CDC and the Smallpox Crusade
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
History and Epidemiology of Global Smallpox Eradication Smallpox
History and Epidemiology of Global Smallpox Eradication Smallpox Three Egyptian Mummies 1570-1085 BC Ramses the Vth Died 1157 BC Early Written Description of Smallpox India 400 AD “Severe pain is felt in the large and small joints, with cough, shaking, listlessness and langour; the palate, lips, and tongue are dry with thirst and no appetite. The pustules are red, yellow, and white and they are accompanied by burning pain. The form soon ripens …the body has a blue color and seems studded with rice. The pustules become black and flat, are depressed in the centre, with much pain.” Smallpox and History • In the Elephant war in Mecca 568 AD, smallpox decimated the Ethiopian soldiers • Introduction of smallpox into the new world (Carribean 1507, Mexico 1520, Peru 1524, and Brazil 1555 ) facilitated Spanish conquest • Smallpox destroys Hottentots (1713) • In 1738, smallpox killed half the Cherokee Indian population • Smallpox disrupted colonial army in 1776 Smallpox Control Strategies • Smallpox hospitals (Japan 982 AD). • Variolation 10th Century. • Quarantine 1650s. • Home isolation of smallpox in Virginia 1667. • Inoculation and isolation (Haygarth 1793). • Jenner and widespread practice of vaccination throughout Europe and rest of the world. • Mass vaccination. • Surveillance containment. Variolation Inoculation with Smallpox Pus • Observations: – Pocked marked persons never affected with smallpox – Persons inoculated with smallpox pustular fluid or dried scabs usually had milder disease • Not ideal control strategy – Case fatality rate still 2% – Can transmit disease to others during illness The 1st Smallpox Vaccination Jenner 1796 Cowpox lesions on the hand of Sarah Nelmes (case XVI in Jenner’s Inquiry), from which material was taken for the vaccination of James Phipps below in 1796 History of Smallpox Vaccination 1805 Growth of virus on the flank of a calf in Italy. -

J. Michael Mcginnis, Md, Ma, Mpp
J. MICHAEL MCGINNIS, MD, MA, MPP National Academy of Medicine, the National Academies, 500 Fifth Street NW, Washington DC 20001, (202) 334-3963, [email protected] Highlights: Michael McGinnis is a physician and epidemiologist who lives and works in Washington DC. Through his writing, government service, and work in philanthropy, he has been a long-time contributor to national and international field leadership in health, health care, and health policy. He currently serves at the National Academy of Medicine (NAM), where he is the Leonard D. Schaeffer Executive Officer, Senior Scholar, and Executive Director of the NAM’s Leadership Consortium for public and private collaboration on behalf of a continuously learning health system. Previously, he served as founding Director, respectively, of the Robert Wood Johnson Foundation’s (RWJF) Health Group, the World Health Organization’s Office for Health Reconstruction in Bosnia, the federal Office of Research Integrity (interim), and the federal Office of Disease Prevention and Health Promotion. In a tenure unusual for political and policy posts, he held continuous appointment through the Carter, Reagan, Bush and Clinton Administrations at the Department of Health and Human Services, with policy responsibilities for disease prevention and health promotion (1977-1995). Programs and policies conceived and launched at his initiative include the Healthy People process establishing national health goals and objectives (1979-present), the U.S. Preventive Services Task Force (1984-present), the Dietary Guidelines for Americans (with USDA, 1980- present), the multi-level Public Health Functions Steering Group and the Ten Essential Services of Public Health (1994-present), the RWJF Active Living family of programs (2000-present), the RWJF Young Epidemiology Scholars Program (2001-2012), the RWJF Health and Society Scholars Program (2002-2017), and the current Learning Health System initiative of the NAM. -

