Nasal Carriage, Risk Factors and Antimicrobial Susceptibility Pattern of Methicillin Resistant Staphylococcus Aureus Among Healt
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Situation Report EEPA HORN No. 59 - 18 January 2021
Situation Report EEPA HORN No. 59 - 18 January 2021 Europe External Programme with Africa is a Belgium-based Centre of Expertise with in-depth knowledge, publications, and networks, specialised in issues of peace building, refugee protection and resilience in the Horn of Africa. EEPA has published extensively on issues related to movement and/or human trafficking of refugees in the Horn of Africa and on the Central Mediterranean Route. It cooperates with a wide network of Universities, research organisations, civil society and experts from Ethiopia, Eritrea, Kenya, Djibouti, Somalia, Sudan, South Sudan, Uganda and across Africa. Reported war situation (as confirmed per 17 January) - According to Sudan Tribune, the head of the Sudanese Sovereign Council, Abdel Fattah al-Burhan, disclosed that Sudanese troops were deployed on the border as per an agreement with the Ethiopian Prime Minister, Abiy Ahmed, arranged prior to the beginning of the war. - Al-Burhan told a gathering about the arrangements that were made in the planning of the military actions: “I visited Ethiopia shortly before the events, and we agreed with the Prime Minister of Ethiopia that the Sudanese armed forces would close the Sudanese borders to prevent border infiltration to and from Sudan by an armed party.” - Al-Burhan stated: "Actually, this is what the (Sudanese) armed forces have done to secure the international borders and have stopped there." His statement suggests that Abiy Ahmed spoke with him about the military plans before launching the military operation in Tigray. - Ethiopia has called the operation a “domestic law and order” action to respond to domestic provocations, but the planning with neighbours in the region on the actions paint a different picture. -
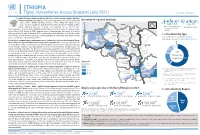
20210714 Access Snapshot- Tigray Region June 2021 V2
ETHIOPIA Tigray: Humanitarian Access Snapshot (July 2021) As of 31 July 2021 The conflict in Tigray continues despite the unilateral ceasefire announced by the Ethiopian Federal Government on 28 June, which resulted in the withdrawal of the Ethiopian National Overview of reported incidents July Since Nov July Since Nov Defense Forces (ENDF) and Eritrea’s Defense Forces (ErDF) from Tigray. In July, Tigray forces (TF) engaged in a military offensive in boundary areas of Amhara and Afar ERITREA 13 153 2 14 regions, displacing thousands of people and impacting access into the area. #Incidents impacting Aid workers killed Federal authorities announced the mobilization of armed forces from other regions. The Amhara region the security of aid Tahtay North workers Special Forces (ASF), backed by ENDF, maintain control of Western zone, with reports of a military Adiyabo Setit Humera Western build-up on both sides of the Tekezi river. ErDF are reportedly positioned in border areas of Eritrea and in SUDAN Kafta Humera Indasilassie % of incidents by type some kebeles in North-Western and Eastern zones. Thousands of people have been displaced from town Central Eastern these areas into Shire city, North-Western zone. In line with the Access Monitoring and Western Korarit https://bit.ly/3vcab7e May Reporting Framework: Electricity, telecommunications, and banking services continue to be disconnected throughout Tigray, Gaba Wukro Welkait TIGRAY 2% while commercial cargo and flights into the region remain suspended. This is having a major impact on Tselemti Abi Adi town May Tsebri relief operations. Partners are having to scale down operations and reduce movements due to the lack Dansha town town Mekelle AFAR 4% of fuel. -

Starving Tigray
Starving Tigray How Armed Conflict and Mass Atrocities Have Destroyed an Ethiopian Region’s Economy and Food System and Are Threatening Famine Foreword by Helen Clark April 6, 2021 ABOUT The World Peace Foundation, an operating foundation affiliated solely with the Fletcher School at Tufts University, aims to provide intellectual leadership on issues of peace, justice and security. We believe that innovative research and teaching are critical to the challenges of making peace around the world, and should go hand-in- hand with advocacy and practical engagement with the toughest issues. To respond to organized violence today, we not only need new instruments and tools—we need a new vision of peace. Our challenge is to reinvent peace. This report has benefited from the research, analysis and review of a number of individuals, most of whom preferred to remain anonymous. For that reason, we are attributing authorship solely to the World Peace Foundation. World Peace Foundation at the Fletcher School Tufts University 169 Holland Street, Suite 209 Somerville, MA 02144 ph: (617) 627-2255 worldpeacefoundation.org © 2021 by the World Peace Foundation. All rights reserved. Cover photo: A Tigrayan child at the refugee registration center near Kassala, Sudan Starving Tigray | I FOREWORD The calamitous humanitarian dimensions of the conflict in Tigray are becoming painfully clear. The international community must respond quickly and effectively now to save many hundreds of thou- sands of lives. The human tragedy which has unfolded in Tigray is a man-made disaster. Reports of mass atrocities there are heart breaking, as are those of starvation crimes. -

