleshall (for Lilleshall Taxi is advisable or it’s a Albrighton 5 B { Bridge Retail Park 13 Bus Station Abbey) 15 minutes walk from this { Madeley 1, 2, 8, 18 Bus Station University - Telford Campus station (see Local area Bridgnorth < 8, 113, 114 Bus Station map) { Brookside 1, 3 Bus Station { Madeley (#) 4 A WU1+ A Broseley 8, 18 Bus Station Much Wenlock 18 Bus Station B { Muxton 5 B 4 Bucks -

Marches Draft Strategic Economic Plan 2013
19th December 2013: DRAFT Accelerating Growth through Opportunity Draft Strategic Economic Plan 2014 -2020 1 Contents Page Contents 2 Foreword from the Chair of the Marches LEP 4 1 The Marches 5 2 A Context for Growth 7 2.1 Our Vision & Our Area 8 3 The Marches Local Growth Deal 12 3.1 Accelerated Growth Scenario 14 3.2 The Marches Investment Fund 14 3.3 Unlocking Land for Housing and Employment Growth 17 3.4 Transport Infrastructure for Growth 18 3.5 Freedoms to Pool Existing Resources to Address Youth Unemployment and Skills 19 4 The Marches Growth Strategy 20 4.1 Physical Infrastructure 20 Housing and Employment Sites 20 Supporting Growth through Transport Improvements 23 Broadband and Telecommunications 24 4.2 Supporting Business 25 Growth Sectors, Strengths and Opportunities 26 Food and Drink 28 Defence and Security 30 Advanced Manufacturing 31 Visitor Economy 32 Environmental Technologies and Services 34 4.3 The Skills Proposal 35 Scope for supporting further and higher education in the Marches 35 Higher Education 36 A New Higher Education Facility in the Marches 38 4.4 Low Carbon Economy 38 4.5 Social Inclusion 39 5 Governance for Accelerating Growth 41 5.1 Commitment to Good Governance 41 5.2 Governing Growth 41 5.3 Governance Structure 42 5.4 A Track Record of Good Financial Governance 46 2 Page Appendices Appendix A SWOT Analysis 47 Appendix B Key Sites 52 Appendix C Project List 56 Appendix D HE Evidence 78 Appendix E Transport Strategy 81 Appendix F Synergising Funding 100 3 Foreword from the Chair of the Marches LEP The Marches provides an outstanding business environment. -

Impact of Sustainable Transport Measures on Town Centres
Local Sustainable Transport Fund Case Study Evaluation – Impact of Sustainable Transport Measures on Town Centres SUPPORTING TECHNICAL APPENDICES Department for Transport July 2017 LSTF Case Study Evaluation - Impact of Sustainable Transport Measures on Town Centres Supporting Technical Appendices Notice This document and its contents have been prepared and are intended solely for Department for Transport’s information and use in relation to the LSTF Case Study Evaluation Study. Atkins assumes no responsibility to any other party in respect of or arising out of or in connection with this document and/or its contents. Document history Job number: 5127520 Revision Purpose description Originated Checked Reviewed Authorised Date Rev 1.0 Initial draft for DfT review AL, EH, KQ, JR JR - 26/08/16 Accent Rev 2.0 Version 2 addressing AL, Accent JR JR JR 13/12/16 comments from DfT and Peer Reviewer Rev 3.0 Updated draft responding JR - - - 03/03/17 to final comments from DfT (FINAL VERSION) Atkins LSTF Case Study Evaluation - Impact of Sustainable Transport Measures on Town Centres Supporting Technical Appendices Table of contents Chapter Pages Part A - Introduction and Methodology 1. Introduction 7 1.1. Introduction 7 1.2. Study purpose and context 7 1.3. Evaluation aims and research questions 7 1.4. High level programme and study timescales 8 2. Methodology 9 2.1. Introduction 9 2.2. Overall approach 9 2.3. Overview of evidence base 11 2.4. Data issues and limitations 19 Part B – Telford Case Study 3. Introduction 22 3.1. Introduction 22 4. Rationale for LSTF bid 23 4.1. -

Director of Strategy and Transformation Candidate Pack
WE ARE LOOKING FOR A LEADER TO HELP SHAPE THE FUTURE OF OUR TRUST DIRECTOR OF STRATEGY AND TRANSFORMATION CANDIDATE INFORMATION PACK DECEMBER 2018 www. jobs.sath.nhs.uk1 DEAR CANDIDATE Thank you for expressing an interest in this exciting new role. Our Trust is at a signicant cross roads. As we prepared to move into the implementation stages of Future Fit which will see our clinical strategy realised, we are also investing heavily in new technology. This exciting future is featured within our Improvement Plans for the Trust which will see us move out of special measures. Our partnership with the Virginia Mason Institute is establishing a new continuous improvement culture and supporting engagement and charge through our people. This role is pivotal to the success of our organisation. The role will lead the development of our Strategy and Business Planning, as well as having a fey focus on the continuous improvement agenda for the Trust, supported by our partnership with the Virginia Mason Institute (VMI). The next 5 years will be lled with opportunities as we deliver our improvement plan and progress Future Fit to deliver £312m investment into our health system. You will be a dynamic, innovative and a values-based leader; we are looking for someone exceptional and we can promise that your time with us will be both regarding and stimulating. We are not going to be reserved in the type of person we are looking for in this role; we want an exceptional leaders who will have the courage, drive and ambition to support our organisation to move forward. -

