Different Dissecting Orders of the Pulmonary Bronchus and Vessels
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nber Working Paper Series the Impact of the General
NBER WORKING PAPER SERIES THE IMPACT OF THE GENERAL DATA PROTECTION REGULATION ON INTERNET INTERCONNECTION Ran Zhuo Bradley Huffaker kc claffy Shane Greenstein Working Paper 26481 http://www.nber.org/papers/w26481 NATIONAL BUREAU OF ECONOMIC RESEARCH 1050 Massachusetts Avenue Cambridge, MA 02138 November 2019 The authors are grateful to the Doctoral Office at Harvard Business School for financial support for field work. This research is partially supported by NSF OAC-1724853, NSF C-ACCEL OIA-1937165, U.S. AFRL FA8750-18-2-0049. The views and conclusions do not necessarily represent those of the Air Force Research Laboratory, the U.S. Government, or the National Bureau of Economic Research. NBER working papers are circulated for discussion and comment purposes. They have not been peer-reviewed or been subject to the review by the NBER Board of Directors that accompanies official NBER publications. © 2019 by Ran Zhuo, Bradley Huffaker, kc claffy, and Shane Greenstein. All rights reserved. Short sections of text, not to exceed two paragraphs, may be quoted without explicit permission provided that full credit, including © notice, is given to the source. The Impact of the General Data Protection Regulation on Internet Interconnection Ran Zhuo, Bradley Huffaker, kc claffy, and Shane Greenstein NBER Working Paper No. 26481 November 2019 JEL No. L00,L51,L86 ABSTRACT The Internet comprises thousands of independently operated networks, where bilaterally negotiated interconnection agreements determine the flow of data between networks. The European Union’s General Data Protection Regulation (GDPR) imposes strict restrictions on processing and sharing of personal data of EU residents. Both contemporary news reports and simple bilateral bargaining theory predict reduction in data usage at the application layer would negatively impact incentives for negotiating interconnection agreements at the internet layer due to reduced bargaining power of European networks and increased bargaining frictions. -

Cultural Assimilation During the Age of Mass Migration*
Cultural Assimilation during the Age of Mass Migration* Ran Abramitzky Leah Boustan Katherine Eriksson Stanford University and NBER UCLA and NBER UC Davis and NBER November 2015 We document that immigrants achieved a substantial amount of cultural assimilation during the Age of Mass Migration, a formative period in US history. Many immigrants learned to speak English, applied for US citizenship, and married spouses from different origins. Immigrants also chose less foreign names for their sons and daughters as they spent more time in the US. Possessing a foreign name had adverse consequences for the children of immigrants. Linking over one million records across historical Censuses, we find that brothers with more foreign names completed fewer years of schooling, were more likely to be unemployed, earned less, and were less likely to work in a white collar occupation. * We are grateful for the access to Census manuscripts provided by Ancestry.com, FamilySearch.org and the Minnesota Population Center. We benefited from the helpful comments we received at the DAE group of the NBER Summer Institute, the Munich “Long Shadow of History” conference, the Irvine conference on the Economics of Religion and Culture, the Cambridge conference on Networks, Institutions and Economic History, the AFD-World Bank Migration and Development Conference, and the Economic History Association. We also thank participants of seminars at Arizona State, Berkeley, Michigan, Ohio State, UCLA, Warwick, Wharton, Wisconsin and Yale. We profited from conversations with Cihan Artunc, Sascha Becker, Hoyt Bleakley, Davide Cantoni, Raj Chetty, Dora Costa, Dave Donaldson, Joe Ferrie, Price Fishback, Avner Greif, Eric Hilt, Naomi Lamoreaux, Victor Lavy, Joel Mokyr, Kaivan Munshi, Martha Olney, Luigi Pascali, Santiago Perez, Hillel Rapoport, Christina Romer, David Romer, Jared Rubin, Fabian Waldinger, Ludger Woessmann, Gavin Wright, and Noam Yuchtman. -