ETHIOPIA - TIGRAY REGION HUMANITARIAN UPDATE Situation in Tigray (1 July 2021) Last Updated: 2 Jul 2021
ETHIOPIA - TIGRAY REGION HUMANITARIAN UPDATE Situation in Tigray (1 July 2021) Last updated: 2 Jul 2021 FLASH UPDATE (2 Jul 2021) Situation in Tigray (1 July 2021) The political dynamics have changed dramatically in Ethiopia's Tigray Region following the unilateral ceasefire declaration by the Ethiopian Government on 28 June 2021. Reportedly, the Tigray Defense Forces (TDF) have taken control over most parts of Tigray following the withdrawal of the Ethiopian and Eritrean defense forces from the capital, Mekelle, and other parts of the region, while Western Tigray remains under the control of the Amhara Region. The consequences of the unfolding situation on humanitarian operations in Tigray remain fluid. The breakdown of essential services such as the blackout of electricity, telecommunications, and internet throughout Tigray region will only exacerbate the already dire humanitarian situation. Reported shortages of cash and fuel in the region can compromise the duty of care of aid workers on the ground. Despite the dynamic and uncertain situation, partners report that the security situation in Tigray has been generally calm over the past few days, with limited humanitarian activities being implemented around Mekelle and Shire. Key developments On 28 June, the Federal Government agreed to the request from the Interim Regional Administration in Tigray for a "unilateral ceasefire, until the farming season ends." Subsequently, Ethiopia National Defense Forces (ENDF) withdrew from Mekelle and other main towns in the region, including Shire, Axum, Adwa, and Adigrat. Currently, former Tigray Defense Forces (TDF) are in control of the main cities and roads in Tigray. There were no reports of fighting in Mekelle and other towns. -

Investment Opportunities in Mekelle, Tigray State, Ethiopia
MCI AND VCC WORKING PAPER SERIES ON INVESTMENT IN THE MILLENNIUM CITIES No 10/2009 INVESTMENT OPPORTUNITIES IN MEKELLE, TIGRAY STATE, ETHIOPIA Bryant Cannon December 2009 432 South Park Avenue, 13th Floor, New York, NY10016, United States Phone: +1-646-884-7422; Fax: +1-212-548-5720 Websites: www.earth.columbia.edu/mci; www.vcc.columbia.edu MCI and VCC Working Paper Series o N 10/2009 Editor-in-Chief: Dr. Karl P. Sauvant, Co-Director, Millennium Cities Initiative, and Executive Director, Vale Columbia Center on Sustainable International Investment: [email protected] Editor: Joerg Simon, Senior Investment Advisor, Millennium Cities Initiative: [email protected] Managing Editor: Paulo Cunha, Coordinator, Millennium Cities Initiative: [email protected] The Millennium Cities Initiative (MCI) is a project of The Earth Institute at Columbia University, directed by Professor Jeffrey D. Sachs. It was established in early 2006 to help sub-Saharan African cities achieve the Millennium Development Goals (MDGs). As part of this effort, MCI helps the Cities to create employment, stimulate enterprise development and foster economic growth, especially by stimulating domestic and foreign investment, to eradicate extreme poverty – the first and most fundamental MDG. This effort rests on three pillars: (i) the preparation of various materials to inform foreign investors about the regulatory framework for investment and commercially viable investment opportunities; (ii) the dissemination of the various materials to potential investors, such as through investors’ missions and roundtables, and Millennium Cities Investors’ Guides; and (iii) capacity building in the Cities to attract and work with investors. The Vale Columbia Center on Sustainable International Investment promotes learning, teaching, policy-oriented research, and practical work within the area of foreign direct investment, paying special attention to the sustainable development dimension of this investment. -