Emerging Global Epidemiology of Measles and Public Health Response to Confirmed Case in Rhode Island
PUBLIC HEALTH Emerging Global Epidemiology of Measles and Public Health Response to Confirmed Case in Rhode Island ANANDA SANKAR BANDYOPADHYAY, MBBS, MPH; UTPALA BANDY, MD ABSTRACT Organization (WHO) geographical Region of the Americas Measles is a highly contagious viral disease and rapid achieved measles elimination by interrupting transmission identification and control of cases/outbreaks are import- of the endemic strain of measles virus.3 However, importa- ant global health priorities. Measles was declared elimi- tions from endemic countries continued throughout the last nated from the United States in March 2000. However, decade and a median of 56 cases of measles were reported in importations from endemic countries continued through the United States during the 2001-2008 period.4 A major re- out the last decade and in 2011, the United States report- surgence of measles occurred in the WHO European Region ed its highest number of cases in 15 years. With a global in 2011, with more than 13,000 laboratory-confirmed cases, snapshot of current measles epidemiology and the per- nearly three times higher than the total number of laborato- sistent risk of transnational spread based on population ry-confirmed cases reported in 2010.5 Ninety percent of the movement as the backdrop, this article describes the measles cases reported from the WHO European Region in rare event of a measles case identification in the state 2011 had not been vaccinated or had no documentation of of Rhode Island and the corresponding public health prior vaccination.6 Two-hundred and sixteen laboratory-con- response. As the global effort for measles elimination firmed cases were reported in the United States in 2011, the continues to make significant progress, sensitive public highest number of cases since 1996.7 Rhode Island reported health surveillance systems and strong routine immuni- its first case of measles since 1996 in April 2011. -

Federal Register/Vol. 84, No. 151/Tuesday, August 6, 2019/Notices
38264 Federal Register / Vol. 84, No. 151 / Tuesday, August 6, 2019 / Notices IHS or pass-through entity all violations (301) 594–0899, Email: Paul.Gettys@ activities in the Epidemiology Program of federal criminal law involving fraud, ihs.gov. for American Indian/Alaska Native (AI/ bribery, or gratuity violations AN) Tribes and Urban Indian VIII. Other Information potentially affecting the federal award. communities. This program is funded Submission is required for all The Public Health Service strongly by the Office of the Assistant Secretary, applicants and recipients, in writing, to encourages all grant, cooperative HHS, is authorized under the statutory the IHS and to the HHS Office of agreement and contract recipients to earmark for minority AIDS prevention Inspector General all information provide a smoke-free workplace and and treatment activities, and is to be related to violations of federal criminal promote the non-use of all tobacco carried out pursuant to Title III of the law involving fraud, bribery, or gratuity products. In addition, Public Law 103– Public Service Act. The funding is being violations potentially affecting the 227, the Pro-Children Act of 1994, made available through an intra- federal award. 45 CFR 75.113. prohibits smoking in certain facilities Departmental Delegation of Authority Disclosures must be sent in writing to: (or in some cases, any portion of the (IDDA) to award specific funding for U.S. Department of Health and Human facility) in which regular or routine fiscal year (FY) 2019. This program is Services, Indian Health Service, education, library, day care, health care, described in the Assistance Listings Division of Grants Management, ATTN: or early childhood development located at https://beta.sam.gov (formerly Mr. -

(ITFDE) October 22, 2019
Summary of the Thirtieth Meeting of the International Task Force for Disease Eradication (ITFDE) October 22, 2019 The 30th Meeting of the International Task Force for Disease Eradication (ITFDE) was convened at The Carter Center in Atlanta, GA, USA from 8:30 am to 5:00 pm on October 22, 2019 to discuss the potential for eradication of measles and rubella. The Task Force members are Dr. Stephen Blount, The Carter Center (Chair); Dr. Peter Figueroa, The University of the West Indies, Jamaica; Dr. Donald Hopkins, The Carter Center; Dr. Fernando Lavadenz, The World Bank; Dr. Mwelecele Malecela, World Health Organization (WHO); Professor David Molyneux, Liverpool School of Tropical Medicine; Dr. Ana Morice, Independent Consultant; Dr. Stefan Peterson, UNICEF; Dr. David Ross, The Task Force for Global Health; Dr. William Schluter, Centers for Disease Control and Prevention (CDC); Dr. Nilanthi de Silva, University of Kelaniya, Sri Lanka/WHO Strategic and Technical Advisory Group for Neglected Tropical Diseases (STAG-NTDs); Dr. Dean Sienko, The Carter Center; Dr. Laurence Slutsker, PATH; Dr. Jordan Tappero, Bill & Melinda Gates Foundation; Dr. Ricardo Thompson, National Institute of Health (Mozambique); and Dr. Dyann Wirth, Harvard School of Public Health. Eleven Task Force members (Blount, Figueroa, Hopkins, Morice, Ross, Sienko, de Silva, Slutsker, Tappero, Thompson, Wirth) participated in this meeting; three were represented by an alternate (Drs. Fatima Barry for Lavadenz, Steve Cochi for Schluter, Yodit Sahlemariam for Peterson). Presenters included Drs. Sunil Bahl, WHO/SEARO; Amanda Cohn, CDC; Matthew Hanson, Bill & Melinda Gates Foundation; Alan Hinman, The Task Force for Global Health; Mark Jit, London School of Tropical Medicine & Hygiene; Ann Lindstrand, WHO/Geneva; Balcha Masresha, WHO/AFRO; Patrick O’Connor, WHO/Europe; and Desiree Pastor, Pan American Health Organization (WHO/PAHO). -

