Antioxidant and Antimicrobial Activity of Solvent Fractions of Calpurnia Aurea (Ait.) Benth
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
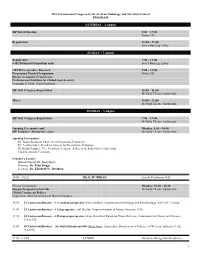
2011 Sip Meeting at a Glance
2011 International Congress on Invertebrate Pathology and Microbial Control PROGRAM SATURDAY – 6 August SIP Board Meeting 8:00 – 17:00 Sobey 153 Registration 18:00 – 21:00 Sobey Building Lobby SUNDAY – 7 August Registration 7:00 – 12:00 (OECD-funded Symposium only) Sobey Building Lobby OECD Co-operative Research 9:00 – 18:00 Programme Funded Symposium: Sobey 255 Disease in Aquatic Crustaceans: Problems and Solutions for Global Food Security Organizer & Chair: Grant Stentiford SIP 2011 Congress Registration 16:00 – 21:00 McNally Theatre Auditorium Mixer 18:00 – 21:00 McNally Theatre Auditorium MONDAY – 8 August SIP 2011 Congress Registration 7:00 – 17:00 McNally Theatre Auditorium Opening Ceremonies and Monday, 8:30 – 10:00 SIP Founders’ Memorial Lecture McNally Theatre Auditorium Opening Ceremonies Dr. Susan Bjornson, Chair, Local Organizing Committee Dr. Leellen Solter, President, Society for Invertebrate Pathology Dr David Gauthier, Vice President Academic & Research, Saint Mary’s University Student Awards Ceremony Founder’s Lecture Introduction by Dr. Harry Kaya Honoree: Dr. John Briggs Lecturer: Dr. Elizabeth W. Davidson 10:00 – 10:25 HEALTH BREAK Loyola Conference Hall Plenary Symposium Monday, 10:30 – 12:30 Disease Perspectives from the McNally Theatre Auditorium Global Crustacean Fishery Organizers: Grant Stentiford and Martin Erlandson 10:30 1 Crustacean diseases – A Canadian perspective Rick Cawthorn. Department of Pathology and Microbiology, AVCLSC, Canada 11:00 2 Crustacean diseases – A US perspective Jeff Shields. Virginia Institute of Marine Sciences, USA 11:30 3 Crustacean diseases – A European perspective Grant Stentiford. European Union Reference Laboratory for Crustacean Diseases, Cefas, UK 12:00 4 Crustacean Diseases – An Australian perspective Brian Jones. -

Oberholzeria (Fabaceae Subfam. Faboideae), a New Monotypic Legume Genus from Namibia
RESEARCH ARTICLE Oberholzeria (Fabaceae subfam. Faboideae), a New Monotypic Legume Genus from Namibia Wessel Swanepoel1,2*, M. Marianne le Roux3¤, Martin F. Wojciechowski4, Abraham E. van Wyk2 1 Independent Researcher, Windhoek, Namibia, 2 H. G. W. J. Schweickerdt Herbarium, Department of Plant Science, University of Pretoria, Pretoria, South Africa, 3 Department of Botany and Plant Biotechnology, University of Johannesburg, Johannesburg, South Africa, 4 School of Life Sciences, Arizona a11111 State University, Tempe, Arizona, United States of America ¤ Current address: South African National Biodiversity Institute, Pretoria, South Africa * [email protected] Abstract OPEN ACCESS Oberholzeria etendekaensis, a succulent biennial or short-lived perennial shrublet is de- Citation: Swanepoel W, le Roux MM, Wojciechowski scribed as a new species, and a new monotypic genus. Discovered in 2012, it is a rare spe- MF, van Wyk AE (2015) Oberholzeria (Fabaceae subfam. Faboideae), a New Monotypic Legume cies known only from a single locality in the Kaokoveld Centre of Plant Endemism, north- Genus from Namibia. PLoS ONE 10(3): e0122080. western Namibia. Phylogenetic analyses of molecular sequence data from the plastid matK doi:10.1371/journal.pone.0122080 gene resolves Oberholzeria as the sister group to the Genisteae clade while data from the Academic Editor: Maharaj K Pandit, University of nuclear rDNA ITS region showed that it is sister to a clade comprising both the Crotalarieae Delhi, INDIA and Genisteae clades. Morphological characters diagnostic of the new genus include: 1) Received: October 3, 2014 succulent stems with woody remains; 2) pinnately trifoliolate, fleshy leaves; 3) monadel- Accepted: February 2, 2015 phous stamens in a sheath that is fused above; 4) dimorphic anthers with five long, basifixed anthers alternating with five short, dorsifixed anthers, and 5) pendent, membranous, one- Published: March 27, 2015 seeded, laterally flattened, slightly inflated but indehiscent fruits. -