Evolutionary Consultant in Radiology (Breast) Candidate Information Pack June 2018
BELONG TO SOMETHING EVOLUTIONARY CONSULTANT IN RADIOLOGY (BREAST) CANDIDATE INFORMATION PACK JUNE 2018 jobs.sath.nhs.uk/legacy1 CONTENTS 3 ABOUT THE TRUST, OUR SERVICES, COMMUNITIES AND PARTNERSHIPS 8 EDUCATION AND TEACHING 9 OUR STRATEGY AND VALUES 10 HOW WE ARE DELIVERING CHANGE 11 LIVING AND WORKING IN SHROPSHIRE 16 UK WORKING VISA ENTRY REQUIREMENTS AND SUPPORT BESPOKE PACKAGES 17 JOB DESCRIPTION 20 PROVISIONAL JOB PLAN 28 PERSON SPECIFICATION 2 jobs.sath.nhs.uk/legacy ABOUT THE TRUST The Shrewsbury and Telford Hospital NHS Trust is the main provider of acute hospital services for around half a million people in Shropshire, Telford & Wrekin and mid Wales. Encompassing some of the most picturesque parts We employ almost 6,000 staff, and hundreds of staff of England and Wales, the Trust’s catchment stretches and students from other organisations also work in our from the Cambrian Mountains in the west to Newport hospitals. We benefit from around 1,000 wonderful and the fringes of the Black Country in the east. volunteers at the Trust and our main charitable partners are The main towns include: Bridgnorth, Ludlow, Market the league of friends at the Royal Shrewsbury Hospital and Drayton, Oswestry, Shrewsbury and Whitchurch at the Princess Royal Hospital and the Lingen Davies cancer (in Shropshire); Newport, Telford and Wellington appeal which is based at the Royal Shrewsbury Hospital. (in Telford & Wrekin); and Newtown and Welshpool In addition to this we also provide services such as (in Powys) – all beautiful and unique. consultant -led outreach clinics at clinics at the Wrekin Our main service locations are the Princess Community Clinic, Telford, the Robert Jones and Agnes Royal Hospital (PRH) in Telford and the Royal Hunt Orthopaedic Hospital, Gobowen and the Bridgnorth, ShrewsburyHospital (RSH) in Shrewsbury which are Ludlow and Whitchurch Community hospitals. -
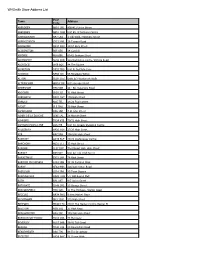
Placement Contact Lists from 2019
Placement Contact Lists FROM 2019 Placement Placement Address1 Placement Address 2 Town Postcode Occupational Area Type of Business Contact Telephone No. Email Address 3D Hair Studio 50 West Street St Georges Telford TF2 9 Hairdressers assistant Hairdressers Deborah Heaney 07813 712610 [email protected] 7 Sence Event Management The Town House Oswestry SY11 1AQ Business Admin/Professional Management Charlotte Gwynne (Event 01691 670027 Manager) 7 Valley Transport Unit 29 Shifnal TF11 8SD Transport Glenys Hillman - Owner 01952 461991 A H Griffiths 11 Bull Ring Ludlow SY8 1AD Retail / Customer Service Matthew Sylvester - Manager 01584 872141 A Ryan & Son 60 High Street Much Wenlock TF13 6AE Retail / Customer Service Sue Ryan - Manager 01952 727409 A T Browns Hortonwood 50 Telford TF1 7GZ Motor Vehicle & Associated Trade Dave Price - Operations 01952 605331 Manager A Walters Electrician Contractor 62 Longden Road Shrewsbury SY3 7HG Plant and Tool Hire/ Contractor Mike Davis- Operations Director 01743 247850 Aardvark Books Ltd The Bookery Bucknell SY7 0DH Retail / Customer Service Sarah Swinson (Director) 01547 530744 Abacus Day Nursery (Newport) 38 St Mary's Street Newport TF10 7AB Educational Leanne Nolan 01952 813652 Abbey Veterinary Centre (Shawbury) High Ridge Shrewsbury SY4 4NW Working With Animals Tracie Howells 01939 250655 ABC Day Nursery (Hadley) Crescent Road Telford TF1 5JU Educational Emma Burrows 01952 387190 ABC Day Nursery (Hoo Farm) Hoo Farm Animal kingdom, Telford TF6 6DJ Educational Lucy Holbrook - Manager 01952 -
Whsmith Store Address List
WHSmith Store Address List Post Town Address Code ABERDEEN AB10 1PD 408/412 Union Street ABERDEEN AB10 1HW Unit E5, St Nicholas Centre ABERGAVENNY NP7 5AG 1 Cibi Walk, Frogmore Street ABERYSTWYTH SY23 2AB 36 Terrace Road ABINGDON OX14 3QX 13/14 Bury Street ACCRINGTON BB5 1EX 14 Cornhill AIRDRIE ML6 6BU 60-62 Graham Street ALDERSHOT GU11 1DB 12a Wellington centre, Victoria Road ALDRIDGE WS9 8QS 44 The Square ALFRETON DE55 7BQ Unit B, Institute Lane ALNWICK NE66 1JD 56 Bondgate Within ALTON GU34 1HZ Units 6/7 Westbrook Walk ALTRINCHAM WA14 1SF 8/12 George Street AMERSHAM HP6 5DR 48 - 50, Sycamore Road ANDOVER SP10 1LJ 31 High Street ARBROATH DD11 1HY 196 High Street ARNOLD NG5 7EL 24/26 Front Street ASCOT SL5 7HG 39 High Street ASHBOURNE DE6 1GH 4 St John Street ASHBY DE LA ZOUCHE LE65 1AL 28 Market Street ASHFORD TN24 8TB 70/72 High Street ASHTON-UNDER-LYNE OL6 7JE Unit 30, Arcade Shopping Centre AYLESBURY HP20 1SH 27/29 High Street AYR KA7 1RH 198/200 High Street BANBURY OX16 5UE 23/24 Castle Quay Centre BANCHORY AB31 5TJ 33 High Street BANGOR LL57 1NY The Market Hall, High Street BARNET EN5 5XY Unit 22 111 High Street BARNSTAPLE EX31 1HP 76 High Street BARROW-IN-FURNESS LA14 1DB 38-42 Portland Walk BARRY CF63 4HH 126/128 Holton Road BASILDON SS14 1BA 29 Town Square BASINGSTOKE RG21 7AW 5/7 Old Basing Mall BATH BA1 1RT 6/7 Union Street BATHGATE EH48 1PG 23 George Street BEACONSFIELD HP9 1QD 11 The Highway, Station Road BECCLES NR34 9HQ 9 New Market Place BECKENHAM BR3 1EW 172 High Street BEDFORD MK40 1TG 29/31 The Harpur Centre, Harpur -

