Toronto N 2016
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Episode 35 - Pediatric Orthopedics - Emergencymedicinecases.Com
EPISODE 35 - PEDIATRIC ORTHOPEDICS - EMERGENCYMEDICINECASES.COM KNEE INJURIES: Check the X-ray for a Segond fracture, a vertically oriented In general, children’s ligaments are avulsion fracture off the lateral stronger than their bones, thus proximal tibia. This is highly fractures are more likely than associated with ACL and meniscal sprains. Have a low threshold for tears. (See page 4 for a picture.) imaging if suspicious. Management of ACL tears: The same ACL-injury mechanism (sudden deceleration - pain management in acute phase of distal leg with forward and (NSAIDs, tylenol, morphine) rotatory movement) will cause a - short term immobilization (splint EPISODE 35: tibial spine fracture in a as needed, +/-crutches), but PEDIATRIC ORTHOPEDICS younger child, and an ACL tear in atrophy of quadriceps occurs WITH DR. SANJAY MEHTA & a teenager or adult. (See page 4 for quickly, so start range of motion in DR. JONATHAN PIRIE a photo of a tibial spine fracture.) 2–3 days. Some experts Patellar subluxations: the child Lachman test for ACL tear recommend weight bearing as may feel a “pop”, from the kneecap involves pulling the proximal tibia tolerated immediately. subluxing, and feel unstable on the anteriorly while holding the knee in - Surgical repair is delayed until leg. First time patella dislocations flexion. It has good sensitivity (>80% range of motion has recovered. and non-displaced fractures do and specificity of 95%) (1). The Refer to outpatient orthopedics. need knee immobilization, pivot shift test (valgus force and with weight bearing as tolerated. internal rotation to extended leg, Displaced fractures or fractures with which is then flexed to feel Additional X-ray views: an impaired extensor mechanism subluxation) is also sensitive for ACL - patellar injury requires a “skyline need urgent orthopedic tear. -

Ottawa Knee Rule: Investigating Use and Application in a Tertiary Teaching Hospital
Open Access Original Article DOI: 10.7759/cureus.8812 Ottawa Knee Rule: Investigating Use and Application in a Tertiary Teaching Hospital Abubakr Mohamed 1 , Elkhidir Babikir 1 , Mohamed Kamal Elbashir Mustafa 2 1. Emergency Medicine, University Hospital Galway, Galway, IRL 2. Vascular Surgery, University Hospital Galway, Galway, IRL Corresponding author: Abubakr Mohamed, [email protected] Abstract Background Knee injuries are encountered commonly in the emergency departments (EDs) in Ireland. Validated clinical decision rules such as Ottawa knee rule (OKR) can be used in acute knee injury settings to reduce the number of unnecessary radiography. Clinical judgment can be used to distinguish between suspected fractures and non-fractures in many cases; however, radiography is still routinely requested. Objectives We evaluated the OKRs in a high-volume tertiary teaching hospital in Ireland to determine whether the rule could be safely used to decide whether patients with acute blunt knee trauma should undergo radiography. Methods This was an observational study conducted in the ED over a three-month period in a tertiary referral hospital. A total of 110 patients with acute knee injuries were examined using OKR. Inclusion criteria included patients with acute knee injuries due to blunt trauma or twisting injury and patients with lacerations or contusions. Open fractures and fractures due to penetrating injury were excluded from the study. Results Fractures were seen in 12 (13.2%) of the 110 patents who met the inclusion criteria. The OKR predicted all 12 fractures. Sensitivity was 100%, and specificity was 39%. Conclusions Received 06/04/2020 Review began 06/18/2020 The OKR is highly sensitive for fracture in this setting and can be safely used to decide whether Review ended 06/21/2020 patients with acute blunt knee trauma should undergo radiography. -

