Open Latarjet: a Reliable, Successful Method to Prevent Recurrence in the Presence of Bony Defects Kevin D
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Netter's Musculoskeletal Flash Cards, 1E
Netter’s Musculoskeletal Flash Cards Jennifer Hart, PA-C, ATC Mark D. Miller, MD University of Virginia This page intentionally left blank Preface In a world dominated by electronics and gadgetry, learning from fl ash cards remains a reassuringly “tried and true” method of building knowledge. They taught us subtraction and multiplication tables when we were young, and here we use them to navigate the basics of musculoskeletal medicine. Netter illustrations are supplemented with clinical, radiographic, and arthroscopic images to review the most common musculoskeletal diseases. These cards provide the user with a steadfast tool for the very best kind of learning—that which is self directed. “Learning is not attained by chance, it must be sought for with ardor and attended to with diligence.” —Abigail Adams (1744–1818) “It’s that moment of dawning comprehension I live for!” —Calvin (Calvin and Hobbes) Jennifer Hart, PA-C, ATC Mark D. Miller, MD Netter’s Musculoskeletal Flash Cards 1600 John F. Kennedy Blvd. Ste 1800 Philadelphia, PA 19103-2899 NETTER’S MUSCULOSKELETAL FLASH CARDS ISBN: 978-1-4160-4630-1 Copyright © 2008 by Saunders, an imprint of Elsevier Inc. All rights reserved. No part of this book may be produced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording or any information storage and retrieval system, without permission in writing from the publishers. Permissions for Netter Art figures may be sought directly from Elsevier’s Health Science Licensing Department in Philadelphia PA, USA: phone 1-800-523-1649, ext. 3276 or (215) 239-3276; or e-mail [email protected]. -

Open Latarjet: Tried, Tested and True
Review Article Page 1 of 14 Open Latarjet: tried, tested and true Owen Mattern1, Allan Young1, Gilles Walch2 1Sydney Shoulder Research Institute, Sydney, Australia; 2Centre Orthopédique Santy, Lyon, France Contributions: (I) Conception and design: G Walch, A Young; (II) Administrative support: A Young; (III) Provision of study materials or patients: None; (IV) Collection and assembly of data: None; (V) Data analysis and interpretation: None; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Allan Young. Sydney Shoulder Research Institute, Suite 201, 156 Pacific Highway, St Leonards, Sydney, New South Wales 2065, Australia. Email: [email protected]. Abstract: The open Latarjet procedure has proven to be an effective procedure in the treatment of anterior shoulder instability, particularly in patients with glenoid bone loss and/or an engaging Hill-Sachs lesion. The transfer of the coracoid bone block to the anterior glenoid provides stability via the “triple blocking effect”. We describe our indications and surgical technique for the open Latarjet procedure. Keywords: Latarjet; coracoid transfer; anterior shoulder instability Received: 04 June 2017; Accepted: 18 September 2017; Published: 08 November 2017. doi: 10.21037/aoj.2017.10.01 View this article at: http://dx.doi.org/10.21037/aoj.2017.10.01 Introduction Latarjet included a lower recurrence and dislocation rate, whilst loss of external rotation was less with Latarjet of Traumatic anterior shoulder instability is a common injury 11.5° compared to 20.9° with Bankart repair (11). for the contact athlete, with high rates of recurrence in some athletic populations (1-4). Anatomical Bankart repair procedures have been successful, however high recurrence Principles rates have been shown in certain patient groups (5,6). -

Multidirectional Shoulder Instability with Bone Loss and Prior Failed
Technical Note Multidirectional Shoulder Instability With Bone Loss and Prior Failed Latarjet Procedure: Treatment With Fresh Distal Tibial Allograft and Modified T-Plasty Open Capsular Shift Liam A. Peebles, B.A., Zachary S. Aman, B.A., Fletcher R. Preuss, B.S., Brian T. Samuelsen, M.D., M.B.A., Tyler J. Zajac, M.S., A.T.C., O.T.C., Mitchell I. Kennedy, B.S., and Matthew T. Provencher, M.D., C.A.PT., M.C., U.S.N.R. Abstract: Recurrent multidirectional shoulder instability (MDI) is a challenging clinical problem, particularly in the setting of connective tissue diseases, and there is a distinct lack of literature discussing strategies for operative management of this unique patient group. These patients frequently present with significant glenoid bone loss, patulous and abnormal capsulolabral structures, and a history of multiple failed arthroscopic or open instability procedures. Although the precise treatment algorithm requires tailoring to the individual patient, we have shown successful outcomes in correcting recurrent MDI in the setting of underlying connective tissue disorders by means of a modified T-plasty capsular shift and rotator interval closure in conjunction with distal tibial allograft bony augmentation. The purpose of this Technical Note was to describe a technique that combines a fresh distal tibial allograft for glenoid bony augmentation with a modified T-plasty capsular shift and rotator interval closure for the management of recurrent shoulder MDI in patients presenting with Ehlers-Danlos syndrome or other connective tissue disorders after failed Latarjet stabilization. ecurrent multidirectional shoulder instability Conversely, MDI without hyperlaxity is more likely to R(MDI) is a difficult clinical problem and becomes present with anterior and/or posterior capsulolabral even more challenging in the face of connective tissue pathology1,2 in addition to bony lesions. -

