Breakthroughs Annual Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Facts and Figures 2010 Facts.Med.Yale.Edu
Clinical overview patient care Medical center medical center New Haven yale university and new haven Endowment finance institutions Income $390.6 million§ More than 800 Yale physicians provide primary An affiliation agreement between the medical Population The School of Medicine is located immedi- (6/30/09) The School of Medicine had operating income Yale School (2009) 127,401 Clinical departments 18 and specialty care for patients through Yale school and Grace-New Haven Hospital in ately adjacent to the main campus of Yale Yale $16.1 billion of $1,076.6 million in 2009. A total of $557.9 of Medicine Distance from: Yale Medical Group Medical Group. Yale Medical Group delivers 1965 created Yale-New Haven Hospital, which University, one of the world’s great institu- YSM $1.4 billion million was awarded in sponsored research Yale Cancer Center NYC 80 miles Office visits advanced care in more than 160 specialties and expanded in 1993 with the opening of the tions of higher learning. With a residential agreements, of which $466.0 million was Boston 137 miles 2009 capital projects 323,532 subspecialties, and has centers of excellence in Yale Child Children’s Hospital and again in 2000 with college system modeled after those of Cam- received and spent during the fiscal year. The Study Center (in millions) Patient encounters such fields as cancer, cardiac care, minimally the acquisition of the Psychiatric Hospital. The University profile bridge and Oxford, the undergraduate school school ranked fifth among medical schools re- Yale Medical Group NEW CONSTRUCTION 1,331,353 invasive surgery, and organ transplantation. -

From Bench to Bedside and Back
From Bench to Bedside and Back spring | summer 2014 contents spring | summer 2014 10 4 8 features departments 2 What if you were the patient? 1 Director’s Letter Clinicians redesign care. 7 Advances 4 From Bench to Bedside and Back Breakthrough research from Yale Cancer Center The rallying cry at Yale Cancer Center is “translational medicine.” 8 Forefront Cancer Center chosen for groundbreaking study 10 Arming the Immune System to Fight Back against Cancer 12 Prevention Bill Brown’s success story. Millions of lives saved by surgeon general’s report on smoking but the fight isn’t over 14 Giving High-risk, high-reward fund aims to accelerate cancer research 16 Meet the Physician Q&A with Dr. Steven Gore On the Cover 17 New Faces Dr. Lajos Pusztai, Director of Breast Appointments at Yale Cancer Center Medical Oncology and Co-Director of Cancer Genetics and Genomics, with Dr. Anees Chagpar, Director of the Breast Center at Smilow Cancer Hospital at Yale-New Haven. Peter Baker photographer director’s letter yale cancer center Thomas J. Lynch, Jr., MD Director Kevin Vest, MBA, FACHE Deputy Director, Administration and Clinical Affairs Renee Gaudette Director, Public Affairs and Marketing art + production Greg Mursko Creative Director contributors Writers Emily Fenton Steve Kemper Colleen Shaddox Photographer Peter Baker pbakerphoto.com Design Peter Baker Studios www.pbakerstudios.com Yale Cancer Center and Smilow Cancer Hospital at Yale-New Haven have joined the National Comprehensive Cancer Network (NCCN) with official acceptance into the organization at their annual submit your ideas... Do you have an idea for a story meeting in March. -

Facts and Figures 2009
Medical center medical center New Haven yale university and new haven Endowment finances institutions An affiliation agreement between the Population The School of Medicine is located immedi- (6/30/08) The School of Medicine had operating Yale School medical school and Grace-New Haven (2007) 130,625 ately adjacent to the main campus of Yale Yale $22.7 billion income of $988.6 million in 2008. A total of Medicine Hospital in 1965 created Yale-New Haven Distance from: University, one of the world’s great institu- YSM $1.9 billion of $511.6 million was awarded in sponsored Yale Cancer Center NYC 80 miles Hospital, which expanded in 1993 with tions of higher learning. With a residential 2008 capital projects research agreements, of which $442.1 Yale Child the opening of the Children’s Hospital and Boston 137 miles college system modeled after those of (in millions) million was received and spent during Study Center again in 2000 with the acquisition of the University profile Cambridge and Oxford, the undergraduate NEW CONSTRUCTION the fiscal year. The school ranked fifth Yale Medical Group Psychiatric Hospital. The 14-story Smilow FACULTY school is complemented by the Graduate Yale $146.60 among medical schools receiving research Yale School of Cancer Hospital will open in fall 2009. The Yale 3,619 School of Arts and Sciences; and 12 profes- YSM $13.81 funding from the NIH in 2008 and first in Public Health YSM 1,971 medical campus has grown over the years sional schools, including Architecture, Art, RENOVATION & ALTERATION NIH grants per faculty member. -