Giants of Dawley People, Places and Events That Helped Shape Britain
Giants of Dawley People, places and events that helped shape Britain 3 Giants of Dawley People, places and events that helped shape Britain 1 Dawley Heritage Project • www.dawleyheritage.co.uk Giants of Dawley People, places and events that helped shape Britain Dawley Regeneration Partnership Bank House 66 High Street Dawley Telford TF4 2HD © The Dawley Regeneration Partnership, 2010 First published 2010 All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without the prior written permission of the Publisher. Every effort has been made to contact copyright holders of material reproduced in this book. The Publisher apologise for any omissions and will be pleased to rectify them at the earliest opportunity. Editing and production: Carol Thompson & Nigel McDonald, No Nonsense – Interpretation Design and artwork: Mike Ashton, MA Creative Printed in the UK (Creative Digital Ltd, Shrewsbury) 2 Contents Foreword by Shirley Bruneau 5 Contributing authors 6 Acknowledgements 8 Introduction 9 A Mighty Industrial Past: dominating works and momentous events Horsehay Works: ‘the best heavy engineering company in the UK’ 14 The Battle of Cinderloo: workers’ revolt in Old Park cinder hills 18 The Springwell Pit Disaster: one of the biggest local mining tragedies of its day 26 Pillars of Religious Faith: voices of conviction and demonstrations of unity Samuel Peploe: Bishop of Chester from 1726 to 1752 -

Messages Report Nov 1 Copy.Pptx
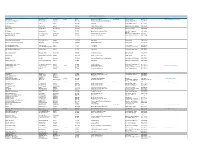
FACEBOOK Blah blah Messages etc.. ENGAGEMENT ANALYSIS CHARTS The chart in this document is collated daily by us as part of our commitment to ensure the marketing we conduct at our schemes is as social as it is effective for both the centres and their tenants. The statistics represent independent figures provided by Facebook and is based on the algorithms they run evaluating the relative performance of Pages and Posts relative to ‘Engagement’, measuring reactions, comments and shares. Messages PR harvest figures for 240 UK Shopping Centres and present them in a tabular form. We display the results in relative terms, which allows us to judge the performance of Pages when comparing the size of schemes and the number of ‘Page likes’ they enjoy. We also show the absolute positions where more Page likes, bigger budgets and boosts all work to generate increased engagement. Messages PR deliver astonishing results, regardless of how they are measured. In this vital Christmas sales period, our centres were placed within 10 of the top 20 places in relative terms and occupied the entire top 7. Even in absolute terms we placed 4 schemes in the top 10 UK Centre pages. Pentagon, Chatham was also number one in absolute terms, the best performing UK Shopping Scheme on Facebook, outperforming the mega centre Bluewater. Similarly Parkway in Middlesbrough outperformed The Metro Centre and Grays outperformed intu Lakeside by significant margins as you can see from the charts. We do not achieve these results by clever tweaking of posts, giveaways or boosts – It is because the work we undertake is genuinely social that we generate extraordinary results on social media.