TIBIOTALOCALCANEAL ARTHRODESIS George E. Quill, Jr
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Skier Tibia (Leg) Fractures
Skier Tibia (Leg) Fractures In years past, the prototypical ski fracture was sustained at the lower part of the outside of the leg in the region of the ankle. However, in the past 10 years, with the advent of the modern ski boots and improvements in binding, the most commonly seen lower leg skier fracture is the tibia (or shinbone) fracture. 10% of these fractures are associated with a collision. Thus, 90 % are associated with an isolated fall or noncontact type of injury, which is generally the result of binding malfunctions and inappropriate release. The most common mechanism leading to a tibia (leg) fracture is a forward fall. Risk factors for sustaining a skier tibia fracture include: beginners or novice skiers, less than 20 years of age, higher outdoor temperatures, and increased snow depth. Non-risk factors include ski lengths, icy conditions, and male versus female sex. The modern ski boot very closely resembles an extremely well padded short leg cast in the treatment of many orthopaedic lower extremity fractures. It of course goes to a much higher level than the former shorter boot top-level varieties. The binding release and designs have been based on the fracture strength of the adult tibia (shin) bone at the top of the modern ski boot. The treatment of most skier leg fractures includes a closed reduction and cast application for variable periods of time, with or without weight bearing allowed. However, severe misalignments of the bones can lead to later bony prominences that may be incompatible with snug, rigid, high fitting ski boots. -

Assessment, Management and Decision Making in the Treatment Of
Pediatric Ankle Fractures Anthony I. Riccio, MD Texas Scottish Rite Hospital for Children Update 07/2016 Pediatric Ankle Fractures The Ankle is the 2nd most Common Site of Physeal Injury in Children 10-25% of all Physeal Injuries Occur About the Ankle Pediatric Ankle Fractures Primary Concerns Are: • Anatomic Restoration of Articular Surface • Restoration of Symmetric Ankle Mortise • Preservation of Physeal Growth • Minimize Iatrogenic Physeal Injury • Avoid Fixation Across Physis in Younger Children Salter Harris Classification Prognosis and Treatment of Pediatric Ankle Fractures is Often Dictated by the Salter Harris Classification of Physeal Fractures Type I and II Fractures: Often Amenable to Closed Tx / Lower Risk of Physeal Arrest Type III and IV: More Likely to Require Operative Tx / Higher Risk of Physeal Arrest Herring JA, ed. Tachdjian’s Pediatric Orthopaedics, 5th Ed. 2014. Elsevier. Philadelphia, PA. ISOLATED DISTAL FIBULA FRACTURES Distal Fibula Fractures • The Physis is Weaker than the Lateral Ankle Ligaments – Children Often Fracture the Distal Fibula but…. – …ligamentous Injuries are Not Uncommon • Mechanism of Injury = Inversion of a Supinated Foot • SH I and II Fractures are Most Common – SH I Fractures: Average Age = 10 Years – SH II Fractures: Average Age = 12 Years Distal Fibula Fractures Lateral Ankle Tenderness SH I Distal Fibula Fracture vs. Lateral Ligamentous Injury (Sprain) Distal Fibula Fractures • Sankar et al (JPO 2008) – 37 Children – All with Open Physes, Lateral Ankle Tenderness + Normal Films – 18%: Periosteal -
Validation of a Clinical Prediction Rule for the Differentiation Between Septic Arthritis and Transient Synovitis of the Hip in Children by MININDER S
COPYRIGHT © 2004 BY THE JOURNAL OF BONE AND JOINT SURGERY, INCORPORATED Validation of a Clinical Prediction Rule for the Differentiation Between Septic Arthritis and Transient Synovitis of the Hip in Children BY MININDER S. KOCHER, MD, MPH, RAHUL MANDIGA, BS, DAVID ZURAKOWSKI, PHD, CAROL BARNEWOLT, MD, AND JAMES R. KASSER, MD Investigation performed at the Departments of Orthopaedic Surgery, Biostatistics, and Radiology, Children’s Hospital, Boston, Massachusetts Background: The differentiation between septic arthritis and transient synovitis of the hip in children can be difficult. The purpose of the present study was to validate a previously published clinical prediction rule for this differentiation in a new patient population. Methods: We prospectively studied children who presented to a major children’s hospital between 1997 and 2002 with an acutely irritable hip. As in the previous study, diagnoses of septic arthritis (fifty-one patients) and transient synovitis (103 patients) were operationally defined on the basis of the white blood-cell count in the joint fluid, the re- sults of cultures of joint fluid and blood, and the clinical course. Univariate analysis and multiple logistic regression were used to compare the two groups. The predicted probability of septic arthritis of the hip from the prediction rule was compared with actual distributions in the current patient population. The area under the receiver operating char- acteristic curve was determined. Results: The same four independent predictors of septic arthritis of the hip (a history of fever, non-weight-bearing, an erythrocyte sedimentation rate of 40 mm/hr, and a serum white blood-cell count of >12,000 cells/mm3 (>12.0 × 109/L)) were identified in the current patient population. -

