St John Ambulance Australia (Western Australia) Inc
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Free Tv Guide Sydney Tonight
Free tv guide sydney tonight Continue ABC1 2/21 Drum 6:00pm ABC News 7:00pm 7.30pm 7.30pm Anh's Brush with glory 8:02pm Big weather (and how to survive) 8.30pm No time for quiet 9.26pm Insert name here 10.25pm ABC News Late 100 :56pm FOR 11:28pm ABC HD 20 Drum 6:00pm ABC News 7:00pm 7.30 7.30pm Anh's Brush with Glory 8.02pm Big Weather (and How to Survive) 8.30pm No time for Silent 9.26pm Insert name here 10.02pm ABC's Late News 10.56pm FOR 11.28pm ABC COMEDY/ABC Kids 22 Go Jetters 5.55pm Love Monster 6.11pm Bluey 6.20pm School Roars 6.27pm Ben and Holly Little Kingdom 6.35pm Andy Water Adventures 6.47pm Sir Mouse 7.02pm Odd Squad 7.15pm Spicks and Specks 7.33pm Spicks and Specks 8.01pm Insert Name Here 8.30pm Ghosts 9.01pm Trip to Greece 9.30pm Frontline 10.01pm Parks and Recreation 10.30pm Schitt's Creek 10.52pm Red Dwarf 11.16pm Rosehaven 11.45pm ABC ME 23 Total Drama 5.52pm Dragons: Race to the Edge 6.45pm ABC ME 23 Total Dramarama 5.52pm Dragons: Race to Edge 6:: 02pm BT NEWSbreak 6.25pm Horrible Stories 6.31pm Deadly Pole to Pole 7:00pm Shaun the Sheep 7.30pm Penguins of Madagascar 7.37pm Thunderbirds Go 8.00pm Best Mistakes Forever 8.23pm Get Blake! 8.35pm The Secret Life of the Boys 8.48pm Sailor Luna Crystal 9.11pm Miracle: Tales of Ladybird and Cat Noir 9.35pm Fury 9.58pm ABC Me Program Resume at 5.30am 1 0:58pm ABC NEWS 24 ABC Evening News 6:00pm ABC National News 7:00pm ABC News Tonight at 8:00pm Business 8:45pm ABC News Update 9:00 p.m. -
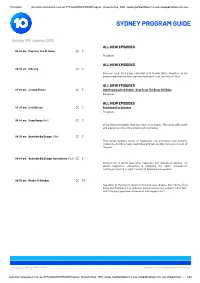
Sydney Program Guide
1/10/2020 prtten04.networkten.com.au:7778/pls/DWHPROD/Program_Reports.Dsp_TEN_Guide?psStartDate=12-Jan-20&psEndDate=25-Jan-… SYDNEY PROGRAM GUIDE Sunday 12th January 2020 ALL NEW EPISODES 06:00 am Mass For You At Home CC G Religious. ALL NEW EPISODES 06:30 am Hillsong CC G Discover your God-given potential with Pastor Brian Houston as he shares empowering and inspiring messages from the Word of God. ALL NEW EPISODES 07:00 am Joseph Prince CC G Overflowing Life & Health - Keys From The Story Of Elisha Religious ALL NEW EPISODES 07:30 am Joel Osteen CC G Positioned For Increase Religious. 08:00 am Snap Happy (Rpt) CC G If you like photography then you'll love Snap Happy. This show will inspire and equip you to become a better photographer. 08:30 am Australia By Design: (Rpt) CC G This series gathers some of Australia's top architects and industry leaders to decide what is Australia's ultimate architectural statement of the year. 09:00 am Australia By Design: Innovations (Rpt) CC G Innovations is about Australian ingenuity and design excellence, it's about inspiration, disruption & changing the game. Innovations continues to bring to light the best of Australian innovation. 09:30 am Studio 10 Sunday CC PG See what all the fuss is about with Sarah, Joe, Angela, Kerri-Anne, Ding Dong and Narelda. Fiery debates, big exclusives and a whole lot of fun - with this gang you never know what will happen next! Last Updated 10th Jan 2020 - 14:31 © Network Ten Pty Limited ABN 91 052 515 250 prtten04.networkten.com.au:7778/pls/DWHPROD/Program_Reports.Dsp_TEN_Guide?psStartDate=12-Jan-20&psEndDate=25-Jan-20&psChan… 1/54 1/10/2020 prtten04.networkten.com.au:7778/pls/DWHPROD/Program_Reports.Dsp_TEN_Guide?psStartDate=12-Jan-20&psEndDate=25-Jan-… SYDNEY PROGRAM GUIDE Sunday 12th January 2020 ALL NEW EPISODES 12:00 pm The Offroad Adventure Show CC G Four ultimate touring 4WDs, two all-new thrillseeking hosts, tackling our toughest adventures yet, discovering spectacular campsites and bucket list adventures along the way. -

