Mechanisms of Ccr5 Agonist/Antagonist Inhibition of Hiv-1
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
HIV Tropism Testing for Maraviroc Response
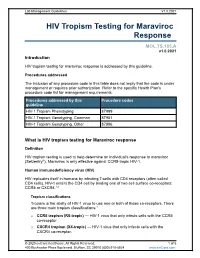
Lab Management Guidelines V1.0.2021 HIV Tropism Testing for Maraviroc Response MOL.TS.185.A v1.0.2021 Introduction HIV tropism testing for maraviroc response is addressed by this guideline. Procedures addressed The inclusion of any procedure code in this table does not imply that the code is under management or requires prior authorization. Refer to the specific Health Plan's procedure code list for management requirements. Procedures addressed by this Procedure codes guideline HIV-1 Tropism Phenotyping 87999 HIV-1 Tropism Genotyping, Common 87901 HIV-1 Tropism Genotyping, Other 87906 What is HIV tropism testing for Maraviroc response Definition HIV tropism testing is used to help determine an individual's response to maraviroc (Selzentry®). Maraviroc is only effective against CCR5-tropic HIV-1. Human immunodeficiency virus (HIV) HIV replicates itself in humans by infecting T-cells with CD4 receptors (often called CD4 cells). HIV-1 enters the CD4 cell by binding one of two cell surface co-receptors: CCR5 or CXCR4.1,2 Tropism classifications Tropism is the ability of HIV-1 virus to use one or both of these co-receptors. There are three main tropism classifications:3 o CCR5 tropism (R5-tropic) — HIV-1 virus that only infects cells with the CCR5 co-receptor. o CXCR4 tropism (X4-tropic) — HIV-1 virus that only infects cells with the CXCR4 co-receptor. © 2020 eviCore healthcare. All Rights Reserved. 1 of 5 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Lab Management Guidelines V1.0.2021 o Dual or mixed tropism (D/M-tropic) — HIV-1 virus populations that can use either co-receptor to infect cells. -

Enhanced Monocyte Migration to CXCR3 and CCR5 Chemokines in COPD
ERJ Express. Published on March 10, 2016 as doi: 10.1183/13993003.01642-2015 ORIGINAL ARTICLE IN PRESS | CORRECTED PROOF Enhanced monocyte migration to CXCR3 and CCR5 chemokines in COPD Claudia Costa1, Suzanne L. Traves1, Susan J. Tudhope1, Peter S. Fenwick1, Kylie B.R. Belchamber1, Richard E.K. Russell2, Peter J. Barnes1 and Louise E. Donnelly1 Affiliations: 1Airway Disease, National Heart and Lung Institute, Imperial College London, London, UK. 2Chest Clinic, King Edward King VII Hospital, Windsor, UK. Correspondence: Louise E. Donnelly, Airway Disease, National Heart and Lung Institute, Dovehouse Street, London, SW3 6LY, UK. E-mail: [email protected] ABSTRACT Chronic obstructive pulmonary disease (COPD) patients exhibit chronic inflammation, both in the lung parenchyma and the airways, which is characterised by an increased infiltration of macrophages and T-lymphocytes, particularly CD8+ cells. Both cell types can express chemokine (C-X-C motif) receptor (CXCR)3 and C-C chemokine receptor 5 and the relevant chemokines for these receptors are elevated in COPD. The aim of this study was to compare chemotactic responses of lymphocytes and monocytes of nonsmokers, smokers and COPD patients towards CXCR3 ligands and chemokine (C-C motif) ligand (CCL)5. Migration of peripheral blood mononuclear cells, monocytes and lymphocytes from nonsmokers, smokers and COPD patients toward CXCR3 chemokines and CCL5 was analysed using chemotaxis assays. There was increased migration of peripheral blood mononuclear cells from COPD patients towards all chemokines studied when compared with nonsmokers and smokers. Both lymphocytes and monocytes contributed to this enhanced response, which was not explained by increased receptor expression. -