114.3 Cmr: Division of Health Care Finance and Policy Ambulatory Care
114.3 CMR: DIVISION OF HEALTH CARE FINANCE AND POLICY AMBULATORY CARE 114.3 CMR 40.00: RATES FOR SERVICES UNDER M.G.L. c. 152, WORKERS’ COMPENSATION ACT Section 40.01: General Provisions 40.02: General Definitions 40.03: Service and Rate Coverage Provisions 40.04: Provisions Affecting Eligible Providers 40.05: Policies for Individual Service Types 40.06: Fees 40.07: Appendices 40.08: Severability 40.01: General Provisions (1) Scope, Purpose and Effective Date. 114.3 CMR 40.00 governs the payment rates effective April 1, 2009 for purchasers of health care services under M.G.L. c. 152, the Workers’ Compensation Act. Payment rates for services provided by hospitals are set forth in 114.1 CMR 41.00. Program policies relating to medical necessity and clinical appropriateness are determined pursuant to M.G.L. c. 152 and 452 CMR 6.00. (2) Coverage. The payment rates set forth in 114.3 CMR 40.06 are full payment for services provided under M.G.L. c. 152, § 13, including any related administrative or overhead costs. The insurer, employer and health care service provider may agree upon a different payment rate for any service set forth in the fee schedule in 114.3 CMR 40.00. No employee may be held liable for the payment for health care services determined compensable under M.G.L. c. 152, § 13. (3) Administrative Bulletins. The Division may issue administrative bulletins to clarify substantive provisions of 114.3 CMR 40.00, or to publish procedure code updates and corrections. For coding updates and correction, the bulletin will list: (a) new code numbers for existing codes, with the corresponding cross references between existing and new codes numbers; (b) deleted codes for which there are no corresponding new codes; and (c) codes for entirely new services that require pricing. -

Knee Joint Surgery: Open Synovectomy
Musculoskeletal Surgical Services: Open Surgical Procedures; Knee Joint Surgery: Open Synovectomy POLICY INITIATED: 06/30/2019 MOST RECENT REVIEW: 06/30/2019 POLICY # HH-5588 Overview Statement The purpose of these clinical guidelines is to assist healthcare professionals in selecting the medical service that may be appropriate and supported by evidence to improve patient outcomes. These clinical guidelines neither preempt clinical judgment of trained professionals nor advise anyone on how to practice medicine. The healthcare professionals are responsible for all clinical decisions based on their assessment. These clinical guidelines do not provide authorization, certification, explanation of benefits, or guarantee of payment, nor do they substitute for, or constitute, medical advice. Federal and State law, as well as member benefit contract language, including definitions and specific contract provisions/exclusions, take precedence over clinical guidelines and must be considered first when determining eligibility for coverage. All final determinations on coverage and payment are the responsibility of the health plan. Nothing contained within this document can be interpreted to mean otherwise. Medical information is constantly evolving, and HealthHelp reserves the right to review and update these clinical guidelines periodically. No part of this publication may be reproduced, stored in a retrieval system or transmitted, in any form or by any means, electronic, mechanical, photocopying, or otherwise, without permission from HealthHelp. -