SOUTHWEST HEALTH SYSTEM, INC. SOUTHWEST MEDICAL GROUP CHARGEMASTER AS of 01/01/2021 CDM Code CPT Description Modifiers Fee 10040
SOUTHWEST HEALTH SYSTEM, INC. SOUTHWEST MEDICAL GROUP CHARGEMASTER AS OF 01/01/2021 CDM Code CPT Description Modifiers Fee 10040 10040 Acne surgery $147.00 10060 10060 Incision and drainage of abscess $212.00 10061 10061 Incision and drainage of abscess(multiple\complicated $422.00 10080 10080 Incision and drainage of pilonidal cyst; simple $340.00 10081 10081 Incision and drainage of pilonidal cyst; complicated $576.00 10120 10120 Incision and removal of foreign body, subcutaneous tissues; simple $225.00 10121 10121 Incision and removal of foreign body, subcutaneous tissues; complicated $513.00 10140 10140 Incision and drainage of hematoma, seroma or fluid collection $279.00 10160 10160 Puncture aspiration of abscess, hematoma, bulla, or cyst $179.00 10180 10180 Incision and drainage, complex, postoperative wound infection $594.00 11000 11000 Debridement of extensive eczematous or infected skin; up to 10% of body surface $133.00 Debridement including removal of foreign material associated with open fracture(s) 11010 11010 and/or dislocation(s); skin and subcutaneous tissues $1,085.00 Debridement including removal of foreign material associated with open fracture(s) 11011 11011 and/or dislocation(s); skin, subcutaneous tissue, muscle fascia, and muscle $996.00 Debridement including removal of foreign material associated with open fracture(s) 11012 11012 and/or dislocation(s); skin, subcutaneous tissue, muscle fascia, muscle, and bone $2,791.00 11042 11042 Debridement; skin, and subcutaneous tissue $197.00 11043 11043 Debridement; skin, -
The Open Eden-Hybinette Procedure for Recurrent Anterior Shoulder Instability with Glenoid Bone Loss Joseph W
The Open Eden-Hybinette Procedure for Recurrent Anterior Shoulder Instability With Glenoid Bone Loss Joseph W. Galvin, DO,* Zachary R. Zimmer, MD,* Alexander M. Prete, BS,* and Jon J.P. Warner, MD* In the setting of significant glenoid bone loss, soft tissue stabilization procedures for recur- rent anterior shoulder instability have high failure rates. The open or arthroscopic Eden- Hybinette procedure with tricortical iliac crest autograft has been shown to provide good results with low rates of recurrent instability. Indications for this technique include severe glenoid bone loss (>40%), recurrent instability following a Latarjet or distal tibial allograft procedure, or patients with abnormal coracoid morphology. In this technique article, we review the indications, contraindications, surgical technique, postoperative care, out- comes, and complications of the open Eden-Hybinette procedure. Oper Tech Sports Med 27:95-101 © 2019 Elsevier Inc. All rights reserved. KEYWORDS Eden-Hybinette, recurrent anterior instability Introduction through advanced imaging with MRI and 3-dimensional recon- struction computed tomography (CT) scans has likely led to nterior shoulder instability is a common problem in young increased utilization of bone augmentation techniques such as A active individuals with an incidence in the United States the Latarjet procedure, distal tibial allograft (DTA), and distal 1,2 (US) general population of 0.08 per 1000 person-years. Cer- clavicular autograft.13-17 The Latarjet and DTA procedures have tain at-risk populations involved in contact and collision activi- showntobeeffectiveandprovidegoodoutcomeswithlow ties, such as American football players and military athletes, rates of recurrent instability in primary and revision instability have anterior instability at an order of magnitude greater of scenarios,18-20 with the Latarjet showing long-term durability. -