March 5, 2021
March 5, 2021 from the desk of Nita Ahuja, MD, MBA, FACS Announcements Interim Director, Yale Cancer Center Interim Physician-in-Chief, Smilow Cancer Hospital Chênevert Family Brain Tumor Center Launched at Yale We are proud to announce a gift to establish the Chênevert Family Brain Tumor Center at Yale Cancer Center. The Chênevert Family Brain Tumor Center will be a leading center in Neuro-Oncology research worldwide, bringing ground- breaking solutions and hope to patients with brain tumors. The Center’s vision is to promote discoveries and advance meaningful scientific innovations that set new standards for the diagnosis, treatment, and care for patients with brain tumors. “As a survivor of Stage 4 CNS Lymphoma, our family is thankful for the great care provided by doctors and staff at Yale during my battle. I am News Center fortunate that now I can give back personally and through our Foundation to change the outcome and cure for others affected by Yale Researchers Identify Tumor Reactive brain cancer,” Louis Chênevert said. Mr. Chênevert serves as Immune Cells to Help Fight Against Advanced Chairman of the Yale Cancer Center Director’s Advisory Board. Melanoma Elizabeth Herbert Hired as Vice President for Network Services Please welcome Elizabeth Herbert, Vice President for Network Services, to Smilow Cancer Hospital and Yale Cancer Center. Liz joined us earlier this week from Memorial Sloan Kettering (MSK) Cancer Center where she most recently served as a Senior Vice President in Hospital Administration. In this role, she had administrative oversight of six academic departments at MSK and served as an executive sponsor to numerous improvement projects. -

February 5, 2021 from the Desk of Charles S
February 5, 2021 from the desk of Charles S. Fuchs, MD, MPH Announcements Director, Yale Cancer Center and Physician-in-Chief Smilow Cancer Hospital Annual Award Winners Celebrated at Virtual Conclave Yale Cancer Center’s annual Conclave was celebrated virtually on Tuesday, January 26 to honor the great scientific and clinical accomplishments of 2020, and to underscore the devotion of our scientists, physicians, providers, and staff through an unprecedented and challenging year. David Fischer, MD, was presented with the Yale Cancer Center News Center Lifetime Achievement Award by Vincent T. DeVita, Jr., MD. Dr. Fischer was the first medical oncologist to practice in New Haven, A closer look at the impact of COVID-19 on beginning in 1967, and as Dr. DeVita stated, “his fingerprints are all cardio-oncology over just about everything cancer-related in Connecticut since.” Dr. Fischer wrote and published the first Cancer Chemotherapy Handbook, along with Tish Knobf, RN, PhD, and he later published a formative paper in the Journal of Clinical Oncology to improve the chemotherapy treatment process and safety for patients. He was on the committee to help establish The Connecticut Hospice, the first hospice in the country and continued to be actively involved throughout his career. In 1994, he joined Yale Cancer Center and began his service as Vice-Chair of the Cancer Committee in 1996. Dr. DeVita summarized his remarks stating, “David has been an effective and Read More tireless advocate for Yale Cancer Center, including for the new building [Smilow Cancer Hospital].” Please take a moment to watch accolades Yale Cancer Center Study Shows Aspirin & shared from others in gratitude of Dr. -