Realignment Surgery As Alternative Treatment of Varus and Valgus Ankle Osteoarthritis
CLINICAL ORTHOPAEDICS AND RELATED RESEARCH Number 462, pp. 156–168 © 2007 Lippincott Williams & Wilkins Realignment Surgery as Alternative Treatment of Varus and Valgus Ankle Osteoarthritis Geert I. Pagenstert, MD*; Beat Hintermann, MD*; Alexej Barg, MD*; André Leumann, MD†; and Victor Valderrabano, MD, PhD† In patients with asymmetric (varus or valgus) ankle osteo- Level of Evidence: Level IV, therapeutic study. See the arthritis, realignment surgery is an alternative treatment to Guidelines for Authors for a complete description of levels of fusion or total ankle replacement in selected cases. To deter- evidence. mine whether realignment surgery in asymmetric ankle os- teoarthritis relieved pain and improved function, we clini- cally and radiographically followed 35 consecutive patients Surgical treatment for patients with symptomatic ankle with posttraumatic ankle osteoarthritis treated with lower osteoarthritis (OA) is controversial, particularly in me- leg and hindfoot realignment surgery. We further questioned if outcome correlated with achieved alignment. The average chanically induced, malaligned ankle OA in which joint patient age was 43 years (range, 26–68 years). We used a cartilage is partially preserved. These patients typically are standardized clinical and radiographic protocol. Besides dis- in their economically important, active middle ages be- tal tibial osteotomies, additional bony and soft tissue proce- cause early trauma is the predominant (70–80%) etiology dures were performed in 32 patients (91%). At mean fol- of their ankle OA.49,58 Currently, treatment recommenda- lowup of 5 years (range, 3–10.5 years), pain decreased by an tions after failed nonoperative therapy are polarized be- average of 4 points on a visual analog scale; range of ankle tween fusion2,11,33 and total ankle replacement motion increased by an average of 5°. -

Ankle and Pantalar Arthrodesis
ANKLE AND PANTALAR ARTHRODESIS George E. Quill, Jr., M.D. In: Foot and Ankle Disorders Edited by Mark S. Myerson, M.D. Since reports in the late 19th Century, arthrodesis has been a successful accepted treatment method for painful disorders of the ankle, subtalar, and transverse tarsal joints. While the title of this chapter involves arthrodesis - the intentional fusion of a joint - as a form of reconstruction, this chapter will address not only surgical technique, but nonoperative methods of care as well. We will address the pathophysiology leading to ankle and hindfoot disability, succinctly review the existing literature on the topic of hindfoot and ankle arthrodesis, highlight the pathomechanics involved, and spend considerable time on establishing the diagnosis, indications, and preoperative planning when surgery is indicated. We also will discuss the rehabilitation of the postoperative patient, as well as the management of complications that may arise after ankle and pantalar arthrodesis. There are more than thirty different viable techniques that have been described in order to achieve successful ankle and hindfoot arthrodesis. It is not the purpose of this chapter to serve as compendium of all the techniques ever described. The author will, rather, attempt to distill into a useful amount of clinically applicable material this vast body of information that the literature and clinical experience provide. Ankle arthrodesis is defined as surgical fusion of the tibia to the talus. Surgical fusion of the ankle (tibiotalar) and subtalar (talocalcaneal) joints at the same operative sitting is termed tibiotalocalcaneal arthrodesis. Fusion of the talus to all the bones articulating with it (distal tibia, calcaneus, navicular, and cuboid) is termed pantalar arthrodesis. -