Gateless Gate Has Become Common in English, Some Have Criticized This Translation As Unfaithful to the Original
Wú Mén Guān The Barrier That Has No Gate Original Collection in Chinese by Chán Master Wúmén Huìkāi (1183-1260) Questions and Additional Comments by Sŏn Master Sǔngan Compiled and Edited by Paul Dōch’ŏng Lynch, JDPSN Page ii Frontspiece “Wú Mén Guān” Facsimile of the Original Cover Page iii Page iv Wú Mén Guān The Barrier That Has No Gate Chán Master Wúmén Huìkāi (1183-1260) Questions and Additional Comments by Sŏn Master Sǔngan Compiled and Edited by Paul Dōch’ŏng Lynch, JDPSN Sixth Edition Before Thought Publications Huntington Beach, CA 2010 Page v BEFORE THOUGHT PUBLICATIONS HUNTINGTON BEACH, CA 92648 ALL RIGHTS RESERVED. COPYRIGHT © 2010 ENGLISH VERSION BY PAUL LYNCH, JDPSN NO PART OF THIS BOOK MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM OR BY ANY MEANS, GRAPHIC, ELECTRONIC, OR MECHANICAL, INCLUDING PHOTOCOPYING, RECORDING, TAPING OR BY ANY INFORMATION STORAGE OR RETRIEVAL SYSTEM, WITHOUT THE PERMISSION IN WRITING FROM THE PUBLISHER. PRINTED IN THE UNITED STATES OF AMERICA BY LULU INCORPORATION, MORRISVILLE, NC, USA COVER PRINTED ON LAMINATED 100# ULTRA GLOSS COVER STOCK, DIGITAL COLOR SILK - C2S, 90 BRIGHT BOOK CONTENT PRINTED ON 24/60# CREAM TEXT, 90 GSM PAPER, USING 12 PT. GARAMOND FONT Page vi Dedication What are we in this cosmos? This ineffable question has haunted us since Buddha sat under the Bodhi Tree. I would like to gracefully thank the author, Chán Master Wúmén, for his grace and kindness by leaving us these wonderful teachings. I would also like to thank Chán Master Dàhuì for his ineptness in destroying all copies of this book; thankfully, Master Dàhuì missed a few so that now we can explore the teachings of his teacher. -

The Analects of Confucius
The analecTs of confucius An Online Teaching Translation 2015 (Version 2.21) R. Eno © 2003, 2012, 2015 Robert Eno This online translation is made freely available for use in not for profit educational settings and for personal use. For other purposes, apart from fair use, copyright is not waived. Open access to this translation is provided, without charge, at http://hdl.handle.net/2022/23420 Also available as open access translations of the Four Books Mencius: An Online Teaching Translation http://hdl.handle.net/2022/23421 Mencius: Translation, Notes, and Commentary http://hdl.handle.net/2022/23423 The Great Learning and The Doctrine of the Mean: An Online Teaching Translation http://hdl.handle.net/2022/23422 The Great Learning and The Doctrine of the Mean: Translation, Notes, and Commentary http://hdl.handle.net/2022/23424 CONTENTS INTRODUCTION i MAPS x BOOK I 1 BOOK II 5 BOOK III 9 BOOK IV 14 BOOK V 18 BOOK VI 24 BOOK VII 30 BOOK VIII 36 BOOK IX 40 BOOK X 46 BOOK XI 52 BOOK XII 59 BOOK XIII 66 BOOK XIV 73 BOOK XV 82 BOOK XVI 89 BOOK XVII 94 BOOK XVIII 100 BOOK XIX 104 BOOK XX 109 Appendix 1: Major Disciples 112 Appendix 2: Glossary 116 Appendix 3: Analysis of Book VIII 122 Appendix 4: Manuscript Evidence 131 About the title page The title page illustration reproduces a leaf from a medieval hand copy of the Analects, dated 890 CE, recovered from an archaeological dig at Dunhuang, in the Western desert regions of China. The manuscript has been determined to be a school boy’s hand copy, complete with errors, and it reproduces not only the text (which appears in large characters), but also an early commentary (small, double-column characters). -