Netter's Musculoskeletal Flash Cards, 1E
Netter’s Musculoskeletal Flash Cards Jennifer Hart, PA-C, ATC Mark D. Miller, MD University of Virginia This page intentionally left blank Preface In a world dominated by electronics and gadgetry, learning from fl ash cards remains a reassuringly “tried and true” method of building knowledge. They taught us subtraction and multiplication tables when we were young, and here we use them to navigate the basics of musculoskeletal medicine. Netter illustrations are supplemented with clinical, radiographic, and arthroscopic images to review the most common musculoskeletal diseases. These cards provide the user with a steadfast tool for the very best kind of learning—that which is self directed. “Learning is not attained by chance, it must be sought for with ardor and attended to with diligence.” —Abigail Adams (1744–1818) “It’s that moment of dawning comprehension I live for!” —Calvin (Calvin and Hobbes) Jennifer Hart, PA-C, ATC Mark D. Miller, MD Netter’s Musculoskeletal Flash Cards 1600 John F. Kennedy Blvd. Ste 1800 Philadelphia, PA 19103-2899 NETTER’S MUSCULOSKELETAL FLASH CARDS ISBN: 978-1-4160-4630-1 Copyright © 2008 by Saunders, an imprint of Elsevier Inc. All rights reserved. No part of this book may be produced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording or any information storage and retrieval system, without permission in writing from the publishers. Permissions for Netter Art figures may be sought directly from Elsevier’s Health Science Licensing Department in Philadelphia PA, USA: phone 1-800-523-1649, ext. 3276 or (215) 239-3276; or e-mail [email protected]. -

Treatment of Common Hip Fractures: Evidence Report/Technology
This report is based on research conducted by the Minnesota Evidence-based Practice Center (EPC) under contract to the Agency for Healthcare Research and Quality (AHRQ), Rockville, MD (Contract No. HHSA 290 2007 10064 1). The findings and conclusions in this document are those of the authors, who are responsible for its content, and do not necessarily represent the views of AHRQ. No statement in this report should be construed as an official position of AHRQ or of the U.S. Department of Health and Human Services. The information in this report is intended to help clinicians, employers, policymakers, and others make informed decisions about the provision of health care services. This report is intended as a reference and not as a substitute for clinical judgment. This report may be used, in whole or in part, as the basis for the development of clinical practice guidelines and other quality enhancement tools, or as a basis for reimbursement and coverage policies. AHRQ or U.S. Department of Health and Human Services endorsement of such derivative products may not be stated or implied. Evidence Report/Technology Assessment Number 184 Treatment of Common Hip Fractures Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 540 Gaither Road Rockville, MD 20850 www.ahrq.gov Contract No. HHSA 290 2007 10064 1 Prepared by: Minnesota Evidence-based Practice Center, Minneapolis, Minnesota Investigators Mary Butler, Ph.D., M.B.A. Mary Forte, D.C. Robert L. Kane, M.D. Siddharth Joglekar, M.D. Susan J. Duval, Ph.D. Marc Swiontkowski, M.D. -

What Is the Best Way to Evaluate an Acute Traumatic Knee Injury?
From the CLINICAL INQUIRIES Family Physicians Inquiries Network Matthew L. Silvis, MD, C. Randall Clinch, DO, MS, What is the best way and Janine S. Tillet, MSLS Wake Forest University, to evaluate an acute Winston-Salem, NC traumatic knee injury? Evidence-based answer Use the Ottawa Knee Rules. When there or ligamentous injury (SOR: C, based on is a possibility of fracture, they can guide studies of intermediate outcomes). the use of radiography in adults who Sonographic examination of a present with isolated knee pain. However, traumatized knee can accurately detect information on use of these rules in the internal knee derangement (SOR: C, pediatric population is limited (strength based on studies of intermediate of recommendation [SOR]: A, based on outcomes). Magnetic resonance imaging systematic review of high-quality studies (MRI) of the knee is the noninvasive and a validated clinical decision rule). standard for diagnosing internal knee Specific physical examination maneuvers derangement, and it is useful for both adult (such as the Lachman and McMurray tests) and pediatric patients (SOR: C, based on FAST TRACK may be helpful when assessing for meniscal studies of intermediate outcomes). Employ the Clinical commentary Ottawa Knee Rules Ottawa rules for ankles—yes, test, Drawer sign, and McMurray test to determine but they’re good for knees, too are useful in diagnosing the presence of whether plain The evidence presented here suggests internal ligamentous injuries without MRI, x-rays are needed a number of practical and useful and an ultrasound can help to detect knee to rule out fracture approaches for the evaluation of acute effusion when it is not clinically obvious. -
EM Cases Digest Vol. 1 MSK & Trauma
THE MAGAZINE SERIES FOR ENHANCED EM LEARNING Vol. 1: MSK & Trauma Copyright © 2015 by Medicine Cases Emergency Medicine Cases by Medicine Cases is copyrighted as “All Rights Reserved”. This eBook is Creative Commons Attribution-NonCommercial- NoDerivatives 3.0 Unsupported License. Upon written request, however, we may be able to share our content with you for free in exchange for analytic data. For permission requests, write to the publisher, addressed “Attention: Permissions Coordinator,” at the address below. Medicine Cases 216 Balmoral Ave Toronto, ON, M4V 1J9 www.emergencymedicinecases.com This book has been authored with care to reflect generally accepted practices. As medicine is a rapidly changing field, new diagnostic and treatment modalities are likely to arise. It is the responsibility of the treating physician, relying on his/her experience and the knowledge of the patient, to determine the best management plan for each patient. The author(s) and publisher of this book are not responsible for errors or omissions or for any consequences from the application of the information in this book and disclaim any liability in connection with the use of this information. This book makes no guarantee with respect to the completeness or accuracy of the contents within. OUR THANKS TO... EDITORS IN CHIEF Anton Helman Taryn Lloyd PRODUCTION EDITOR Michelle Yee PRODUCTION MANAGER Garron Helman CHAPTER EDITORS Niran Argintaru Michael Misch PODCAST SUMMARY EDITORS Lucas Chartier Keerat Grewal Claire Heslop Michael Kilian PODCAST GUEST EXPERTS Andrew Arcand Natalie Mamen Brian Steinhart Mike Brzozowski Hossein Mehdian Arun Sayal Ivy Cheng Sanjay Mehta Laura Tate Walter Himmel Jonathan Pirie Rahim Valani Dave MacKinnon Jennifer Riley University of Toronto, Faculty of Medicine EM Cases is a venture of the Schwartz/ Reisman Emergency Medicine Institute. -