Knee Joint Surgery: Open Arthodesis of the Knee, Unspecified
Musculoskeletal Surgical Services: Open Surgical Procedures; Knee Joint Surgery: Open Arthodesis of the knee, unspecified POLICY INITIATED: 06/30/2019 MOST RECENT REVIEW: 06/30/2019 POLICY # HH-5623 Overview Statement The purpose of these clinical guidelines is to assist healthcare professionals in selecting the medical service that may be appropriate and supported by evidence to improve patient outcomes. These clinical guidelines neither preempt clinical judgment of trained professionals nor advise anyone on how to practice medicine. The healthcare professionals are responsible for all clinical decisions based on their assessment. These clinical guidelines do not provide authorization, certification, explanation of benefits, or guarantee of payment, nor do they substitute for, or constitute, medical advice. Federal and State law, as well as member benefit contract language, including definitions and specific contract provisions/exclusions, take precedence over clinical guidelines and must be considered first when determining eligibility for coverage. All final determinations on coverage and payment are the responsibility of the health plan. Nothing contained within this document can be interpreted to mean otherwise. Medical information is constantly evolving, and HealthHelp reserves the right to review and update these clinical guidelines periodically. No part of this publication may be reproduced, stored in a retrieval system or transmitted, in any form or by any means, electronic, mechanical, photocopying, or otherwise, without permission -

DISSERTATION INVESTIGATION of CATIONIC CONTRAST-ENHANCED COMPUTED TOMOGRAPHY for the EVALUATION of EQUINE ARTICULAR CARTILAGE Su
DISSERTATION INVESTIGATION OF CATIONIC CONTRAST-ENHANCED COMPUTED TOMOGRAPHY FOR THE EVALUATION OF EQUINE ARTICULAR CARTILAGE Submitted by Bradley B. Nelson Department of Clinical Sciences In partial fulfillment of the requirements For the Degree of Doctor of Philosophy Colorado State University Fort Collins, Colorado Fall 2017 Doctoral Committee: Advisor: Christopher E. Kawcak Co-Advisor: Laurie R. Goodrich C. Wayne McIlwraith Mark W. Grinstaff Myra F. Barrett Copyright by Bradley Bernard Nelson 2017 All Rights Reserved ABSTRACT INVESTIGATION OF CATIONIC CONTRAST-ENHANCED COMPUTED TOMOGRAPHY FOR THE EVALUATION OF EQUINE ARTICULAR CARTILAGE Osteoarthritis and articular cartilage injury are substantial problems in horses causing joint pain, lameness and decreased athleticism resonant of the afflictions that occur in humans. This debilitating joint disease causes progressive articular cartilage degeneration and coupled with a poor capacity to heal necessitates that articular cartilage injury is detected early before irreparable damage ensues. The use of diagnostic imaging is critical to identify and characterize articular cartilage injury, though currently available methods are unable to identify these early degenerative changes. Cationic contrast-enhanced computed tomography (CECT) uses a cationic contrast media (CA4+) to detect the early molecular changes that occur in the extracellular matrix. Glycosaminoglycans (GAGs) within the extracellular matrix are important for the providing the compressive stiffness of articular cartilage and their degradation is an early event in the development of osteoarthritis. Cationic CECT imaging capitalizes on the electrostatic attraction between CA4+ and GAGs; exposing the proportional relationship between the amount of GAGs present within and the amount of CA4+ that diffuses into the tissue. The amount of CA4+ that resides in the tissue is then quantified through CECT imaging and estimates tissue integrity through nondestructive assessment. -
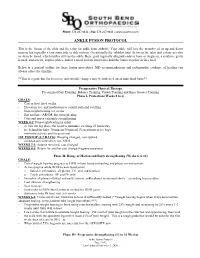
Ankle Fusion Protocol
Phone: 574.247.9441 ● Fax: 574.247.9442 ● www.sbortho.com ANKLE FUSION PROTOCOL This is the fusion of the tibia and the talus for ankle joint arthritis. Your ankle will lose the majority of its up and down motion, but typically retain some side to side motion. Occasionally the subtalar joint (between the talus and calcaneus) also needs to be fused, which further stiffens the ankle. Bone graft (typically allograft/cadaver bone or Augment, a synthetic graft) is used, and screws, staples, plates, and/or a metal rod are inserted to hold the bones together as they heal. Below is a general outline for these fusion procedures. MD recommendations and radiographic evidence of healing can always affect the timeline. **This is a guideline for recovery, and specific changes may be indicated on an individual basis** Preoperative Physical Therapy Pre surgical Gait Training, Balance Training, Crutch Training and Knee Scooter Training Phase I- Protection (Weeks 0 to 6) GOALS: - Cast or boot for 6 weeks - Elevation, ice, and medication to control pain and swelling - Non-weight bearing x 6 weeks - Hip and knee AROM, hip strengthening - Core and upper extremity strengthening WEEK 0-2: Nonweightbearing in splint - elevate the leg above the heart to minimize swelling 23 hours/day - ice behind the knee 30 min on/30 min off (Vascutherm or ice bag) - minimize activity and focus on rest 1ST POSTOP (5-7 DAYS): Dressing changed, cast applied - continue strict elevation, ice, NWB WEEKS 2-3: Sutures removed, cast changed WEEKS 4-5: Return for another cast change -