Revised 4/1/2021 GEORGIA MEDICAID FEE-FOR-SERVICE HIV
GEORGIA MEDICAID FEE-FOR-SERVICE HIV-AIDS PA SUMMARY Preferred (may not be all inclusive) Non-Preferred Abacavir generic Abacavir/lamivudine/zidovudine generic Abacavir/lamivudine generic Aptivus (tipranavir) Complera (emtricitabine/rilpivirine/tenofovir disoproxil Atazanavir capsules generic fumarate) Atripla (efavirenz/emtricitabine/tenofovir disoproxil Crixivan (indinavir) fumarate) Biktarvy (bictegravir/emtricitabine/tenofovir Delstrigo (doravirine/lamivudine/tenofovir disoproxil alafenamide) fumarate) Cimduo (lamivudine/tenofovir disoproxil fumarate) Fuzeon (enfuvirtide) Descovy (emtricitabine/tenofovir alafenamide) Intelence (etravirine) Dovato Invirase (saquinavir) Edurant (rilpivirine)* Lexiva (fosamprenavir) Efavirenz tablets generic Nevirapine extended-release generic Emtriva (emtricitabine) Norvir Powder (ritonavir) Epivir solution (lamivudine) Pifeltro (doravirine) Evotaz (atazanavir/cobicistat)* Reyataz Powder (atazanavir) Genvoya (elvitegravir/cobicistat/emtricitabine/ Ritonavir tablets generic tenofovir alafenamide) Isentress and Isentress HD (raltegravir)* Rukobia (fostemsavir) Juluca (dolutegravir/rilpivirine) Selzentry (maraviroc) Kaletra (lopinavir/ritonavir) Stavudine generic^ Stribild (elvitegravir/cobicistat/emtricitabine/ tenofovir Lamivudine generic disoproxil fumarate) Symfi (efavirenz 600 mg/lamivudine/tenofovir Lamivudine/zidovudine generic disoproxil fumarate) Symfi Lo (efavirenz 400 mg/lamivudine/tenofovir Nevirapine immediate-release tablets generic disoproxil fumarate) Norvir (ritonavir) Temixys (lamivudine/tenofovir -

Human Th17 Cells Share Major Trafficking Receptors with Both Polarized Effector T Cells and FOXP3+ Regulatory T Cells
Human Th17 Cells Share Major Trafficking Receptors with Both Polarized Effector T Cells and FOXP3+ Regulatory T Cells This information is current as Hyung W. Lim, Jeeho Lee, Peter Hillsamer and Chang H. of September 28, 2021. Kim J Immunol 2008; 180:122-129; ; doi: 10.4049/jimmunol.180.1.122 http://www.jimmunol.org/content/180/1/122 Downloaded from References This article cites 44 articles, 15 of which you can access for free at: http://www.jimmunol.org/content/180/1/122.full#ref-list-1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on September 28, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2008 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology Human Th17 Cells Share Major Trafficking Receptors with Both Polarized Effector T Cells and FOXP3؉ Regulatory T Cells1 Hyung W. Lim,* Jeeho Lee,* Peter Hillsamer,† and Chang H. Kim2* It is a question of interest whether Th17 cells express trafficking receptors unique to this Th cell lineage and migrate specifically to certain tissue sites. -

Characterization of Resistance to a Potent D-Peptide HIV Entry Inhibitor
Smith et al. Retrovirology (2019) 16:28 https://doi.org/10.1186/s12977-019-0489-7 Retrovirology RESEARCH Open Access Characterization of resistance to a potent D-peptide HIV entry inhibitor Amanda R. Smith1†, Matthew T. Weinstock1†, Amanda E. Siglin2, Frank G. Whitby1, J. Nicholas Francis1, Christopher P. Hill1, Debra M. Eckert1, Michael J. Root2 and Michael S. Kay1* Abstract Background: PIE12-trimer is a highly potent D-peptide HIV-1 entry inhibitor that broadly targets group M isolates. It specifcally binds the three identical conserved hydrophobic pockets at the base of the gp41 N-trimer with sub- femtomolar afnity. This extremely high afnity for the transiently exposed gp41 trimer provides a reserve of binding energy (resistance capacitor) to prevent the viral resistance pathway of stepwise accumulation of modest afnity- disrupting mutations. Such modest mutations would not afect PIE12-trimer potency and therefore not confer a selective advantage. Viral passaging in the presence of escalating PIE12-trimer concentrations ultimately selected for PIE12-trimer resistant populations, but required an extremely extended timeframe (> 1 year) in comparison to other entry inhibitors. Eventually, HIV developed resistance to PIE12-trimer by mutating Q577 in the gp41 pocket. Results: Using deep sequence analysis, we identifed three mutations at Q577 (R, N and K) in our two PIE12-trimer resistant pools. Each point mutant is capable of conferring the majority of PIE12-trimer resistance seen in the poly- clonal pools. Surface plasmon resonance studies demonstrated substantial afnity loss between PIE12-trimer and the Q577R-mutated gp41 pocket. A high-resolution X-ray crystal structure of PIE12 bound to the Q577R pocket revealed the loss of two hydrogen bonds, the repositioning of neighboring residues, and a small decrease in buried surface area. -