SOUTHWEST HEALTH SYSTEM, INC. SOUTHWEST MEDICAL GROUP CHARGEMASTER AS of 01/01/2021 CDM Code CPT Description Modifiers Fee 10040
SOUTHWEST HEALTH SYSTEM, INC. SOUTHWEST MEDICAL GROUP CHARGEMASTER AS OF 01/01/2021 CDM Code CPT Description Modifiers Fee 10040 10040 Acne surgery $147.00 10060 10060 Incision and drainage of abscess $212.00 10061 10061 Incision and drainage of abscess(multiple\complicated $422.00 10080 10080 Incision and drainage of pilonidal cyst; simple $340.00 10081 10081 Incision and drainage of pilonidal cyst; complicated $576.00 10120 10120 Incision and removal of foreign body, subcutaneous tissues; simple $225.00 10121 10121 Incision and removal of foreign body, subcutaneous tissues; complicated $513.00 10140 10140 Incision and drainage of hematoma, seroma or fluid collection $279.00 10160 10160 Puncture aspiration of abscess, hematoma, bulla, or cyst $179.00 10180 10180 Incision and drainage, complex, postoperative wound infection $594.00 11000 11000 Debridement of extensive eczematous or infected skin; up to 10% of body surface $133.00 Debridement including removal of foreign material associated with open fracture(s) 11010 11010 and/or dislocation(s); skin and subcutaneous tissues $1,085.00 Debridement including removal of foreign material associated with open fracture(s) 11011 11011 and/or dislocation(s); skin, subcutaneous tissue, muscle fascia, and muscle $996.00 Debridement including removal of foreign material associated with open fracture(s) 11012 11012 and/or dislocation(s); skin, subcutaneous tissue, muscle fascia, muscle, and bone $2,791.00 11042 11042 Debridement; skin, and subcutaneous tissue $197.00 11043 11043 Debridement; skin, -

Subacromial Decompression in the Shoulder
Subacromial Decompression Geoffrey S. Van Thiel, Matthew T. Provencher, Shane J. Nho, and Anthony A. Romeo PROCEDURE 2 22 Indications P ITFALLS ■ Impingement symptoms refractory to at least • There are numerous possible 3 months of nonoperative management causes of shoulder pain that can ■ In conjunction with arthroscopic treatment of a mimic impingement symptoms. All potential causes should be rotator cuff tear thoroughly evaluated prior to ■ Relative indication: type II or III acromion with undertaking operative treatment clinical fi ndings of impingement of isolated impingement syndrome. Examination/Imaging Subacromial Decompression PHYSICAL EXAMINATION ■ Assess the patient for Controversies • Complete shoulder examination with range of • Subacromial decompression in motion and strength the treatment of rotator cuff • Tenderness with palpation over anterolateral pathology has been continually acromion and supraspinatus debated. Prospective studies • Classic Neer sign with anterolateral shoulder have suggested that there is no difference in outcomes with and pain on forward elevation above 90° when without subacromial the greater tuberosity impacts the anterior decompression. acromion (and made worse with internal rotation) • Subacromial decompression • Positive Hawkins sign: pain with internal rotation, performed in association with a forward elevation to 90°, and adduction, which superior labrum anterior- causes impingement against the coracoacromial posterior (SLAP) repair can potentially increase ligament postoperative stiffness. ■ The impingement test is positive if the patient experiences pain relief with a subacromial injection of lidocaine. ■ Be certain to evaluate for acromioclavicular (AC) joint pathology, and keep in mind that there are several causes of shoulder pain that can mimic impingement syndrome. P ITFALLS IMAGING • Ensure that an axillary lateral ■ Standard radiographs should be ordered, view is obtained to rule out an os acromiale. -