Download File
On the Periphery of a Great “Empire”: Secondary Formation of States and Their Material Basis in the Shandong Peninsula during the Late Bronze Age, ca. 1000-500 B.C.E Minna Wu Submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the Graduate School of Arts and Sciences COLUMIBIA UNIVERSITY 2013 @2013 Minna Wu All rights reserved ABSTRACT On the Periphery of a Great “Empire”: Secondary Formation of States and Their Material Basis in the Shandong Peninsula during the Late Bronze-Age, ca. 1000-500 B.C.E. Minna Wu The Shandong region has been of considerable interest to the study of ancient China due to its location in the eastern periphery of the central culture. For the Western Zhou state, Shandong was the “Far East” and it was a vast region of diverse landscape and complex cultural traditions during the Late Bronze-Age (1000-500 BCE). In this research, the developmental trajectories of three different types of secondary states are examined. The first type is the regional states established by the Zhou court; the second type is the indigenous Non-Zhou states with Dong Yi origins; the third type is the states that may have been formerly Shang polities and accepted Zhou rule after the Zhou conquest of Shang. On the one hand, this dissertation examines the dynamic social and cultural process in the eastern periphery in relation to the expansion and colonization of the Western Zhou state; on the other hand, it emphasizes the agency of the periphery during the formation of secondary states by examining how the polities in the periphery responded to the advances of the Western Zhou state and how local traditions impacted the composition of the local material assemblage which lay the foundation for the future prosperity of the regional culture. -
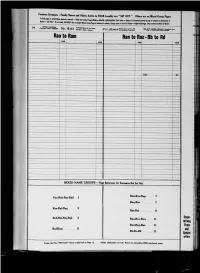
Grantor Index to Land Records
^^^ Common Surname. - Family Name, and Other, Active in YOUR Locality are "SET OUT." Other, are on Mixed Gronp Page,. Nale'is^SET OUT "tm» iKi">i ! ^"^ ~"^l00k Under Pr0P8r PRIME 0r MASTER SUB-0IVISI0N' (firs, letter or le,,ers of Sumame, Prin,ed • ,0P of tolomn5 "• detemiine if not listed, SECONDLY rsfer to proper Mixed Group Page at bottom of column. Groups start on Front of Sheets—Right Hand Page. They continue on Back of Sheets l 54 Copyii9hl 1951-AA199 757 No. 12-63 IStHT^iT*'** *** «• u . ^t _-„ OM.^ I„d«.. Sine. 1888 TO COW DTOD COMrAHT Cl—k-. OW. I* WW 63 Lbf-UnlU-tartly «T.OF„c.6^l^«<5^frAn|d.ndWn.Tr.d.M«k flKWWCSHfiC'jSS^ Rai a toiRam Ran to Raz - Rb to Rd PAGI FACE MM PAGE I , . Rav 15 ..— _ • — 1 - - 1 ••"• , • 1 MIXED NAME GROUPS—Page Reference for Surname, Not Set Out. Ran-Rao- Rap 7 Raa-Rab-Rac-Rad 1 Raq-Rar 7 Rae-Raf-Rag 3 : Ras-Rat 9 i I Corpo- Rah-Rai-Raj-Rak 3 Rau-Rav-Jlaw 11 rations, Rax-Ray-1 laz 11 Firms Ral-Ram 5 and Rb-Rc-Rd 11 Special OVER Assign the First " 5ETOL IT" Name of this Unit to Page 15 Awifn additional (set out) Names to succeeding ODD numbered pages. Corporation,, Firm., Partnership., Etc., Active in YOUR Locality are "SET OUT." Other, are on Mixed Group Pages. To find page on which Name desired is en.ered-FIRST look under Proper PRIME or MASTER SUB-DIVISION, (first letter of First Principal Word, ignore prefix "Th.") printed at top of columns to determine if Name is "SET OUT." If not listed, SECONDLY refer to proper Mixed Group Page at bottom of column. -

Nabu 2005-25 Ran Zadok Tikva Zadok