THE SURGEON GENERAL and the BULLY PULPIT Michael Stobbe a Dissertation Submitted to the Faculty of the University of North Carol
THE SURGEON GENERAL AND THE BULLY PULPIT Michael Stobbe A dissertation submitted to the faculty of the University of North Carolina at Chapel Hill in partial fulfillment of the requirements for the degree of Doctor of Public Health in the Department of Health Policy and Administration, School of Public Health Chapel Hill 2008 Approved by: Ned Brooks Jonathan Oberlander Tom Ricketts Karl Stark Bryan Weiner ABSTRACT MIKE STOBBE: The Surgeon General and the Bully Pulpit (Under the direction of Ned Brooks) This project looks at the role of the U.S. Surgeon General in influencing public opinion and public health policy. I examined historical changes in the administrative powers of the Surgeon General, to explain what factors affect how a Surgeon General utilizes the office’s “bully pulpit,” and assess changes in the political environment and in who oversees the Surgeon General that may affect the Surgeon General’s future ability to influence public opinion and health. This research involved collecting and analyzing the opinions of journalists and key informants such as current and former government health officials. I also studied public documents, transcripts of earlier interviews and other materials. ii TABLE OF CONTENTS LIST OF TABLES.................................................................................................................v Chapter 1. INTRODUCTION ...............................................................................................1 Background/Overview .........................................................................................1 -

Measles: Chapter 7.1 Chapter 7: Measles Paul A
VPD Surveillance Manual 7 Measles: Chapter 7.1 Chapter 7: Measles Paul A. Gastanaduy, MD, MPH; Susan B. Redd; Nakia S. Clemmons, MPH; Adria D. Lee, MSPH; Carole J. Hickman, PhD; Paul A. Rota, PhD; Manisha Patel, MD, MS I. Disease Description Measles is an acute viral illness caused by a virus in the family paramyxovirus, genus Morbillivirus. Measles is characterized by a prodrome of fever (as high as 105°F) and malaise, cough, coryza, and conjunctivitis, followed by a maculopapular rash.1 The rash spreads from head to trunk to lower extremities. Measles is usually a mild or moderately severe illness. However, measles can result in complications such as pneumonia, encephalitis, and death. Approximately one case of encephalitis2 and two to three deaths may occur for every 1,000 reported measles cases.3 One rare long-term sequelae of measles virus infection is subacute sclerosing panencephalitis (SSPE), a fatal disease of the central nervous system that generally develops 7–10 years after infection. Among persons who contracted measles during the resurgence in the United States (U.S.) in 1989–1991, the risk of SSPE was estimated to be 7–11 cases/100,000 cases of measles.4 The risk of developing SSPE may be higher when measles occurs prior to the second year of life.4 The average incubation period for measles is 11–12 days,5 and the average interval between exposure and rash onset is 14 days, with a range of 7–21 days.1, 6 Persons with measles are usually considered infectious from four days before until four days after onset of rash with the rash onset being considered as day zero. -