Ethiopia: Administrative Map (August 2017)
Ethiopia: Administrative map (August 2017) ERITREA National capital P Erob Tahtay Adiyabo Regional capital Gulomekeda Laelay Adiyabo Mereb Leke Ahferom Red Sea Humera Adigrat ! ! Dalul ! Adwa Ganta Afeshum Aksum Saesie Tsaedaemba Shire Indasilase ! Zonal Capital ! North West TigrayTahtay KoraroTahtay Maychew Eastern Tigray Kafta Humera Laelay Maychew Werei Leke TIGRAY Asgede Tsimbila Central Tigray Hawzen Medebay Zana Koneba Naeder Adet Berahile Region boundary Atsbi Wenberta Western Tigray Kelete Awelallo Welkait Kola Temben Tselemti Degua Temben Mekele Zone boundary Tanqua Abergele P Zone 2 (Kilbet Rasu) Tsegede Tselemt Mekele Town Special Enderta Afdera Addi Arekay South East Ab Ala Tsegede Mirab Armacho Beyeda Woreda boundary Debark Erebti SUDAN Hintalo Wejirat Saharti Samre Tach Armacho Abergele Sanja ! Dabat Janamora Megale Bidu Alaje Sahla Addis Ababa Ziquala Maychew ! Wegera Metema Lay Armacho Wag Himra Endamehoni Raya Azebo North Gondar Gonder ! Sekota Teru Afar Chilga Southern Tigray Gonder City Adm. Yalo East Belesa Ofla West Belesa Kurri Dehana Dembia Gonder Zuria Alamata Gaz Gibla Zone 4 (Fantana Rasu ) Elidar Amhara Gelegu Quara ! Takusa Ebenat Gulina Bugna Awra Libo Kemkem Kobo Gidan Lasta Benishangul Gumuz North Wello AFAR Alfa Zone 1(Awsi Rasu) Debre Tabor Ewa ! Fogera Farta Lay Gayint Semera Meket Guba Lafto DPubti DJIBOUTI Jawi South Gondar Dire Dawa Semen Achefer East Esite Chifra Bahir Dar Wadla Delanta Habru Asayita P Tach Gayint ! Bahir Dar City Adm. Aysaita Guba AMHARA Dera Ambasel Debub Achefer Bahirdar Zuria Dawunt Worebabu Gambela Dangura West Esite Gulf of Aden Mecha Adaa'r Mile Pawe Special Simada Thehulederie Kutaber Dangila Yilmana Densa Afambo Mekdela Tenta Awi Dessie Bati Hulet Ej Enese ! Hareri Sayint Dessie City Adm. -

SITUATION ANALYSIS of CHILDREN and WOMEN: Tigray Region
SITUATION ANALYSIS OF CHILDREN AND WOMEN: Tigray Region SITUATION ANALYSIS OF CHILDREN AND WOMEN: Tigray Region This briefing note covers several issues related to child well-being in Tigray Regional State. It builds on existing research and the inputs of UNICEF Ethiopia sections and partners.1 It follows the structure of the Template Outline for Regional Situation Analyses. 1Most of the data included in this briefing note comes from the Ethiopia Demographic and Health Survey (EDHS), Household Consumption and Expenditure Survey (HCES), Education Statistics Annual Abstract (ESAA) and Welfare Monitoring Survey (WMS) so that a valid comparison can be made with the other regions of Ethiopia. SITUATION ANALYSIS OF CHILDREN AND WOMEN: TIGRAY REGION 4 1 THE DEVELOPMENT CONTEXT The northern and mountainous region of Tigray has an estimated population of 5.4 million people, of which approximately 13 per cent are under 5 years old and 43 per cent is under 18 years of age. This makes Tigray the fifth most populous region of Ethiopia. Tigray has a relatively high percentage of female-headed households, at 34 per cent in 2018 versus a national rate of 25 per cent in 2016. Three out of four Tigrayans live in rural areas, and most depend on agriculture (mainly subsistence crop farming).4 Urbanization is an emerging priority, as many new towns are created, and existing towns expand. Urbanization in Tigray is referred to as ‘aggressive’, with an annual rate of 4.6 per cent in the Tigray Socio-Economic Baseline Survey Report (2018).5 The annual urban growth -