Fruits and Seeds of Genera in the Subfamily Faboideae (Fabaceae)
Fruits and Seeds of United States Department of Genera in the Subfamily Agriculture Agricultural Faboideae (Fabaceae) Research Service Technical Bulletin Number 1890 Volume I December 2003 United States Department of Agriculture Fruits and Seeds of Agricultural Research Genera in the Subfamily Service Technical Bulletin Faboideae (Fabaceae) Number 1890 Volume I Joseph H. Kirkbride, Jr., Charles R. Gunn, and Anna L. Weitzman Fruits of A, Centrolobium paraense E.L.R. Tulasne. B, Laburnum anagyroides F.K. Medikus. C, Adesmia boronoides J.D. Hooker. D, Hippocrepis comosa, C. Linnaeus. E, Campylotropis macrocarpa (A.A. von Bunge) A. Rehder. F, Mucuna urens (C. Linnaeus) F.K. Medikus. G, Phaseolus polystachios (C. Linnaeus) N.L. Britton, E.E. Stern, & F. Poggenburg. H, Medicago orbicularis (C. Linnaeus) B. Bartalini. I, Riedeliella graciliflora H.A.T. Harms. J, Medicago arabica (C. Linnaeus) W. Hudson. Kirkbride is a research botanist, U.S. Department of Agriculture, Agricultural Research Service, Systematic Botany and Mycology Laboratory, BARC West Room 304, Building 011A, Beltsville, MD, 20705-2350 (email = [email protected]). Gunn is a botanist (retired) from Brevard, NC (email = [email protected]). Weitzman is a botanist with the Smithsonian Institution, Department of Botany, Washington, DC. Abstract Kirkbride, Joseph H., Jr., Charles R. Gunn, and Anna L radicle junction, Crotalarieae, cuticle, Cytiseae, Weitzman. 2003. Fruits and seeds of genera in the subfamily Dalbergieae, Daleeae, dehiscence, DELTA, Desmodieae, Faboideae (Fabaceae). U. S. Department of Agriculture, Dipteryxeae, distribution, embryo, embryonic axis, en- Technical Bulletin No. 1890, 1,212 pp. docarp, endosperm, epicarp, epicotyl, Euchresteae, Fabeae, fracture line, follicle, funiculus, Galegeae, Genisteae, Technical identification of fruits and seeds of the economi- gynophore, halo, Hedysareae, hilar groove, hilar groove cally important legume plant family (Fabaceae or lips, hilum, Hypocalypteae, hypocotyl, indehiscent, Leguminosae) is often required of U.S. -

Reconstructing the Deep-Branching Relationships of the Papilionoid Legumes
SAJB-00941; No of Pages 18 South African Journal of Botany xxx (2013) xxx–xxx Contents lists available at SciVerse ScienceDirect South African Journal of Botany journal homepage: www.elsevier.com/locate/sajb Reconstructing the deep-branching relationships of the papilionoid legumes D. Cardoso a,⁎, R.T. Pennington b, L.P. de Queiroz a, J.S. Boatwright c, B.-E. Van Wyk d, M.F. Wojciechowski e, M. Lavin f a Herbário da Universidade Estadual de Feira de Santana (HUEFS), Av. Transnordestina, s/n, Novo Horizonte, 44036-900 Feira de Santana, Bahia, Brazil b Royal Botanic Garden Edinburgh, 20A Inverleith Row, EH5 3LR Edinburgh, UK c Department of Biodiversity and Conservation Biology, University of the Western Cape, Modderdam Road, \ Bellville, South Africa d Department of Botany and Plant Biotechnology, University of Johannesburg, P. O. Box 524, 2006 Auckland Park, Johannesburg, South Africa e School of Life Sciences, Arizona State University, Tempe, AZ 85287-4501, USA f Department of Plant Sciences and Plant Pathology, Montana State University, Bozeman, MT 59717, USA article info abstract Available online xxxx Resolving the phylogenetic relationships of the deep nodes of papilionoid legumes (Papilionoideae) is essential to understanding the evolutionary history and diversification of this economically and ecologically important legume Edited by J Van Staden subfamily. The early-branching papilionoids include mostly Neotropical trees traditionally circumscribed in the tribes Sophoreae and Swartzieae. They are more highly diverse in floral morphology than other groups of Keywords: Papilionoideae. For many years, phylogenetic analyses of the Papilionoideae could not clearly resolve the relation- Leguminosae ships of the early-branching lineages due to limited sampling. -