THE SURGEON GENERAL and the BULLY PULPIT Michael Stobbe a Dissertation Submitted to the Faculty of the University of North Carol
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Carolina Digital Repository THE SURGEON GENERAL AND THE BULLY PULPIT Michael Stobbe A dissertation submitted to the faculty of the University of North Carolina at Chapel Hill in partial fulfillment of the requirements for the degree of Doctor of Public Health in the Department of Health Policy and Administration, School of Public Health Chapel Hill 2008 Approved by: Ned Brooks Jonathan Oberlander Tom Ricketts Karl Stark Bryan Weiner ABSTRACT MIKE STOBBE: The Surgeon General and the Bully Pulpit (Under the direction of Ned Brooks) This project looks at the role of the U.S. Surgeon General in influencing public opinion and public health policy. I examined historical changes in the administrative powers of the Surgeon General, to explain what factors affect how a Surgeon General utilizes the office’s “bully pulpit,” and assess changes in the political environment and in who oversees the Surgeon General that may affect the Surgeon General’s future ability to influence public opinion and health. This research involved collecting and analyzing the opinions of journalists and key informants such as current and former government health officials. I also studied public documents, transcripts of earlier interviews and other materials. ii TABLE OF CONTENTS LIST OF TABLES.................................................................................................................v Chapter 1. INTRODUCTION ...............................................................................................1 -
Module on Best Practices for Measles Surveillance
WHO/V&B/01.43 ORIGINAL: ENGLISH DISTR.: GENERAL Module on best practices for measles surveillance Written by Dalya Guris, MD, MPH National Immunization Program Centers for Disease Control and Prevention, USA DEPARTMENT OF VACCINES AND BIOLOGICALS World Health Organization Geneva 2001 The Department of Vaccines and Biologicals thanks the donors whose unspecified financial support has made the production of this document possible. This document was produced by the Vaccine Assessment and Monitoring team of the Department of Vaccines and Biologicals Ordering code: WHO/V&B/01.43 Printed: March 2002 This document is available on the Internet at: www.who.int/vaccines-documents/ Copies may be requested from: World Health Organization Department of Vaccines and Biologicals CH-1211 Geneva 27, Switzerland • Fax: + 41 22 791 4227 • Email: [email protected] • © World Health Organization 2001 This document is not a formal publication of the World Health Organization (WHO), and all rights are reserved by the Organization. The document may, however, be freely reviewed, abstracted, reproduced and translated, in part or in whole, but not for sale nor for use in conjunction with commercial purposes. The views expressed in documents by named authors are solely the responsibility of those authors. ii Contents Glossary ............................................................................................................................. v Introduction ....................................................................................................................1 -