Subacromial Decompression in the Shoulder
Subacromial Decompression Geoffrey S. Van Thiel, Matthew T. Provencher, Shane J. Nho, and Anthony A. Romeo PROCEDURE 2 22 Indications P ITFALLS ■ Impingement symptoms refractory to at least • There are numerous possible 3 months of nonoperative management causes of shoulder pain that can ■ In conjunction with arthroscopic treatment of a mimic impingement symptoms. All potential causes should be rotator cuff tear thoroughly evaluated prior to ■ Relative indication: type II or III acromion with undertaking operative treatment clinical fi ndings of impingement of isolated impingement syndrome. Examination/Imaging Subacromial Decompression PHYSICAL EXAMINATION ■ Assess the patient for Controversies • Complete shoulder examination with range of • Subacromial decompression in motion and strength the treatment of rotator cuff • Tenderness with palpation over anterolateral pathology has been continually acromion and supraspinatus debated. Prospective studies • Classic Neer sign with anterolateral shoulder have suggested that there is no difference in outcomes with and pain on forward elevation above 90° when without subacromial the greater tuberosity impacts the anterior decompression. acromion (and made worse with internal rotation) • Subacromial decompression • Positive Hawkins sign: pain with internal rotation, performed in association with a forward elevation to 90°, and adduction, which superior labrum anterior- causes impingement against the coracoacromial posterior (SLAP) repair can potentially increase ligament postoperative stiffness. ■ The impingement test is positive if the patient experiences pain relief with a subacromial injection of lidocaine. ■ Be certain to evaluate for acromioclavicular (AC) joint pathology, and keep in mind that there are several causes of shoulder pain that can mimic impingement syndrome. P ITFALLS IMAGING • Ensure that an axillary lateral ■ Standard radiographs should be ordered, view is obtained to rule out an os acromiale. -

H3 Schedule of Procedures H3 Insurance Schedule of Procedures
H3 Schedule of Procedures H3 Insurance Schedule of Procedures This schedule is based on the CCSD schedule of procedures. H3 Schedule of Procedures Version 2020 All codes listed detail the maximum amount we will pay towards the fee a specialist and anaesthetist will charge for the operation/procedure. H3 Insurance is a trading name of Insure I Limited which is authorised and regulated by the Financial Conduct Authority. Insure I Ltd is registered in Northern Ireland, Registered number NI072940. H3 Insurance Registered address is Channel Wharf, 21 Old Channel Road, Belfast, BT3 9DE. T: 028 9046 9990 www.h3insurance.com H3 Schedule of Procedures Index Guidance Notes .................................................................................................................. 1 Abdomen – excluding urinary / reproductive organs......................................................... 3 Bones, joints & connective tissue / tendon muscle ......................................................... 13 Brain, cranium & other intracranial organs ...................................................................... 29 Breasts .............................................................................................................................. 32 Consultations, simple investigations & general procedures ............................................ 35 Ear, nose & throat… .......................................................................................................... 38 Endoscopic GIT procedures ............................................................................................. -

The Biomechanics of the Latarjet Reconstruction: Is It All About the Sling? Nobuyuki Yamamoto, MD,* and Scott P
The Biomechanics of the Latarjet Reconstruction: Is It All About the Sling? Nobuyuki Yamamoto, MD,* and Scott P. Steinmann, MD† It has been clinically believed that the stabilizing mechanism of the Latarjet procedure is the sling effect. Biomechanical studies have demonstrated that there are 3 stabilizing mecha- nisms of the Latarjet procedure, the main one being the sling effect produced by the sub- scapularis and conjoint tendons. The other 2 mechanisms are the suturing of the capsular flap at the end-range arm position and reconstruction of the glenoid concavity at the mid- range arm position. All 3 stabilizing mechanisms function at both the mid- and end-range arm positions. After the Latarjet procedure, the shoulder even with a large glenoid defect can have stability increased by 14% compared to the normal shoulder. The acceptable clini- cal outcomes of the Latarjet procedure are supported by these 3 stabilizing mechanisms. Oper Tech Sports Med 27:49-54 © 2019 Elsevier Inc. All rights reserved. KEYWORDS biomechanics, Latarjet reconstruction, sling, subscapularis Why Good Clinical Results Can in which the essential lesion, the Bankart lesion is not repaired? To date, “sling effect of the subscapularis muscle” Be Obtained Without the Bankart has been clinically believed as the main stabilizing mechanism Repair? of this procedure. This was speculation among surgeons. Its he Latarjet procedure has gained popularity with recent precise stabilizing mechanism had not been studied. T reports1,2 showing that postoperative arthritis can be avoided by appropriate positioning of the coracoid bone graft. Excellent clinical results even for shoulders with a large Biomechanical Experiments glenoid defect have been reported. -