Rbcl and Legume Phylogeny, with Particular Reference to Phaseoleae, Millettieae, and Allies Tadashi Kajita; Hiroyoshi Ohashi; Yoichi Tateishi; C
rbcL and Legume Phylogeny, with Particular Reference to Phaseoleae, Millettieae, and Allies Tadashi Kajita; Hiroyoshi Ohashi; Yoichi Tateishi; C. Donovan Bailey; Jeff J. Doyle Systematic Botany, Vol. 26, No. 3. (Jul. - Sep., 2001), pp. 515-536. Stable URL: http://links.jstor.org/sici?sici=0363-6445%28200107%2F09%2926%3A3%3C515%3ARALPWP%3E2.0.CO%3B2-C Systematic Botany is currently published by American Society of Plant Taxonomists. Your use of the JSTOR archive indicates your acceptance of JSTOR's Terms and Conditions of Use, available at http://www.jstor.org/about/terms.html. JSTOR's Terms and Conditions of Use provides, in part, that unless you have obtained prior permission, you may not download an entire issue of a journal or multiple copies of articles, and you may use content in the JSTOR archive only for your personal, non-commercial use. Please contact the publisher regarding any further use of this work. Publisher contact information may be obtained at http://www.jstor.org/journals/aspt.html. Each copy of any part of a JSTOR transmission must contain the same copyright notice that appears on the screen or printed page of such transmission. The JSTOR Archive is a trusted digital repository providing for long-term preservation and access to leading academic journals and scholarly literature from around the world. The Archive is supported by libraries, scholarly societies, publishers, and foundations. It is an initiative of JSTOR, a not-for-profit organization with a mission to help the scholarly community take advantage of advances in technology. For more information regarding JSTOR, please contact [email protected]. -

Wasps and Bees in Southern Africa
SANBI Biodiversity Series 24 Wasps and bees in southern Africa by Sarah K. Gess and Friedrich W. Gess Department of Entomology, Albany Museum and Rhodes University, Grahamstown Pretoria 2014 SANBI Biodiversity Series The South African National Biodiversity Institute (SANBI) was established on 1 Sep- tember 2004 through the signing into force of the National Environmental Manage- ment: Biodiversity Act (NEMBA) No. 10 of 2004 by President Thabo Mbeki. The Act expands the mandate of the former National Botanical Institute to include respon- sibilities relating to the full diversity of South Africa’s fauna and flora, and builds on the internationally respected programmes in conservation, research, education and visitor services developed by the National Botanical Institute and its predecessors over the past century. The vision of SANBI: Biodiversity richness for all South Africans. SANBI’s mission is to champion the exploration, conservation, sustainable use, appreciation and enjoyment of South Africa’s exceptionally rich biodiversity for all people. SANBI Biodiversity Series publishes occasional reports on projects, technologies, workshops, symposia and other activities initiated by, or executed in partnership with SANBI. Technical editing: Alicia Grobler Design & layout: Sandra Turck Cover design: Sandra Turck How to cite this publication: GESS, S.K. & GESS, F.W. 2014. Wasps and bees in southern Africa. SANBI Biodi- versity Series 24. South African National Biodiversity Institute, Pretoria. ISBN: 978-1-919976-73-0 Manuscript submitted 2011 Copyright © 2014 by South African National Biodiversity Institute (SANBI) All rights reserved. No part of this book may be reproduced in any form without written per- mission of the copyright owners. The views and opinions expressed do not necessarily reflect those of SANBI. -