Your Prime Time Tv Guide ABC (Ch2) SEVEN (Ch6) NINE (Ch5) WIN (Ch8) SBS (Ch3) 6Pm the Drum
tv guide PAGE 2 FOR DIGITAL CHOICE> your prime time tv guide ABC (CH2) SEVEN (CH6) NINE (CH5) WIN (CH8) SBS (CH3) 6pm The Drum. 6pm Seven Local News. 6pm Nine News. 6pm WIN News. 6pm Mastermind Australia. 7.00 ABC News. 6.30 Seven News. 7.00 A Current Affair. 6.30 The Project. 6.30 SBS World News. Y 7.30 Gardening Australia. Josh gets 7.00 Better Homes And Gardens. 7.30 Escape To The Chateau. (PG) 7.30 The Living Room. (PG) 7.30 Secrets Unearthed: Maya A tips from a thriving family garden. 8.30 MOVIE Game Night. (2018) 8.30 MOVIE Gladiator. (2000) (M) 8.30 To Be Advised. Pyramid. (PG) D I 8.30 Vera. (M) A social worker’s (MA15+) Jason Bateman, Rachel Russell Crowe, Joaquin Phoenix. A 9.30 Have You Been Paying 8.25 The World’s Most murder is investigated. McAdams. Friends become Roman general seeks revenge. Attention? (M) Hosted by Extraordinary Homes: FR 10.00 Mum. (M) entangled in a real-life mystery. 11.35 MOVIE The Man With The Tom Gleisner. Underground. Part 4 of 4. 10.35 ABC Late News. 10.40 To Be Advised. Iron Fists. (2012) (MA15+) 10.30 To Be Advised. 9.35 8 Out Of 10 Cats. (M) 10.50 Gruen. 11.45 Surveillance Oz. (PG) 11.00 WIN’s All Australian News. 10.25 SBS News. 8pm QLD Votes: Election Results 6pm Seven News. 6pm Nine News Saturday. 6pm Rugby Union. Tri-Nations. 6.30pm News. Y Live. Continued coverage of the 7.00 7NEWS Special: Queensland 6.30 Election 2020: Qld Decides - Round 1. -

Sydney Program Guide
Firefox http://prtten04.networkten.com.au:7778/pls/DWHPROD/Program_Repor... SYDNEY PROGRAM GUIDE Sunday 13th December 2020 ALL NEW EPISODES 06:00 am Mass For You At Home CC G Religious. ALL NEW EPISODES 06:30 am Hillsong CC G Religious. ALL NEW EPISODES 07:00 am Joseph Prince CC G 353 - Can I Ask God To Prosper Me? Religious ALL NEW EPISODES 07:30 am Joel Osteen CC G Jo861 - Letting Go Of Control Religious. 08:00 am Australia By Design: Interiors (Rpt) CC G Australia By Design: Interiors takes us into the heart of the design process and looks at the psychology of interpreting space and creating an environment. 08:30 am The Living Room Encore (Rpt) CC Baz scrubs up a tired old bathroom and transforms an unused space into every teenage girls dream and Miguel adds a taste of home to a classic custard. 09:30 am Studio 10 Sunday CC PG Start your day with a dose of sunshine and join the feelgood fun with Sarah Harris and Tristan MacManus weekdays from 8am. 12:00 pm Destination Dessert (Rpt) CC G Destination Dessert is the ultimate travel show for the sweet tooth! Exploring NSW in our first series, discovering the sweeter things in life. 12:30 pm Roads Less Travelled (Rpt) CC An Australian Road Trip Series exploring those hidden gems that only the locals know about. Tour some of the lesser known roads exploring unique locations amidst Australia’s natural beauty. 1 of 52 27/11/2020, 3:54 pm Firefox http://prtten04.networkten.com.au:7778/pls/DWHPROD/Program_Repor.. -