Bones Can Tell Us More Compiled By: Nancy Volk
Bones Can Tell Us More Compiled By: Nancy Volk Strong Bones Sometimes only a few bones are found in a location in an archeological dig. VOCABULARY A few bones can tell about the height of a person. This is possible due to the Femur ratios of the bones. It has been determined that there are relationships between the femur, tibia, humerus, and radius and a person’s height. Humerus Radius Here is a little help to identify these four bones and formulas to assist with Tibia determining the height of a person based on bone length. Humerus Femur: Humerus: The thigh is the region of the femur. The arm bone most people call the From the hip bone to the knee bone. upper arm. It is found from the elbow to the shoulder joints. Inside This Packet Radius Strong Bones 1 New York State Standards 1 Activity: Bone Relationships 2 Information for the Teacher 4 Tibia: Radius: The larger and stronger of the two bones The bone found in the forearm that New York State Standards in the leg below the knee bone. extends from the side of the elbow to Middle School In vertebrates It is recognized as the the wrist. Standard 4: Living Environment strongest weight bearing bone in the Idea 1: 1.2a, 1.2b, 1.2e, 1.2f body. Life Sciences - Post Module 3 Middle School Page 1 Activity: Bone Relationships MATERIALS NEEDED Skeleton Formulas: Tape Measure Bone relationship is represented by the following formulas: Directions and formulas P represents the person’s height. The last letter of each formula stands for the Calculator known length of the bone (femur, tibia, humerus, or radius) through measurement. -

Normative Values for Femoral Length, Tibial Length, Andthe Femorotibial
Article Normative Values for Femoral Length, Tibial Length, and the Femorotibial Ratio in Adults Using Standing Full-Length Radiography Stuart A Aitken MaineGeneral Medical Center, 35 Medical Center Parkway, Augusta, ME 04330, USA; [email protected] Abstract: Knowledge of the normal length and skeletal proportions of the lower limb is required as part of the evaluation of limb length discrepancy. When measuring limb length, modern standing full-length digital radiographs confer a level of clinical accuracy interchangeable with that of CT imaging. This study reports a set of normative values for lower limb length using the standing full-length radiographs of 753 patients (61% male). Lower limb length, femoral length, tibial length, and the femorotibial ratio were measured in 1077 limbs. The reliability of the measurement method was tested using the intra-class correlation (ICC) of agreement between three observers. The mean length of 1077 lower limbs was 89.0 cm (range 70.2 to 103.9 cm). Mean femoral length was 50.0 cm (39.3 to 58.4 cm) and tibial length was 39.0 cm (30.8 to 46.5 cm). The median side-to-side difference was 0.4 cm (0.2 to 0.7, max 1.8 cm) between 324 paired limbs. The mean ratio of femoral length to tibial length for the study population was 1.28:1 (range 1.16 to 1.39). A moderately strong inverse linear relationship (r = −0.35, p < 0.001, Pearson’s) was identified between tibial length and the Citation: Aitken, S.A. Normative corresponding femorotibial ratio.