Extraction of Calpurnia Aurea (CA) Root Phytochemical Screening for Detection and Usage of Glycosides
Extraction of Calpurnia aurea (CA) root phytochemical screening for detection and usage of glycosides 1 * 3 Dr A Sri Pavan Kumar, 2 Dr. R. Suryanarayana Raju, Mr Nageswara Rao 1Department of SPM, 2,3Department of Pharmacology, 1,2,3Konaseema Institute of medical Sciences Research Foundation, Amalapuram, Andhra Pradesh, India *corresponding author: [email protected] ( Raju) Abstract In Ethiopia, Calpurnia aurea (CA) is utilized for several diseases like syphilis, malaria, rabies, diabetes ect. Researchers assessed the photochemical screening like flavoides, saponins glycosides ect., are used for standard methods in vitro antioxidant properties that are screened by DPPH. Calpurnia aura leaves are dried seeds that are collected by south Gondar, northern Ethiopia collets the plant materials that are dried and powdered utilizing electric grinder. Here major part of CA are utilized in pharmaceutical industry for the evidence of study by highest therapeutic efficiency processing by major metabolic classes contains more alkaloids and tannins of CA leaves. Here many medical plants are helpful for healing and curing human disease on the presence of phytochemical constituents so it is used in many Auyurvedic medicines. This is safe, less toxic, economical and reliable under indigenous systems of medicine. Keywords: CA; phytochemicals; Screening of Phytochemical; Qualitative examination; Standard approaches How to cite this article: Kumar SP, Raju RS, Rao N (2020): Extraction of calpurnia aurea (CA) root phytochemical screening for detection of glycoside, Ann Trop Med and Public Health; 23(S21): SP231931. DOI: http://doi.org/10.36295/ASRO.2020.231931 1 Introduction So as to advance home grown medications, there is an earnest need to assess the restorative possibilities of the medications according to WHO rules and referenced that 30% of the overall deals of medications depends on characteristic products1. -

Innovative Agricultural Approaches of Promoting Food Security in Eritrea: Trends, Challenges and Opportunities for Growth
AEAS / ESAPP / SLM Eritrea Joint Report Innovative Agricultural Approaches of Promoting Food Security in Eritrea: Trends, Challenges and Opportunities for Growth Proceedings of the Workshop of the Association of Eritreans in Agricultural Sciences (AEAS) 2 – 3 March 2006 Asmara, Eritrea | downloaded: 13.3.2017 Editors: Bissrat Ghebru and Tadesse Mehari 2007 https://doi.org/10.7892/boris.71045 source: A ESAPP E A S Innovative Agricultural Approaches of Promoting Food Security in Eritrea: Trends, Challenges and Opportunities for Growth Innovative Agricultural Approaches of Promoting Food Security in Eritrea: Trends, Challenges and Opportunities for Growth Proceedings of the Workshop of the Association of Eritreans in Agricultural Sciences (AEAS) 2-3 March 2006 Asmara, Eritrea Editors: Bissrat Ghebru and Tadesse Mehari Publisher: Geographica Bernensia Bern, 2007 Citation: Bissrat Ghebru and Tadesse Mehari (Editors) 2007 Innovative Agricultural Approaches of Promoting Food Security in Eritrea: Trends, Challenges and Opportunities for Growth. Proceedings of the Workshop of the Association of Eritreans in Agricultural Sciences (AEAS), 2-3 March, Asmara, Eritrea Bern, Geographica Bernensia, 169pp. SLM Eritrea, and ESAPP, Syngenta Foundation for Sustainable Agriculture, and Centre for Development and Environment (CDE), University of Bern, 2007 Publisher: Geographica Bernensia Printed by: Varicolor, Switzerland Copyright© 2007 by: Association of Eritreans in Agricultural Sciences (AEAS) This publication was prepared with support from: Eastern and -