Water Is Lifeblood
Thursday, June 10, 2021 Print Post approved – 100003237 $1.70 inc GST Sport from Regional the regions roundup From page 12 pages 6 & 7 Health Water is lifeblood turmoil in MIA Nicholas Rupolo organiser Mick Grayson said HEALTH Services Union paramedics regional paramedics were at a across the Riverina will only attend significant disadvantage from lower to serious emergencies today pay and costly work practices. following NSW Treasurer Dominic Mr Grayson said regional staff Perrottet’s wage increase offer the had paid for their own professional union describes as “humiliating and development, registration fees and insulting”. working with children checks. A 24-hour strike today (June “And the government basically 10) will see paramedics only treat refuses to pass on meagre 2.5 per cent “the most urgent, life threatening pay rise,” he said. “Queensland and emergencies” in an attempt to force ACT paramedics are approximately the hand of the government. $200 a week better off than NSW This industrial action has been paramedics. Specifically in the taken by workers and the union after Riverina, paramedic numbers are they were offered a 0.3 per cent pay the lowest of the major states, the increase in 2020 and a 1.5 per cent Riverina has the lowest paramedic increase in 2021. to community ratios, they work The union says it is a low-ball harder for less.” offer considering the government’s A major concern for paramedics budget accounts for inflation at and the HSU is the low wage offers 2.2 per cent. paired with rising average increases Following the freezing of public in the cost of living. -

Swine Flu: Vol24 Evacuations in New Zealand
The Australian Journal of Emergency Management Vol 24 No 3 AUGUST 2009 Swine flu: Australia’s preparations Vol 24 Vol and response No 3 AUGUST 2009 Does experience How will climate change affect Preparing for Tsunami alter fire fighters’ attitudes our volunteer sector? evacuations in New Zealand. to safety? GREY18166 historical snapshot interesting websites Australian Government Department of Health & Ageing Preparing for pandemic influenza website http://www.healthemergency.gov.au/ internet/healthemergency/publishing.nsf This website provides important information about pandemic influenza, including what the Australian Government will do if it happens, and what individuals, businesses, communities and health care professionals can do to prepare for and respond to a flu pandemic. This website was developed in consultation with State and Territory and local governments. Even though Australia is well equipped, governments alone cannot respond effectively to a flu pandemic. It is important that we are all prepared for the possibility of a pandemic and ready to respond to the threat to help slow the spread of infection and lessen the impact. The Influenza Pandemic of 1918 The influenza pandemic of 1918-1919 killed more people than World War I, at somewhere between 20 and 40 million people. It has been cited as the most devastating epidemic in recorded world history. More people died of influenza in a single year than in four-years of the Black Death Bubonic Plague from 1347 to 1351. Known as “Spanish Flu” or “La Grippe” the influenza of 1918-1919 was a global disaster. The gauze mask was a prevention method using ideas of contagion and germ theory. -

2019-20 Annual Report on Behalf of the Many People and Their Stories That Lie Behind the Numbers, Tables and Graphs
Department of Health Annual Report 2019-20 © Government of Tasmania 2020 For further information, please contact: Department of Health Office of the Secretary GPO Box 125 Hobart TAS 7001 Telephone: 1300 135 513 Website: www.health.tas.gov.au Published October 2020 ISBN 978-0-9924618-2-9 Hon Sarah Courtney MP Hon Jeremy Rockliff MP Minister for Health Deputy Premier Minister for Women Minister for Education and Training Minister for Strategic Growth Minister for Trade Minister for Small Business, Hospitality and Events Minister for Advanced Manufacturing and Defence Industries Minister for Disability Services and Community Development Minister for Mental Health and Wellbeing Dear Ministers Department of Health Annual Report 2019-20 In accordance with the requirements of Section 30 of the Tasmanian Health Service Act 2018, Section 36 of the State Service Act 2000 and Section 42 of the Financial Management Act 2016, I have pleasure in presenting the Department of Health Annual Report for the financial year ending 30 June 2020. Please note that this report also includes reports from the Council of Obstetric and Paediatric Mortality and Morbidity and the Tasmanian Pharmacy Authority. Kathrine Morgan-Wicks Secretary, Department of Health 7 October 2020 This page is intentionally blank Contents Page INTRODUCTION Message from the Secretary 2 COVID-19 Response 5 Governance 9 OUR DEPARTMENT Department Overview 14 System Manager and THS Service Plan 25 Quality and Patient Safety 30 Consumer and Community Engagement 33 Workforce Overview 36 Awards -