2019 Orthopaedic Updates Bookle
Doctors Consulting here Dr Todd Gothelf Concord 47-49 Burwood Road Tel 02 9744 2666 Dr Samya Lakis CONCORD NSW 2137 Fax 02 9744 3706 Dr Paul Mason Dr John Negrine Dr Rodney Pattinson Dr Doron Sher Dr Kwan Yeoh Doctors Consulting here Dr Paul Annett Dr Jerome Goldberg Level 7 Dr Todd Gothelf Hurstville Waratah Private Tel 02 9580 6066 Dr Samya Lakis 29-31 Dora Street Fax 02 9580 0890 Dr Andreas Loefler HURSTVILLE NSW 2220 Dr John Negrine Dr Rodney Pattinson Dr Ivan Popoff Dr Allen Turnbull Dr Kwan Yeoh Doctors Consulting here Suite 5B Penrith Tel 02 4721 7799 Dr Todd Gothelf 119-121 Lethbridge St Fax 02 4721 7997 Dr Kwan Yeoh PENRITH NSW 2750 Doctors Consulting here Dr John Best Dr Jerome Goldberg Dr Leigh Golding Dr Todd Gothelf 160 Belmore Road Tel 02 9399 5333 Dr Samya Lakis Randwick RANDWICK NSW 2031 Fax 02 9398 8673 Dr Paul Mason Dr Andreas Loefler Dr John Negrine Dr Rodney Pattinson Dr Ivan Popoff Dr Doron Sher www.orthosports.com.au Topic Presenter Notes An approach to the stiffening painful shoulder Dr John Best Notes below Medial meniscal root tears Dr Doron Sher Notes below The first time dislocation of the shoulder Dr Jerome Goldberg Notes below Diagnosing and treating spinal pain Dr Paul Mason Rapid recovery after joint replacement Dr Andreas Loefler Case based sports medicine mimics, Dr Paul Annett rheumatology and others Lisfranc Injuries Dr Todd Gothelf International touring during a pandemic Dr Leigh Golding Vertebral body tethering (VBT): an update Dr Samya Lakis Notes below Interesting Case Studies Dr John Negrine Slipped upper femoral epiphysis Dr Rod Pattinson Dr John P Best B Med, Dip Sports Med (London), FACSP, FFSEM Sport & Exercise Medicine Physician An Approach to the Stiffening Painful Shoulder This handout complements the video presentation on this topic. -

FSH Chrgmaster 12-2018
Description Q Code CPTCode Rev Code Cost Markup Flatfee Markup% Billable Billable Fee 300-399 MG/ML IODINE CONCENTRATE Q9967 Q9967 320 50.00 100.00 50.00 ABDOMINO-VAGINAL VESICAL NECK SUSPENSION, WITH OR WITHOUT ENDOSCOPIC 51845 51845 360 100.00 0.00 CONTROL (EG, STAMEY, RAZ, MODIFIED PEREYRA) ABLATION, ONE OR MORE LIVER TUMOR(S), 47382 47382 360 100.00 0.00 PERCUTANEOUS, RADIOFREQUENCY ABLATION, OPEN, OF ONE OR MORE LIVER 47381 47381 360 100.00 0.00 TUMOR(S); CRYOSURGICAL ABLATION, OPEN, OF ONE OR MORE LIVER 47380 47380 360 100.00 0.00 TUMOR(S); RADIOFREQUENCY ABRASION; EACH ADDITIONAL FOUR LESIONS OR LESS (LIST SEPARATELY IN ADDITION TO 15787 15787 360 100.00 0.00 CODE FOR PRIMARY PROCEDURE) ABRASION; SINGLE LESION (EG, KERATOSIS, 15786 15786 360 100.00 0.00 SCAR) ACETABULOPLASTY; (EG, WHITMAN, COLONNA, 27120 27120 360 100.00 0.00 HAYGROVES, OR CUP TYPE) ACETABULOPLASTY; RESECTION, FEMORAL 27122 27122 360 100.00 0.00 HEAD (EG, GIRDLESTONE PROCEDURE) ACETONE OTHER KETONE BODIES 82009 82009 301 60.00 100.00 60.00 ACROMIOPLASTY OR ACROMIONECTOMY, PARTIAL, WITH OR WITHOUT 23130 23130 360 17,250.00 100.00 17,250.00 CORACOACROMIAL LIGAMENT RELEASE ACTH 82024 82024 301 300.00 100.00 300.00 ACUTE HEPATITIS PANEL 80074 80074 300 1,210.00 100.00 1,210.00 ADAPT/EXT, PACING OR NEUROSTIMULATOR C1883-G C1883 278 700.00 0.00 LEAD IMPLANTABLE ADAPTER/EXT, PACING OR NEUROSTIMULATOR C1883-W C1883 278 100.00 0.00 LEAD IMPLANTABLE ADENOIDECTOMY, PRIMARY; AGE 12 OR OVER 42831 42831 360 8,900.00 100.00 8,900.00 ADENOIDECTOMY, PRIMARY; UNDER AGE 12 42830 42830 -