June 24, 2016
June 24, 2016 Announcements T-TARE Awarded to Head & Neck Cancers Program A new Translational Targeted Area of Research Excellence (T-TARE) grant has been awarded to the Head & Neck Cancers Program, led by Dr. Barbara Burtness and Dr. Wendell Yarbrough, to support their translational research efforts. Under the direction of Roy Herbst, MD, PhD, Associate Director for Translational Research, T-TARE Grants at Yale Cancer Center are institutionally supported with the express purpose of developing translational research programs for patient care a to promote multi-investigator grant submissions to the National Cancer Institute, such as program project grants or SPORE grants. Drs. Burtness and Yarbrough are actively working on a SPORE submission for Head and Neck Cancers to the NCI and the T-TARE grant funding will provide the resources needed to fund pilot projects and team science to strengthen their application. For more information about the T-TARE program, please contact Dr. Herbst or Ed Kaftan, PhD, Associate Director for Translational Research Administration. Recent News New Funding to Research Cancers in HIV+ Patients Read recent articles featuring experts I am pleased to announce that Dr. Walther Mothes, Co- from Yale Cancer Center Director of the Virus and Other Infection-Associated News Center >> Cancers Research Program, has received funding to support his application to the NCI for the "Yale Cancer Center pilot program to stimulate research in non-AIDS defining cancers in aging HIV+populations." The LATEST ARTICLES: application will create Yale Cancer Center pilot grants to stimulate research in non-AIDS defining cancers in aging HIV+ populations. It aims to increase the basic understanding of the differential behaviors of these cancers and has the potential to significantly alleviate disparities in the treatment of HIV+ cancer patients in New Haven. -

February 9, 2018
February 9, 2018 Announcements New Smilow Immunology Clinic Smilow Cancer Hospital will launch a new clinical program next week for patients experiencing side effects or immune-related adverse events resulting from treatment with immunotherapy. Patients with autoimmune diseases anticipating beginning treatment for cancer are also advised to seek a consultation. Dr. Christina Price, Assistant Professor of Allergy and Clinical Immunology, will lead the clinic and collaborate with each patient's oncologist and care team to ensure streamlined care. The weekly patient clinic will begin on Wednesday mornings on NP8, starting on February 14. For more information, please contact Dr. Price. To refer a patient through EPIC, please use ID#: 45848 Name: YNH Smilow Immunology. The Policy, Politics & Law of Cancer Recent News News Center >> LATEST ARTICLES: I hope many of you will be able to join us today at the Yale Law School for what is expected to be a great event giving us the opportunity to examine the current state of cancer policy and discuss ways in which law can influence its development. There is a full agenda of speakers today, including a keynote presentation by the director of the National Cancer Institute, Dr. Norman Sharpless at 12:45pm. Learn More >> U.S. News Best Hospitals Voting will soon open on Doximity for the annual Best Yale Takes First Look At The Politics Hospitals survey in U.S. News & World Report. All Of Cancer Treatment registered clinicians can login and vote. When voting Read More >> officially opens, we will send a notification to you to prompt you to vote. -

September 4, 2020 from the Desk of Charles S
September 4, 2020 from the desk of Charles S. Fuchs, MD, MPH Director, Yale Cancer Center Announcements and Physician-in-Chief Smilow Cancer Hospital Dr. Elizabeth Berger Joins Breast Center We are pleased to welcome Dr. Elizabeth Berger, Assistant Professor of Surgery (Oncology) to The Breast Center at Smilow Cancer Hospital. Dr. Berger received her Medical Degree from Loyola University Chicago Stritch School of Medicine where she was also a Clinical Research Scholar. She recently completed a fellowship in Breast Surgical Oncology at Memorial Sloan Kettering Cancer Center and was selected as the Breast Cancer Alliance Fellow while at Memorial Sloan Kettering. She received her Master of Science in Health Services and Outcomes Research from Northwestern University and did a General Surgery Residency at Loyola University Medical Center. Dr. Berger was an American College of Surgeons (ACS) Clinical Scholar-in-Residence from 2014 to 2016. Her focus at the ACS was on breast cancer research and outcomes. Her research focuses on improving health outcomes for women with breast cancer, including perioperative surgical quality, cancer care quality measure development, and assessment of national accreditation in breast News Center cancer surgery. Dr. Berger has published in several high impact journals such as JAMA, Annals of Surgery, and the Journal of the 'No One is Immune’: Boseman’s Death Shows American College of Surgeons, as well as contributed chapters to Colon Cancer Affecting Young and Black several surgical textbooks. She has also served on national quality Americans committees, including a member of the National Accreditation Program for Breast Centers (NAPBC). T-TARE Awarded Elias Lolis, PhD, Professor of Pharmacology, has been awarded a Yale Cancer Center T-TARE Award to support his project, “CXCR5- targeted CAR-T for Aggressive T Cell Lymphomas.” In alignment with the collaborative, translational focus of the T-TARE Program, Dr. -