The Life and Death of Smallpox Ian and Jenifer Glynn Frontmatter More Information
Cambridge University Press 0521845424 - The Life and Death of Smallpox Ian and Jenifer Glynn Frontmatter More information The Life and Death of Smallpox This is an engaging and fascinating story of a conditional human success story. Smallpox has been one of the most devastating scourges of humanity throughout recorded history, and it is the only human illness to have been eradicated, though polio may soon follow it to official extinction through human agency. However, while smallpox is officially extinct in nature, our fears that stocks of smallpox virus may return as a weapon of bioterrorists have led to the stockpiling of vaccine, and continuing vigilance, even though the official victory over smallpox is now 15 years old. The Life and Death of Smallpox presents the entire engaging history of our struggle and ultimate (?) victory over one of our oldest and worst enemies. The story of the campaign to track down and eradicate the virus, throughout the world – the difficulties, setbacks, and the challenges successfully met – is a highlight of a fascinating book, but we cannot be confident of the ending. The final chapter of the book clearly and authoritatively explains the current status of the threat from the deliberate release of smallpox or other potential agents of biological terrorism. Ian Glynn is Professor Emeritus of Physiology at Cambridge University and Fellow of Trinity College. He is the author of An Anatomy of Thought (1999). Jenifer Glynn is a Cambridge historian and author of Tidings From Zion (2000). © Cambridge University Press www.cambridge.org Cambridge University Press 0521845424 - The Life and Death of Smallpox Ian and Jenifer Glynn Frontmatter More information The Life and Death of Smallpox IAN AND JENIFER GLYNN © Cambridge University Press www.cambridge.org Cambridge University Press 0521845424 - The Life and Death of Smallpox Ian and Jenifer Glynn Frontmatter More information PUBLISHED BY CAMBRIDGE UNIVERSITY PRESS 40 We s t 20th Street, New York, NY 10011-4211, USA http://www.cambridge.org c Ian and Jenifer Glynn 2004 This book is in copyright. -
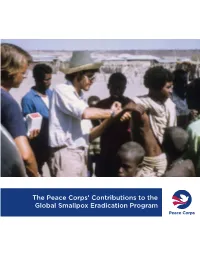
The Peace Corps' Contributions to the Global Smallpox Eradication Program
The Peace Corps’ Contributions to the Global Smallpox Eradication Program About the Office of Strategic Information, Research, and Planning (OSIRP) It is the mission of OSIRP to advance evidence-based management at the Peace Corps by guiding agency strategic planning; monitoring and evaluating agency-level performance and programs; conducting research to generate new insights in the fields of international development, cultural exchange, and Volunteer service; enhancing the stewardship and governance of agency data; and helping to shape agency engagement on high-level, governmentwide initiatives. Front Cover: Peace Corps Volunteers Robert Steinglass and Doug Arbuckle administering the smallpox vaccine in Mille, Ethiopia, in 1974. Photo: Steinglass, personal collection. ii Dedication This report is dedicated to the memory of Dr. Donald Ainslie “D. A.” Henderson (September 7, 1928—August 19, 2016), a seminal figure in the field of smallpox eradication. The Peace Corps is deeply appreciative of having had the opportunity to correspond with Dr. Henderson about the contributions of Peace Corps Volunteers and returned Volunteers within the context of the global eradication program. His charismatic leadership, tireless energy, and unflagging devotion to this program inspired countless public health workers around the world, including many of the returned Peace Corps Volunteers interviewed for this report. iii Acknowledgments In 1806, approximately 10 years after Dr. Edward Jenner conducted the first documented experiment with smallpox vaccination, laying the foundations of modern medicine, President Thomas Jefferson wrote to the English physician and scientist. Jefferson acknowledged the importance of this discovery, extending “a portion of the tribute of gratitude due to you from the whole human family. -

Gerald R. Ford Administration White House Press Releases
MARCq 24, 1976 '-. Office of the White House Press Secretary ~ NOTICE TO THE PRESS Participants in the 3:30 p. m. ~eeting with Secretary Mathews and the President: Eugene W. Fowinkle, H.D., Commissioner of Public Health, Tennessee Department of Public Health, Nashville. George Hardy, M.D., Health Officer, Jefferson County Health Department, Birmingham, Alabama. Albert G. Randell, M.D., Director of Public Health, City of Houston, Texas. Charles Hall, M.D., Charleston, West Virginia. Merritt B. Lowe, M.D., Greenfield, Massachusetts. Raymond Holden, M.D., Washington, D.C., chairman, A.M.A. Morton S. Hilbert, MPH, CE, Chairman, Department of Enviro,nmental and Industrial Health, School of Public Health, University of Michigan, Ann Arbor. Maurice R. Hilleman, Ph.D., Vice President, Merck, Sharp and Dohme Research Laboratories, West Point, PAD John F. Lawlis, Ph.D., Vice President of Biological Operations, Menell-National Laboratories, Swiftwater, PAD Eugene A. Timm, Ph.D., Asst. Division Director, Quality Control and Government Regulations, Parke, Davis and Company, Detroit, Michigan. Alan Gray, Ph.D., Director of Biologics, Merck, Sharp and Dohme, West Point, PAD Alan Bernstein, Ph.D., Managing Director, Wyeth Laboratories, Inc., Marietta, Pennsylvania. Dr. Fred M. Davenport, Department of Epidemiology, University of Michigan School of Public Health, Ann Arbor. Reul A. Stallones, M.D., Dean, University of Texas School of Public Health, Houston. Dr. Floyd Denny, University of North Carolina Department of Pediatrics, Chapel Hill. Edwin Kilbourne, M.D., Chairman, Department of Microbiology, Mt. Sinai School of Medicine, City University of New York. Saul Krugman, M.D., Department of Pediatrics, New York University School of Medicine.