Imaging Shoulder Impingement
UCLA UCLA Previously Published Works Title Imaging shoulder impingement. Permalink https://escholarship.org/uc/item/0kg9j32r Journal Skeletal radiology, 22(8) ISSN 0364-2348 Authors Gold, RH Seeger, LL Yao, L Publication Date 1993-11-01 DOI 10.1007/bf00197135 Peer reviewed eScholarship.org Powered by the California Digital Library University of California Skeletal Radiol (1993) 22:555-561 Skeletal Radiology Review Imaging shoulder impingement Richard H. Gold, M.D., Leannc L. Seeger, M.D., Lawrence Yao, M.D. Department of Radiological Sciences, UCLA School of Medicine, 10833 Le Conte Avenue, Los Angeles, CA 90024-1721, USA Abstract. Appropriate imaging and clinical examinations more components of the coracoacromial arch superiorly. may lead to early diagnosis and treatment of the shoulder The coracoacromial arch is composed of five basic struc- impingement syndrome, thus preventing progression to a tures: the distal clavicle, acromioclavicular joint, anteri- complete tear of the rotator cuff. In this article, we discuss or third of the acromion, coracoacromial ligament, and the anatomic and pathophysiologic bases of the syn- anterior third of the coracoid process (Fig. 1). Repetitive drome, and the rationale for certain imaging tests to eval- trauma leads to progressive edema and hemorrhage of uate it. Special radiographic projections to show the the rotator cuff and hypertrophy of the synovium and supraspinatus outlet and inferior surface of the anterior subsynovial fat of the subacromial bursa. In a vicious third of the acromion, combined with magnetic reso- cycle, the resultant loss of space predisposes the soft nance images, usually provide the most useful informa- tissues to further injury, with increased pain and disabili- tion regarding the causes of impingement. -
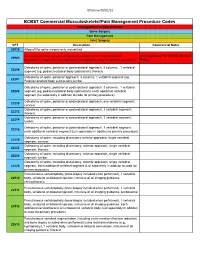
Commercial MSK Procedure Code List Effective 09.01.21.Xlsx
Effective 09/01/21 BCBST Commercial Musculoskeletal/Pain Management Procedure Codes Investigational or Non-Covered Spine Surgery Pain Management Joint Surgery CPT Description Commercial Notes 20930 Allograft for spine surgery only morselized Computer-assisted surgical navigational procedure for musculoskeletal Investigational Per BCBST Medical 20985 procedures, image-less (List separately in addition to code for primary procedure) Policy Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral 22206 segment (eg, pedicle/vertebral body subtraction); thoracic Osteotomy of spine, posterior approach, 3 columns, 1 vertebral segment (eg. 22207 Pedicle/vertebral body subtraction);lumbar Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral 22208 segment (eg, pedicle/vertebral body subtraction); each additional vertebral segment (list separately in addition to code for primary procedure) Osteotomy of spine, posterior or posterolateral approach, one vertebral segment; 22210 cervical Osteotomy of spine, posterior or posterolateral approach, 1 vertebral segment; 22212 thoracic Osteotomy of spine, posterior or posterolateral approach, 1 vertebral segment; 22214 lumbar Osteotomy of spine, posterior or posterolateral approach, 1 vertebral segment; 22216 each additional vertebral segment (List separately in addition to primary procedure) Osteotomy of spine, including discectomy anterior approach, single vertebral 22220 segment; cervical Osteotomy of spine, including discectomy, anterior approach, single