School of Medicine 2020–2021
BULLETIN OF YALE UNIVERSITY BULLETIN OF YALE BULLETIN OF YALE UNIVERSITY Periodicals postage paid New Haven ct 06520-8227 New Haven, Connecticut School of Medicine 2020–2021 School of Medicine 2020–2021 BULLETIN OF YALE UNIVERSITY Series 116 Number 8 July 30, 2020 BULLETIN OF YALE UNIVERSITY Series 116 Number 8 July 30, 2020 (USPS 078-500) The University is committed to basing judgments concerning the admission, education, is published seventeen times a year (one time in October; three times in September; four and employment of individuals upon their qualifications and abilities and a∞rmatively times in June and July; five times in August) by Yale University, 2 Whitney Avenue, New seeks to attract to its faculty, sta≠, and student body qualified persons of diverse back- Haven CT 0651o. Periodicals postage paid at New Haven, Connecticut. grounds. In accordance with this policy and as delineated by federal and Connecticut law, Yale does not discriminate in admissions, educational programs, or employment against Postmaster: Send address changes to Bulletin of Yale University, any individual on account of that individual’s sex, race, color, religion, age, disability, PO Box 208227, New Haven CT 06520-8227 status as a protected veteran, or national or ethnic origin; nor does Yale discriminate on the basis of sexual orientation or gender identity or expression. Managing Editor: Kimberly M. Go≠-Crews University policy is committed to a∞rmative action under law in employment of Editor: Lesley K. Baier women, minority group members, individuals with disabilities, and protected veterans. PO Box 208230, New Haven CT 06520-8230 Inquiries concerning these policies may be referred to Valarie Stanley, Senior Direc- tor of the O∞ce of Institutional Equity and Access, 221 Whitney Avenue, 4th Floor, The closing date for material in this bulletin was June 30, 2020. -

Directconnect Newsletter
June 10, 2016 Announcements Hematology Inpatient Unit Named for Tom Duffy Last week, it was an honor to dedicate the Duffy Hematology Firm at Yale New Haven Hospital. Thomas P. Duffy, MD is highly respected for his dedication and care of his patients, his incredible regard and talent for teaching our housestaff and fellows, and his mentorship at Yale Cancer Center and Yale New Haven Hospital throughout his 40 year career here. Please join me in congratulating Tom on the well-deserved honor of the Duffy Hematology Firm. Justin Blasberg Joins Thoracic Surgery Dr. Justin Blasberg has been appointed an Assistant Professor of Surgery at Yale School of Medicine and is a member of the Thoracic Oncology program at Smilow Cancer Hospital. His practice includes minimally invasive and open management for diseases of the esophagus, lung, mediastinum, chest wall, Recent News thoracic outlet, and Read recent articles featuring experts diaphragm. In addition, he from Yale Cancer Center has a particular interest in benign and malignant News Center >> diseases of the trachea, as well as complex lung resections requiring bronchoplasty. Dr. Blasberg received his undergraduate degree from Binghamton University, his medical degree from Albert Einstein LATEST ARTICLES: College of Medicine, and a master's degree in science from University of Wisconsin School of Medicine and Public Health. Development Update Mary McNiff presented Dr. Harriet Kluger with $26,000 from the Jim McNiff Annual Golf Tournament in support of renal cell cancer research at Yale Cancer Center. Over 100 guests attended the May 16th event. At Yale Cancer Yale Cancer Center researchers win Center we are grateful for the continued generosity of Sokoloff Family-Melanoma Research the McNiff family, friends, and sponsors, which will Alliance team science award help us to pursue new research and treatment options Read More >> for cancer. -