Wood Anatomy of Cyathostegia Mathewsii
IAWA Journal, Vol. 22 (2), 2001: 193–199 WOOD ANATOMY OF CYATHOSTEGIA MATHEWSII (SWARTZIEAE, PAPILIONOIDEAE, LEGUMINOSAE) by Peter Gasson & Elspeth J. Wray Royal Botanic Gardens, Kew, Richmond, Surrey, TW9 3AB, United Kingdom SUMMARY The genus Cyathostegia consists of one or possibly two species from Ecuador and Peru. The wood anatomy of C. mathewsii (Benth.) Schery is described, thereby completing generic coverage of wood anatomy in the tribe Swartzieae sensu Polhill (1994b). In Cyathostegia, vessels are mainly in radial multiples, axial parenchyma is relatively sparse, storied and mainly paratracheal, and rays are 1–2-seriate and irregularly storied. Its wood anatomy is compared with that of other genera in the closely related tribes Sophoreae and Swartzieae, both of which have included Cyathostegia. The similarities and differences between Cyathostegia, Ateleia and Amburana are emphasised. Key words: Amburana, Ateleia, Cyathostegia, Sophoreae, Swartzieae. INTRODUCTION Cyathostegia comprises one, or possibly two species of shrubs or small trees in Ecua- dor and Peru. Wood specimens of this genus were unavailable for previous studies of Sophoreae (Gasson 1994) and Swartzieae (Gasson 1996), and no published informa- tion on the wood anatomy of this genus could be found. A wood sample of Cyathoste- gia mathewsii has recently been collected in Ecuador, allowing us to provide a wood description and compare the wood anatomy of the genus with other Sophoreae and Swartzieae. Generic descriptions of the tribe Swartzieae as circumscribed by Polhill (1994b) are now complete (Gasson 1994, 1996; Gasson & Webley 1999). Polhill (1981) associated Cyathostegia with seven other genera of Sophoreae in the Myroxy- lon group. The closest relative of Cyathostegia is considered to be Ateleia (e.g. -

A New Subfamily Classification of The
LPWG Phylogeny and classification of the Leguminosae TAXON 66 (1) • February 2017: 44–77 A new subfamily classification of the Leguminosae based on a taxonomically comprehensive phylogeny The Legume Phylogeny Working Group (LPWG) Recommended citation: LPWG (2017) This paper is a product of the Legume Phylogeny Working Group, who discussed, debated and agreed on the classification of the Leguminosae presented here, and are listed in alphabetical order. The text, keys and descriptions were written and compiled by a subset of authors indicated by §. Newly generated matK sequences were provided by a subset of authors indicated by *. All listed authors commented on and approved the final manuscript. Nasim Azani,1 Marielle Babineau,2* C. Donovan Bailey,3* Hannah Banks,4 Ariane R. Barbosa,5* Rafael Barbosa Pinto,6* James S. Boatwright,7* Leonardo M. Borges,8* Gillian K. Brown,9* Anne Bruneau,2§* Elisa Candido,6* Domingos Cardoso,10§* Kuo-Fang Chung,11* Ruth P. Clark,4 Adilva de S. Conceição,12* Michael Crisp,13* Paloma Cubas,14* Alfonso Delgado-Salinas,15 Kyle G. Dexter,16* Jeff J. Doyle,17 Jérôme Duminil,18* Ashley N. Egan,19* Manuel de la Estrella,4§* Marcus J. Falcão,20 Dmitry A. Filatov,21* Ana Paula Fortuna-Perez,22* Renée H. Fortunato,23 Edeline Gagnon,2* Peter Gasson,4 Juliana Gastaldello Rando,24* Ana Maria Goulart de Azevedo Tozzi,6 Bee Gunn,13* David Harris,25 Elspeth Haston,25 Julie A. Hawkins,26* Patrick S. Herendeen,27§ Colin E. Hughes,28§* João R.V. Iganci,29* Firouzeh Javadi,30* Sheku Alfred Kanu,31 Shahrokh Kazempour-Osaloo,32* Geoffrey C. -
![Common Calpurnia[E] Geelkeur[A](https://docslib.b-cdn.net/cover/6493/common-calpurnia-e-geelkeur-a-5006493.webp)