Nabu 2005-25 Ran Zadok Tikva Zadok 25) On the Esaggil-mansum Clan – All the BM tablets below are published or quoted with kind permission of the Trustees of the British Museum. Tikva Zadok is responsible only for the copy. The months in Roman fi gures are the Babylonian ones. BM 29379 - Esaggil-mansum, 8.XII.4 Camb. = 526/5 BC (1) MU 4 KAM mkam-bu-zi-iá LUGAL TIN.TIRki (2) LUGAL KUR.KUR ƒqu-da-šú DUMU.MUNUS-su (3) <šá> md+AG-mu-tir-ri-gi-mil A mSUMna-dpap-sukkal (4) i-na hu-ud ŠÀbi-šú ŠE.NUMUN-šú šá i-na (5) é-sag-gil-man-sum ma-la ba* (over erasure)-šu-ú (6) šá md+AG-MU-SI.SÁ DUMU-šú šá md+AG-na-ṣir (7) A msag-gil-<man>-sum DAM-su* ku-ú nu- dun-né-šú (8) ik-nu-uk-<<nu>>ku pa-ni-šú ú-šad-gi-li (9) ta-ak-nu-uk-ma pa-ni mdDUMU. É-ŠEŠmeš-MU (10) DUMU-šú šá md+AG-MU-SI.SÁ A msag-gil-man-sum (11) DUMU<<meš>>-šú ku-ú su-da-di-šú (12) pa-la-hi-šú ù ma-ṣar?!-ti-šú (13) tu-šad-gil u4-mu ma-la ƒqu-da-šú md meš (14) bal-ṭa-tu4 BURU14 A.ŠÀ i-na pa-ni-šú (15) ar-kát-tu-ú pa-ni DUMU.É-ŠEŠ -MU (16) DUMU-šú id-dag-gal (r. 17) i-na ka-nak na’DUB MUmeš (18) IGI mÌR-dgu-la DUMU-šú šá mMU- a (19) A mla-kup-pu-ru md+EN-ib-ni DUMU-šú šá (20) md+AG-MU-SUMna A mdDÙ-ib-ni (21) md+AG-ra-’-<im>-UNmeš-šú DUMU-šú šá mba-la-ṭu (22) A mDÙmeš-<šá>-DINGIR-iá md+AG-KAR- ZImeš DUMU-šú šá (23) mšu*-la-a A m.lúGAL DÙ md+AG-ŠEŠmeš-MU (24) DUMU-šú šá mDÙ-a A m.lú m d+ lú md+ na m NAGAR ÌR- EN (25) DUB.SAR DUMU-šú šá AG-MU4-SUM (26) A DÙ-A+A é-sag- iti m ki gil-man-sum ŠE (27) U4 8 KAM <<MU>> MU 4 KAM kam-bu-zi-iá (28) LUGAL TIN.TIR LUGAL KUR.KUR d(text PA)UTU dPA dAMAR.UTU (29) -

Representing Talented Women in Eighteenth-Century Chinese Painting: Thirteen Female Disciples Seeking Instruction at the Lake Pavilion
REPRESENTING TALENTED WOMEN IN EIGHTEENTH-CENTURY CHINESE PAINTING: THIRTEEN FEMALE DISCIPLES SEEKING INSTRUCTION AT THE LAKE PAVILION By Copyright 2016 Janet C. Chen Submitted to the graduate degree program in Art History and the Graduate Faculty of the University of Kansas in partial fulfillment of the requirements for the degree of Doctor of Philosophy. ________________________________ Chairperson Marsha Haufler ________________________________ Amy McNair ________________________________ Sherry Fowler ________________________________ Jungsil Jenny Lee ________________________________ Keith McMahon Date Defended: May 13, 2016 The Dissertation Committee for Janet C. Chen certifies that this is the approved version of the following dissertation: REPRESENTING TALENTED WOMEN IN EIGHTEENTH-CENTURY CHINESE PAINTING: THIRTEEN FEMALE DISCIPLES SEEKING INSTRUCTION AT THE LAKE PAVILION ________________________________ Chairperson Marsha Haufler Date approved: May 13, 2016 ii Abstract As the first comprehensive art-historical study of the Qing poet Yuan Mei (1716–97) and the female intellectuals in his circle, this dissertation examines the depictions of these women in an eighteenth-century handscroll, Thirteen Female Disciples Seeking Instructions at the Lake Pavilion, related paintings, and the accompanying inscriptions. Created when an increasing number of women turned to the scholarly arts, in particular painting and poetry, these paintings documented the more receptive attitude of literati toward talented women and their support in the social and artistic lives of female intellectuals. These pictures show the women cultivating themselves through literati activities and poetic meditation in nature or gardens, common tropes in portraits of male scholars. The predominantly male patrons, painters, and colophon authors all took part in the formation of the women’s public identities as poets and artists; the first two determined the visual representations, and the third, through writings, confirmed and elaborated on the designated identities. -

Chinese Radicals (Meaning Parts); Section 2: GCSE Vocabulary & Key Structures; Section 3: Key Grammar Points; Section 4: Chinese Culture;