Yale Cancer Center Benefits Doubly from Generosity New Ceowill Lead
march 2013 volume 9, issue 1 Advancing Biomedical Science, Education, and Health Care Yale Cancer Center benefits doubly from generosity United Technologies supports “Smilow Cancer Hospital is now Easing suffering, ‘the power of innovation’ in delivering great service to the com- giving support munity, including utc employees,” Yale’s cancer care and research says Louis Chênevert, chairman and at the end of life ceo of United Technologies. “Our United Technologies Corporation company has a long history of sup- The Palliative Care (utc), a Hartford-based multinational porting leading organizations in our Program at Yale manufacturer and Connecticut’s largest communities, and Yale Cancer Center Cancer Center private employer, has donated $3 mil- is a proven leader.” (ycc) has received Jennifer Kapo lion to establish a new endowed profes- The new professorship, which a $1 million gift sorship at Yale Cancer Center (ycc). will support the full-time research from the Milbank Foundation for The gift, which establishes the activities of a faculty member whose courtesy of united technologies corp Rehabilitation. United Technologies Corporation primary research focus is cancer, is (From left) Mark Reitsma, a utc employee Directed by Jennifer M. Kapo, Professorship in Cancer Research, also part of what Chênevert describes and patient at Smilow Cancer Center, and m.d., associate professor of internal stems from utc’s long-time commit- as utc’s “broader efforts of promot- Louis Chênevert, ceo of utc. medicine and chief of palliative medi- ment to supporting cancer care and ing employee wellness.” to live. And then, at his supervisor’s cine at Smilow Cancer Hospital at research, and represents a deepened Mark Reitsma, utc’s manager of recommendation, he sought a second Yale-New Haven, the Palliative Care commitment by utc to what its lead- Global Human Resources Support opinion at Smilow. -
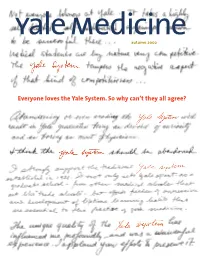
Everyone Loves the Yale System. So Why Can't They All Agree?
yale medicine autumn 2002 Everyone loves the Yale System. So why can’t they all agree? autumn yale medicine 2002CONTENTS 2 Letters 4 Chronicle 12 Rounds 16 Findings 18 Books 19 On Campus 20 Capsule on the cover 22 “A steam engine in pants” When a group of medical students In 1920, Milton Winternitz became dean and ushered in wrote to alumni about exam require- ments earlier this year, they received a new era in medicine at Yale, creating the Yale System in the more than 500 responses, includ- process. For much of his 15 years at the top, what Winternitz ing the testimonials that appear on wanted, Winternitz got. pages 38 to 42. In their letters, By Gerard N. Burrow, m.d. ’58, hs ’66 the majority of those writing recall a Yale System that allowed them the freedom to pursue knowledge 30 Everyone loves the Yale System. independently and instilled a life- So why can’t they all agree? long love of learning. The debate over exams this spring centered on two key questions: how should medicine be taught in the 21st century and how should a student’s progress be measured? By John Curtis 38 The Yale System lives! Long live the Yale System. When nine Yale medical students wrote to 5,000 alumni last winter about changes in the curriculum, they triggered a flood of reminiscences about the experience of becoming a doctor at Yale. 43 Faculty 47 Students 48 Alumni 62 In Memoriam 64 Archives On the Web info.med.yale.edu/ymm On our website, readers can submit class notes or a change of address, check the alumni events calendar, arrange for a lifelong Yale e-mail alias through the virtual Yale Station and search our electronic archive.