ETHIOPIA MONTHLY MARKET WATCH March 2014
ETHIOPIA MONTHLY MARKET March WATCH 2014 ETHIOPIA MONTHLY MARKET WATCH March 2014 Highlights The overall year to year general inflation rate increased by 8.8%; food inflation by 6.1% and non-food by 11.8% in March 2014. Since November 2013, month-to-month food inflation rate increases was below zero but in March 2014 increased by 2.4%. The import parity prices of maize (Durban) and wheat (Black sea) remained stable with upward changes of 4% for maize and 2% downward for wheat as compared to February 2014. The import parity price stood higher than the local wholesale price by about 73% for maize while 6% below the local wheat price at Addis Ababa. In March 2014, the prices of these cereals have remained almost synonymous compared to the preceding month. In all of monitored markets, the prices change were below 5% as compared to February 2014. The prevailing price stability is normal to the season and signifies better access for market dependent households. The retail prices of imported food items (rice, spaghetti and wheat flour) remained stable in Afar while rose at Deghabour and Kebridehar. The retail price of rice rose by 14% and 21% respectively at Kebridehar and Deghabour markets; sugar price increased by 13% at Kebridehar; spaghetti by 8% at Kebridehar and Deghabour. The Alert for Price Spikes (ALPS) The Alert for Price Spikes (ALPS) is used to detect abnormally high food prices. The indicator is constructed as the gap between observed prices and their long-term seasonal trend. The tool measures how far the observed prices depart from the seasonal price trends. -

Evidence of Targeted Ethnic Discrimination and Violence
Evidence of Targeted Ethnic Discrimination Against Tigrayans E X P L A I N E D | @omnatigray | omnatigray.org Not a “Law-and-Order Enforcement Operation” On November 4, 2020, unelected Prime Minister of Ethiopia Abiy Ahmed waged a war on Tigray. He claimed that the war was a domestic "law-and-order enforcement operation” that intended to target a few political rivals from the Tigray People’s Liberation Front (TPLF). Abiy claimed the operation would not disrupt the daily lives of Tigrayan civilians. Six months into the war with reports of great civilian casualties, ethnic based indiscriminate murder, rape, and other human rights violations – it is undeniably clear that this isn’t a ‘‘law-and-order enforcement operation’’ targeted at a few Tigrayan politicians, but rather a genocidal war on Tigray and Tigrayans as a whole. | @omnatigray | omnatigray.org Destroying Tigray’s Infrastructure Invading armies targeted various civilian institutions such as: hospitals, universities, power dam, sugar factory, textile factory, cement factory, and several others. The looting and destruction of civilian institutions highlight the true intent behind the war: disenfranchising Tigrayans for generations. | @omnatigray | omnatigray.org Destroying Tigray’s Infrastructure Some of the destroyed institutions include: Ancient religious institutions such as Al-Nejashi Mosque, St. Amanuel Orthodox Church, and Debre Damo. Not only were these religious sites bombed, but numerous artifacts and manuscripts were also stolen. Hospitals in Mekelle, Shire, Adigrat, Adwa and other Tigrayan cities have been looted and destroyed. In Adigrat alone, Adigrat Hospital has been decimated with only 10 out of the 400 healthcare workers, working to serve the city. -

Ethiopia: Access
ETHIOPIA Access Map - Tigray Region As of 31 May 2021 ERITREA Ethiopia Adi Hageray Seyemti Egela Zala Ambesa Dawuhan Adi Hageray Adyabo Gerhu Sernay Gulo Mekeda Erob Adi Nebried Sheraro Rama Ahsea Tahtay Fatsi Eastern Tahtay Adiyabo Chila Rama Adi Daero Koraro Aheferom Saesie Humera Chila Bzet Adigrat Laelay Adiabo Inticho Tahtay Selekleka Laelay Ganta SUDAN Adwa Edaga Hamus Koraro Maychew Feresmay Afeshum Kafta Humera North Western Wukro Adwa Hahayle Selekleka Akxum Nebelat Tsaeda Emba Shire Embaseneyti Frewoyni Asgede Tahtay Edaga Arbi Mayechew Endabaguna Central Hawzen Atsbi May Kadra Zana Mayknetal Korarit TIGRAY Naeder Endafelasi Hawzen Kelete Western Zana Semema Awelallo Tsimbla Atsibi Adet Adi Remets Keyhe tekli Geraleta Welkait Wukro May Gaba Dima Degua Tsegede Temben Dima Kola Temben Agulae Awra Tselemti Abi Adi Hagere May Tsebri Selam Dansha Tanqua Dansha Melashe Mekelle Tsegede Ketema Nigus Abergele AFAR Saharti Enderta Gijet AMHARA Mearay South Eastern Adi Gudom Hintalo Samre Hiwane Samre Wajirat Selewa Town Accessible areas Emba Alaje Regional Capital Bora Partially accessible areas Maychew Zonal Capital Mokoni Neqsege Endamehoni Raya Azebo Woreda Capital Hard to reach areas Boundary Accessible roads Southern Chercher International Zata Oa Partially accessible roads Korem N Chercher Region Hard to reach roads Alamata Zone Raya Alamata Displacement trends 50 Km Woreda The boundaries and names shown and the designations used on this map do not imply official endorsement or acceptance by the United Nations. Creation date: 31 May 2021 Sources: OCHA, Tigray Statistical Agency, humanitarian partners Feedback: [email protected] http://www.humanitarianresponse.info/operations/ethiopia www.reliefweb.int. -