Osteoarthritis Epidemiologicosteoarthritis and Genetic Aspects Epidemiologic and Genetic Aspects
From the Department of Orthopedics, Clinical Sciences From the DepartmentLund University, of Orthopedics, Lund, Sweden Clinical Sciences Lund University, Lund, Sweden Osteoarthritis EpidemiologicOsteoarthritis and genetic aspects Epidemiologic and genetic aspects Jonas Franklin Jonas Franklin Thesis 2010 Thesis 2010 Contact address Jonas Franklin Department of Orthopedics Akureyri University Hospital IS-600 Akureyri Iceland E-mail: [email protected] ISSN 1652-8220 ISBN 978-91-86443-87-0 Lund University, Faculty of Medicine Doctoral Dissertation Series 2010:71 Printed in Sweden Mediatryck, Lund 2010 To Hlíf Atli Egill and Jóhann Jonas Franklin 1 Contents List of papers, 2 Radiographic techniques, 17 Radiographic classification, 17 Definitions and abbreviations, 3 Statistical methods, 17 Thesis at a glance, 4 Ethics, 18 Description of contributions, 6 Data encryption and protection of the individual, 18 Introduction, 7 Symptoms and signs of osteoarthritis, 7 Summary of results of papers I-V, 19 Natural history of osteoarthritis, 8 Discussion, 24 Radiographic features of osteoarthritis, 8 Research methodology, 24 Definition of osteoarthritis, 9 Abnormal mechanical loading is a risk factor for Definition of hip fractures, 9 OA, 25 Study methodology, 9 Natural history of OA, 27 Epidemiology of osteoarthritis, 11 OA and hip fracture, 28 Epidemiology of hip fractures, 11 Conclusions, 30 Risk factors for osteoarthritis ,12 Summary, 31 Risk factors for hip fracture, 13 Populärvetenskaplig sammanfattning på Aims, 14 svenska, 33 Patients and methods, 15 Ágrip á íslensku, 35 Overview of patient/subject allocation, 15 Acknowledgements, 37 Patient identification, 15 References, 38 Populations examined, 16 2 Osteoarthritis - Epidemiologic and genetic aspects List of papers This thesis is based on the following papers: I. -

FSH Chrgmaster 12-2018
Description Q Code CPTCode Rev Code Cost Markup Flatfee Markup% Billable Billable Fee 300-399 MG/ML IODINE CONCENTRATE Q9967 Q9967 320 50.00 100.00 50.00 ABDOMINO-VAGINAL VESICAL NECK SUSPENSION, WITH OR WITHOUT ENDOSCOPIC 51845 51845 360 100.00 0.00 CONTROL (EG, STAMEY, RAZ, MODIFIED PEREYRA) ABLATION, ONE OR MORE LIVER TUMOR(S), 47382 47382 360 100.00 0.00 PERCUTANEOUS, RADIOFREQUENCY ABLATION, OPEN, OF ONE OR MORE LIVER 47381 47381 360 100.00 0.00 TUMOR(S); CRYOSURGICAL ABLATION, OPEN, OF ONE OR MORE LIVER 47380 47380 360 100.00 0.00 TUMOR(S); RADIOFREQUENCY ABRASION; EACH ADDITIONAL FOUR LESIONS OR LESS (LIST SEPARATELY IN ADDITION TO 15787 15787 360 100.00 0.00 CODE FOR PRIMARY PROCEDURE) ABRASION; SINGLE LESION (EG, KERATOSIS, 15786 15786 360 100.00 0.00 SCAR) ACETABULOPLASTY; (EG, WHITMAN, COLONNA, 27120 27120 360 100.00 0.00 HAYGROVES, OR CUP TYPE) ACETABULOPLASTY; RESECTION, FEMORAL 27122 27122 360 100.00 0.00 HEAD (EG, GIRDLESTONE PROCEDURE) ACETONE OTHER KETONE BODIES 82009 82009 301 60.00 100.00 60.00 ACROMIOPLASTY OR ACROMIONECTOMY, PARTIAL, WITH OR WITHOUT 23130 23130 360 17,250.00 100.00 17,250.00 CORACOACROMIAL LIGAMENT RELEASE ACTH 82024 82024 301 300.00 100.00 300.00 ACUTE HEPATITIS PANEL 80074 80074 300 1,210.00 100.00 1,210.00 ADAPT/EXT, PACING OR NEUROSTIMULATOR C1883-G C1883 278 700.00 0.00 LEAD IMPLANTABLE ADAPTER/EXT, PACING OR NEUROSTIMULATOR C1883-W C1883 278 100.00 0.00 LEAD IMPLANTABLE ADENOIDECTOMY, PRIMARY; AGE 12 OR OVER 42831 42831 360 8,900.00 100.00 8,900.00 ADENOIDECTOMY, PRIMARY; UNDER AGE 12 42830 42830 -