Pre-U Mandarin 中文 Preparation materials This booklet contains suggestions how you can prepare yourself to make a confident start in AS Chinese after your GCSEs. In this booklet you will find a Chinese vocabulary and grammar revision, which will lead to an exam at the beginning of the course in September. In order to have a great start please prepare for the test in advance and aim for high marks. Please learn or revise the following sections. The exam will be written in a similar way to each exercise. Content: Section 1: Chinese radicals (meaning parts); Section 2: GCSE Vocabulary & key structures; Section 3: Key grammar points; Section 4: Chinese culture; Section 1: Chinese radicals (meaning parts) Chinese radicals, or meaning parts, are very important for the usage of dictionary, and also can greatly facilitate the memorisation of Chinese characters. Please learn the following key Chinese radicals. You need to be able to write them from memory, and identify them in individual characters. "people" related to "street" related to "mouth" "speak" related to "female" related to "person" "cold" "water" related to "sun" "body" related to "fence" related to "hand" "hand" related to "silk" related to "silk" related to "trees" related to "feeling" related to "feeling" related to "knife" related to "knife" related to "knife" related to "fire" related to "fire" related to "road" related to "border" related to "eye" related to " feet" related to "food" related to "metal" related to "aninmals" related to "roof" related to "cave" related to "grass" related to "bamboo" indicate actions related to "strength" related to "pray" related to "clothes" related to "soil" related to "stone" related to "hill" related to "room" related to "illness" related to "room" related to "door" related to "jade" related to "money" related to "field" Exercise: Part A Write the following radicals from your memory: People_____ jade _____ animal _______ silk _____ trees ____ soil ____ Part B write down the radicals of the following characters on the lines. -

The Sinitic Nominal Phrase Structure: a Minimalist Perspective
University of Cambridge Faculty of Modern and Medieval Languages The Sinitic Nominal Phrase Structure: A Minimalist Perspective Yi-An Lin St. Catharine’s College This dissertation is submitted for the degree of Doctor of Philosophy 2009 i DECLARATION This dissertation is a result of my own work and includes nothing which is the outcome of work done in collaboration except where specifically indicated in the text. It does not exceed the word limit of 80,000 words. The research reported in this dissertation was partially funded by the Studying Abroad Scholarship from the Ministry of Education, Republic of China (Taiwan). ii The Sinitic Nominal Phrase Structure: A Minimalist Perspective Yi-An Lin SUMMARY This dissertation is a comparative study of the morphosyntax of the constituents referred to as noun phrases in traditional grammar. In line with Abney’s (1987) Determiner Phrase (DP) Hypothesis, this study investigates the syntactic structures of Sinitic nominal phrases by means of a thorough study of lexical elements, such as numerals, classifiers, possessives, adjectives, and nouns, and functional elements, such as plural/collective markers, force particles, and modification markers. It is argued that the syntactic structure of the nominal phrase is universal regardless of the presence of lexical items which realise the heads of the functional projections. This study further proposes a unified account of the articulated structure of nominal phrases, as a full-fledged DP, to explain the syntactic phenomena in both classifier and non-classifier languages. More specifically, a Probe-Goal feature-valuing model is proposed to account for parametric variation among Sinitic and other languages within the framework of Chomsky’s (2000, 2001, 2004) Phase-based Minimalist Programme. -