Investigating the Potential of Ancient Religious Sites in the Ethiopian Orthodox Tewhido Church for Religious Tourism Development: the Case of Kirstos Semra
International Journal of Religious Tourism and Pilgrimage Volume 8 Issue 4 Article 7 2020 Investigating the Potential of Ancient Religious Sites in the Ethiopian Orthodox Tewhido Church for Religious Tourism Development: The Case of Kirstos Semra Dagnachew Nega Debre Tabor University, [email protected] Follow this and additional works at: https://arrow.tudublin.ie/ijrtp Part of the Tourism and Travel Commons Recommended Citation Nega, Dagnachew (2020) "Investigating the Potential of Ancient Religious Sites in the Ethiopian Orthodox Tewhido Church for Religious Tourism Development: The Case of Kirstos Semra," International Journal of Religious Tourism and Pilgrimage: Vol. 8: Iss. 4, Article 7. doi:https://doi.org/10.21427/258d-hh58 Available at: https://arrow.tudublin.ie/ijrtp/vol8/iss4/7 Creative Commons License This work is licensed under a Creative Commons Attribution-No Derivative Works 3.0 License. © International Journal of Religious Tourism and Pilgrimage ISSN : 2009-7379 Available at: http://arrow.tudublin.ie/ijrtp/ Volume 8(iv) 2020 Investigating the Potential of Ancient Religious Sites in the Ethiopian Orthodox Tewhido Church for Religious Tourism Development: The Case of Kirstos Semra Dagnachew Nega Debre Tabor University [email protected] Though Ethiopia is endowed with a variety of religious tourism, its potential hasn’t been outlined, managed and used for the development of tourism. Kirstos Semra and its surroundings is one of the most outstanding sites and this study has a general objective of assessing the potential of the site and its surroundings for religious tourism. Descriptive design is employed as a methodology; to collect data, both primary and secondary sources are employed. -

Mekelle, Ethiopia Potential Opportunities for Investors June 2010
Mekelle, Ethiopia Potential opportunities for investors June 2010 KPMG INTERNATIONAL 2 Mekelle, Ethiopia: Potential Opportunities for Investment Terms of reference This report has been prepared by KPMG in Russia, a partnership registered in Russia and a member firm of KPMG International, a Swiss cooperative. The information contained herein is of a general nature and is not intended to address the circumstances of any particular individual or entity. Although we endeavour to provide accurate and timely information, there can be no guarantee that such information is accurate as at the date it is received or that it will continue to be accurate in the future. In preparing this document we have relied upon and assumed, without independent verification, the accuracy and completeness of various sources of information, including public sources. Details of the sources we have used are given in our report. KPMG in Russia accepts no responsibility or liability to any party in connection with such information or views. Our core fieldwork and research were performed between September 2009 and December 2009. We have not undertaken to update our report for events or circumstances arising after that date. Appropriate professional advice should be sought to undertake a more specific examination of the particular circumstances applicable to a potential investor. The contact details of KPMG professionals who can assist in this regard are given at the end of this report. Acknowledgments KPMG in Russia would like to thank the Millennium Cities Initiative (MCI) for the opportunity to prepare this report to support its valuable project. We would also like to thank the numerous enterprises and organisations which participated and acknowledge their contribution to the preparation of this report (please see Appendix 1 for more details).