Imaging Shoulder Impingement
UCLA UCLA Previously Published Works Title Imaging shoulder impingement. Permalink https://escholarship.org/uc/item/0kg9j32r Journal Skeletal radiology, 22(8) ISSN 0364-2348 Authors Gold, RH Seeger, LL Yao, L Publication Date 1993-11-01 DOI 10.1007/bf00197135 Peer reviewed eScholarship.org Powered by the California Digital Library University of California Skeletal Radiol (1993) 22:555-561 Skeletal Radiology Review Imaging shoulder impingement Richard H. Gold, M.D., Leannc L. Seeger, M.D., Lawrence Yao, M.D. Department of Radiological Sciences, UCLA School of Medicine, 10833 Le Conte Avenue, Los Angeles, CA 90024-1721, USA Abstract. Appropriate imaging and clinical examinations more components of the coracoacromial arch superiorly. may lead to early diagnosis and treatment of the shoulder The coracoacromial arch is composed of five basic struc- impingement syndrome, thus preventing progression to a tures: the distal clavicle, acromioclavicular joint, anteri- complete tear of the rotator cuff. In this article, we discuss or third of the acromion, coracoacromial ligament, and the anatomic and pathophysiologic bases of the syn- anterior third of the coracoid process (Fig. 1). Repetitive drome, and the rationale for certain imaging tests to eval- trauma leads to progressive edema and hemorrhage of uate it. Special radiographic projections to show the the rotator cuff and hypertrophy of the synovium and supraspinatus outlet and inferior surface of the anterior subsynovial fat of the subacromial bursa. In a vicious third of the acromion, combined with magnetic reso- cycle, the resultant loss of space predisposes the soft nance images, usually provide the most useful informa- tissues to further injury, with increased pain and disabili- tion regarding the causes of impingement. -
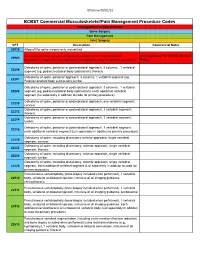
Commercial MSK Procedure Code List Effective 09.01.21.Xlsx
Effective 09/01/21 BCBST Commercial Musculoskeletal/Pain Management Procedure Codes Investigational or Non-Covered Spine Surgery Pain Management Joint Surgery CPT Description Commercial Notes 20930 Allograft for spine surgery only morselized Computer-assisted surgical navigational procedure for musculoskeletal Investigational Per BCBST Medical 20985 procedures, image-less (List separately in addition to code for primary procedure) Policy Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral 22206 segment (eg, pedicle/vertebral body subtraction); thoracic Osteotomy of spine, posterior approach, 3 columns, 1 vertebral segment (eg. 22207 Pedicle/vertebral body subtraction);lumbar Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral 22208 segment (eg, pedicle/vertebral body subtraction); each additional vertebral segment (list separately in addition to code for primary procedure) Osteotomy of spine, posterior or posterolateral approach, one vertebral segment; 22210 cervical Osteotomy of spine, posterior or posterolateral approach, 1 vertebral segment; 22212 thoracic Osteotomy of spine, posterior or posterolateral approach, 1 vertebral segment; 22214 lumbar Osteotomy of spine, posterior or posterolateral approach, 1 vertebral segment; 22216 each additional vertebral segment (List separately in addition to primary procedure) Osteotomy of spine, including discectomy anterior approach, single vertebral 22220 segment; cervical Osteotomy of spine, including discectomy, anterior approach, single