Your Prime Time Tv Guide ABC (Ch2) SEVEN (Ch6) NINE (Ch5) WIN (Ch8) SBS (Ch3) 6Pm the Drum
tv guide PAGE 2 FOR DIGITAL CHOICE> your prime time tv guide ABC (CH2) SEVEN (CH6) NINE (CH5) WIN (CH8) SBS (CH3) 6pm The Drum. 6pm Seven Local News. 6pm Nine News. 6pm WIN News. 6.30pm News. 7.00 ABC News. 6.30 Seven News. 6.30 Rugby League. NRL Finals 6.30 The Project. 7.35 Secrets Unearthed: Y 7.30 Gardening Australia. Millie 7.00 Better Homes And Gardens. Series. First semi-final. 7.30 The Living Room. (PG) Pyramids. (PG) A transforms her lawn into lunch. 8.30 MOVIE John Q. (2002) (M) 8.45 NRL Finals Footy Post-Match. 8.30 To Be Advised. 8.30 The World’s Most D I 8.30 Vera. (M) A woman is murdered Denzel Washington, Robert Duvall. 9.30 MOVIE The Last Castle. 9.30 Have You Been Paying Extraordinary Homes: Mountain. in a hedgerow. An emergency ward is held hostage. (2001) (M) Robert Redford, James Attention? (M) Hosted by (PG) Part 1 of 4. FR 10.00 Mum. (M) 11.00 MOVIE Eraser. (1996) (MA15+) Gandolfini. A disgraced general Tom Gleisner. 9.30 8 Out Of 10 Cats Does 10.30 ABC Late News. organises an uprising. 10.30 To Be Advised. Countdown. (M) 10.45 The Virus. 11.00 WIN’s All Australian News. 10.25 SBS News. 7pm ABC News. 6pm Seven News. 6pm Nine News Saturday. 6pm Bondi Rescue. (PG) 6.30pm News. Y 7.30 Father Brown. (M) A body is 7.00 MOVIE Night At The Museum: 6.30 Rugby League. NRL Finals 7.00 The Masked Singer USA. -

Review of Ambulance Tasmania Clinical and Operational Services | Final Report | May 2017 1 Executive Summary
Review of Ambulance Tasmania Clinical and Operational Service Final Report May 2017 Department of Health and Human Services Contents Executive Summary 2 Recommendations 5 Short Term Demand Pressures 5 Secondary Triage and Partnerships 5 Extended Care Paramedics and Urgent Care Centres 5 Extended Care Paramedic and Intensive Care Paramedic Training 5 Ambulance Tasmania and Emergency Department Interface 5 Non-Emergency Patient Transport Service 6 AT Organisation Structure 6 Scope and Structure 7 Background and Terms of Reference 7 Review Design 8 Structure of the Report 8 Review Context – Evolving Role of Paramedicine 9 Acute Care 9 Non-Acute Care 9 Non-Emergency Patient Transport 10 Aeromedical Retrieval Services 10 Demand Analysis 11 Ambulance Services 11 Emergency Departments 12 Drivers of Demand and Utilisation 14 Potential for Alternative Solutions 16 Reforming Ambulance Tasmania’s Service Model 18 Secondary Triage 19 Extended Care Paramedics 22 Urgent Care Centres 26 Intensive Care Paramedics 26 Training of ECPs and ICPs 28 Patient Management Plans 29 Improving the Interface between Ambulance Tasmania and Emergency Departments 30 Engaging Non-Emergency Patient Transport 32 Referral to NEPT Services from Ambulance Tasmania 31 Improved Regulation of Support for Major Events 33 Greater Flexibility for Utilisation and Innovation in NEPT Services 34 Balancing Operational and Non-Operational Resources 33 Non-Operational Resources 35 Operational Support and Supervision 37 Corporate Support 38 Conclusions and Next Steps 39 Acronyms 40 Review of Ambulance Tasmania Clinical and Operational Services | Final Report | May 2017 1 Executive Summary Ambulance Tasmania (AT) provides Without reform, the emergency-focussed emergency and non-emergency services service model of Ambulance Tasmania to people requiring medical assistance will continue to direct patients towards and/or transportation. -