Common Calpurnia[E] Geelkeur[A
Common Calpurnia [E] Geelkeur [A] Natal Laburnum [E] insiphane-enkhulu [Z] umDlovana [Z] umLalandlovana [Z] umbethe [X] umbhaleni [X] umhlahlambedu [Z] umkhiphampethu [Z] undlole [X] FABACEAE Calpurnia aurea Type: Shrub. Source: Endemic. Flower: Yellow. November until February. Fruit: Brown. November until February. Leaves: Evergreen with Green leaves. Biological Characteristics Crown density: Light. Crown formation: rounded. Growth rate: Medium. Maximum height: 10.00m. Management Dormancy season: Winter. Water requirement: Water when soil dry. Soil Requirements Drainage requirements: Normal. Preferred growing medium: Bark:Riversand:Soil 1:1:1. Preferred soil type: Sandy well drained soil rich in humus. Habits: Shrub. Habitats: Broad-leaved Woodland, Cliffs, Coastal Forest, Escarpment Forest, Valley Bushveld. Propagation methods: Seed (Hard). Sun Requirements: Sun. References:Palgrave, Keith Coates revised by Meg "Trees of Southern Africa" Struik (2002), Page 355 Pooley, Elsa "The Complete Field Guide to Trees of Natal Zululand and Transkei" Natal Flora Publication Trust (1993), Page 158 About the Plant This is one of our easiest shrubs to grow in gardens. It is ideally suited to the small gardens of modern city living. It likes a fairly sheltered but sunny spot in the garden and will delight you with its masses of yellow pea flowers in about three years from seed Anyone can grow this plant. Collect a dry seed pod from a shrub near you split open the pod, remove the amber coloured seeds about the size of a book-match head. Sow the seeds in a mixture of river sand and potting soil to the proportion of 1:1, keep the container in a sunny spot. -

Phytochemical Screening of the Leaves Calpurnia Aurea (Ait.) Benth Extract
International Journal of Clinical Chemistry and Laboratory Medicine (IJCCLM) Volume 5, Issue 4, 2019, PP 18-24 ISSN No. (Online) 2455-7153 DOI: http://dx.doi.org/10.20431/2455-7153.0504004 www.arcjournals.org Phytochemical Screening of the Leaves Calpurnia Aurea (Ait.) Benth Extract Hadera Brhane Gebreslassie1*, Alemseged Eyasu1 1Department of Chemistry, abbiy addi College of teacher education & Educational leadership, Abbiy Addi, Tigray Region, Ethiopia. *Corresponding Author: Hadera Brhane Gebreslassie, Department of Chemistry, abbiy addi College of teacher education & Educational leadership, Abbiy Addi, Tigray Region, Ethiopia. Abstract Background: Calpurnia aurea is a genus of Flowering Plants within the family of fabaceae. Calpurnia aurea from Ethiopia is known locally as "digitta" (Amharic),"ሕፃውፅ-Hitsawits" (Tigrigna). In native countries like Ethiopia, traditionally, the leave of Calpurnia aurea is used for the treatment of syphilis, malaria, rabies, diabetes, lung TB, hypertension, diarrhoea, stomach-ache, bowel, bladder disorders, to induce uterine contractions, tapeworm, trachoma, ringworm, as well as vomiting, Dandruff, headache, eye diseases, to destroy maggots, to destroy bedbugs, to relieve itches, used as a fish-poison or as a cure for dysentery, cough and snake bite. Objective: The main purpose of this study was interested to investigate the phytochemical analysis of the leaves extracts Calpurnia aurea. Methods: Calpurnia aurea leaves were collected from around debrekerbe kebele, medebay zana wereda and north western Zone of Tigray Region, Northern Ethiopia. The collected plant material was dried and powdered using mortar and pestle and then extracted using serial exhaustive solvent extraction methods within four organic solvents: petroleum ether, chloroform, ethyl acetate and ethanol according to their increasing polarity index for 72 hours with mechanical shaking within 4 hours interval in average and it was filtered through Whatman No.1 filter paper and the filtrate was dried using Rotary evaporator.