Inhabiting Literary Beijing on the Eve of the Manchu Conquest
THE UNIVERSITY OF CHICAGO CITY ON EDGE: INHABITING LITERARY BEIJING ON THE EVE OF THE MANCHU CONQUEST A DISSERTATION SUBMITTED TO THE FACULTY OF THE DIVISION OF THE HUMANITIES IN CANDIDACY FOR THE DEGREE OF DOCTOR OF PHILOSOPHY DEPARTMENT OF EAST ASIAN LANGUAGES AND CIVILIZATIONS BY NAIXI FENG CHICAGO, ILLINOIS DECEMBER 2019 TABLE OF CONTENTS LIST OF FIGURES ....................................................................................................................... iv ACKNOWLEDGEMENTS .............................................................................................................v ABSTRACT ................................................................................................................................. viii 1 A SKETCH OF THE NORTHERN CAPITAL...................................................................1 1.1 The Book ........................................................................................................................4 1.2 The Methodology .........................................................................................................25 1.3 The Structure ................................................................................................................36 2 THE HAUNTED FRONTIER: COMMEMORATING DEATH IN THE ACCOUNTS OF THE STRANGE .................39 2.1 The Nunnery in Honor of the ImperiaL Sister ..............................................................41 2.2 Ant Mounds, a Speaking SkulL, and the Southern ImperiaL Park ................................50 -

Rethinking Chinese Kinship in the Han and the Six Dynasties: a Preliminary Observation
part 1 volume xxiii • academia sinica • taiwan • 2010 INSTITUTE OF HISTORY AND PHILOLOGY third series asia major • third series • volume xxiii • part 1 • 2010 rethinking chinese kinship hou xudong 侯旭東 translated and edited by howard l. goodman Rethinking Chinese Kinship in the Han and the Six Dynasties: A Preliminary Observation n the eyes of most sinologists and Chinese scholars generally, even I most everyday Chinese, the dominant social organization during imperial China was patrilineal descent groups (often called PDG; and in Chinese usually “zongzu 宗族”),1 whatever the regional differences between south and north China. Particularly after the systematization of Maurice Freedman in the 1950s and 1960s, this view, as a stereo- type concerning China, has greatly affected the West’s understanding of the Chinese past. Meanwhile, most Chinese also wear the same PDG- focused glasses, even if the background from which they arrive at this view differs from the West’s. Recently like Patricia B. Ebrey, P. Steven Sangren, and James L. Watson have tried to challenge the prevailing idea from diverse perspectives.2 Some have proven that PDG proper did not appear until the Song era (in other words, about the eleventh century). Although they have confirmed that PDG was a somewhat later institution, the actual underlying view remains the same as before. Ebrey and Watson, for example, indicate: “Many basic kinship prin- ciples and practices continued with only minor changes from the Han through the Ch’ing dynasties.”3 In other words, they assume a certain continuity of paternally linked descent before and after the Song, and insist that the Chinese possessed such a tradition at least from the Han 1 This article will use both “PDG” and “zongzu” rather than try to formalize one term or one English translation.