Sydney Program Guide
2/15/2019 prtten04.networkten.com.au:7778/pls/DWHPROD/Program_Reports.Dsp_TEN_Guide?psStartDate=24-Feb-19&psEndDate=02-Mar… SYDNEY PROGRAM GUIDE Sunday 24th February 2019 06:00 am Mass For You At Home CC G Religious program. ALL NEW EPISODES 06:30 am Hillsong CC G Religious Program ALL NEW EPISODES 07:00 am Joesph Prince New Creation CC G Church Pastor Joseph Prince is a leading voice in proclaiming the gospel of grace around the world. He is the senior pastor of New Creation Church, a vibrant and fast-growing church in Singapore. ALL NEW EPISODES 07:30 am Joel Osteen CC G You Are Fully Loaded Religious. 08:00 am Escape Fishing With ET (Rpt) CC G Join Andrew 'ET' Ettingshausen, as he escapes the city for adventure around Australia and the Pacific, hunting out the most exciting species & interesting spots with his mates. 08:30 am Foodie Adventures With Ash CC G Fiji - Steve Price Pollard (Rpt) Ash discovers the fresh, vibrant flavours of Fiji, learning from top international and local chefs. Her dinner guest this week is Steve Price. 09:00 am Places We Go With Jennifer Adams CC PG S11ep.3 (Rpt) Places We Go is series about real travel, hosted by real travellers. Jennifer Adams and Clint Bizzell take viewers on a journey to some of most stunning destinations around Australia and the World. ALL NEW EPISODES 09:30 am Studio 10 Sunday CC PG See what all the fuss is about with Sarah, Joe, Angela, Kerri-Anne Kennerley, Denise Drysdale and Denise Scott. -

Abstracts of the 2011 Paramedics Australasia Conference
Australasian Journal of Prehospital Care: 2013;10(2) Conference Abstracts Abstracts of the 2011 Paramedics Australasia Conference Sydney, New South Wales, Australia 7th and 8th October 2011 Conference Presentation Abstracts that may influence clinical decision making and subsequent actions when assessing patients with A model of paramedic decision making in a complaint of pain. cases involving pain. Bill Lord Conclusions This model of clinical decision making may help Monash University, Victoria, Australia. guide the education of paramedics to enable an Objectives awareness of factors that have the potential to Patients have a right to pain relief on humanitarian adversely influence their clinical decision making. grounds. In addition, unrelieved pain may be associated with morbidity such as the development of chronic pain syndromes. Epidemiology of acute heart failure Paramedics have an important role in relieving presentations and prehospital treatment pain. However, therapeutic interventions that aim by paramedics in New South Wales, to reduce pain depend on clinical judgments that Australia: a retrospective analysis of over involve assessment of the of the patient's reported 7000 patients. symptoms. As pain is a symptom that is difficult to 1 2 Paul Simpson and Jason Bendall objectively validate it is conceivable that clinician's beliefs and attitudes may modify clinical 1Ambulance Research Institute, Ambulance judgements and consequently influence decisions Service of New South Wales, Sydney, New to withhold or initiate care. To investigate -

Ambulance Policy Summary
Ambulance Policy Summary Please read this policy summary carefully and retain. For more policy information, definitions and claiming requirements please refer to Westfund’s Membership Terms & Conditions which can be downloaded at www.westfund.com.au/terms- conditions or by calling Westfund on 1300 937 838. Our Privacy Policy and Complaints Policy as well as information about the Code of Conduct and Commonwealth Ombudsman are also included in our Membership Terms & Conditions. Ambulance Cover Service Waiting Period Item Limit Annual Group Limit Additional Information Emergency Benefit eligible for Westfund recognised ambulance Ambulance 1 day 100% No annual limit service providers in Australia. Westfund covers the cost of Transport transport by either covering the cost of state government levies or covering the ambulance account. Ambulance services not available under this policy: - Inter-hospital transfers between public hospitals Non-Emergency 2 months 100% $5,000 per member - Member requested ambulance transport e.g. to be Patient Transport closer to home/family. Emergency Ambulance Transport Emergency Ambulance transport is ambulance transportation of an unplanned and non-routine nature for the purpose of providing immediate medical attention to a person in the opinion of the treating medical officer. An ambulance service where subsequent transport to a hospital is not required is covered under non-emergency patient transport. Non-Emergency Patient Transport Non-emergency patient transport is ambulance transportation including on the spot treatment where a time critical ambulance response is not essential however clinical monitoring is required for the purpose of providing medical attention to a person in the opinion of the treating medical officer.