KALETRA (Lopinavir/Ritonavir)
HIGHLIGHTS OF PRESCRIBING INFORMATION CONTRAINDICATIONS These highlights do not include all the information needed to use • Hypersensitivity to KALETRA (e.g., toxic epidermal necrolysis, Stevens- KALETRA safely and effectively. See full prescribing information for Johnson syndrome, erythema multiforme, urticaria, angioedema) or any of KALETRA. its ingredients, including ritonavir. (4) • Co-administration with drugs highly dependent on CYP3A for clearance KALETRA (lopinavir and ritonavir) tablet, for oral use and for which elevated plasma levels may result in serious and/or life- KALETRA (lopinavir and ritonavir) oral solution threatening events. (4) Initial U.S. Approval: 2000 • Co-administration with potent CYP3A inducers where significantly reduced lopinavir plasma concentrations may be associated with the potential for RECENT MAJOR CHANGES loss of virologic response and possible resistance and cross resistance. (4) Contraindications (4) 12/2019 WARNINGS AND PRECAUTIONS The following have been observed in patients receiving KALETRA: INDICATIONS AND USAGE • The concomitant use of KALETRA and certain other drugs may result in KALETRA is an HIV-1 protease inhibitor indicated in combination with other known or potentially significant drug interactions. Consult the full antiretroviral agents for the treatment of HIV-1 infection in adults and prescribing information prior to and during treatment for potential drug pediatric patients (14 days and older). (1) interactions. (5.1, 7.3) • Toxicity in preterm neonates: KALETRA oral solution should not be used DOSAGE AND ADMINISTRATION in preterm neonates in the immediate postnatal period because of possible Tablets: May be taken with or without food, swallowed whole and not toxicities. A safe and effective dose of KALETRA oral solution in this chewed, broken, or crushed. -

Truvada (Emtricitabine / Tenofovir Disoproxil)
Pre-exposure Prophylaxis (2.3) HIGHLIGHTS OF PRESCRIBING INFORMATION These highlights do not include all the information needed to use Recommended dose in HIV-1 uninfected adults: One tablet TRUVADA safely and effectively. See full prescribing information (containing 200 mg/300 mg of emtricitabine and tenofovir for TRUVADA. disoproxil fumarate) once daily taken orally with or without food. (2.3) TRUVADA® (emtricitabine/tenofovir disoproxil fumarate) tablets, for oral use Recommended dose in renally impaired HIV-uninfected Initial U.S. Approval: 2004 individuals: Do not use TRUVADA in HIV-uninfected individuals if CrCl is below 60 mL/min. If a decrease in CrCl is observed in WARNING: LACTIC ACIDOSIS/SEVERE HEPATOMEGALY WITH uninfected individuals while using TRUVADA for PrEP, evaluate STEATOSIS, POST-TREATMENT ACUTE EXACERBATION OF potential causes and re-assess potential risks and benefits of HEPATITIS B, and RISK OF DRUG RESISTANCE WITH USE OF continued use. (2.4) TRUVADA FOR PrEP IN UNDIAGNOSED HIV-1 INFECTION -----------------------DOSAGE FORMS AND STRENGTHS------------------- See full prescribing information for complete boxed warning. Tablets: 200 mg/300 mg, 167 mg/250 mg, 133 mg/200 mg, and 100 Lactic acidosis and severe hepatomegaly with steatosis, mg/150 mg of emtricitabine and tenofovir disoproxil fumarate . (3) including fatal cases, have been reported with the use of nucleoside analogs, including VIREAD, a component of TRUVADA. (5.1) --------------------------------CONTRAINDICATIONS----------------------------- TRUVADA is not approved for the treatment of chronic Do not use TRUVADA for pre-exposure prophylaxis in individuals with hepatitis B virus (HBV) infection. Severe acute unknown or positive HIV-1 status. TRUVADA should be used in exacerbations of hepatitis B have been reported in patients HIV-infected patients only in combination with other antiretroviral coinfected with HIV-1 and HBV who have discontinued agents. -

Download Article PDF/Slides
New Antiretrovirals in Development: Reprinted from The PRN Notebook,™ june 2002. Dr. James F. Braun, Editor-in-Chief. Tim Horn, Executive Editor. Published in New York City by the Physicians’ Research Network, Inc.,® John Graham Brown, Executive Director. For further information and other articles The View in 2002 available online, visit http://www.PRN.org All rights reserved. © june 2002. Roy “Trip” Gulick, md, mph Associate Professor of Medicine, Weill Medical College of Cornell University Director, Cornell Clinical Trials Unit, New York, New York Summary by Tim Horn Edited by Scott Hammer, md espite the fact that 16 antiretro- tiviral activity of emtricitabine was estab- Preliminary results from two random- virals are approved for use in the lished, with total daily doses of 200 mg or ized studies—FTC-302 and FTC-303—were United States, there is an indis- more producing the greatest median viral reported by Dr. Charles van der Horst and putable need for new anti-hiv com- load suppression: 1.72-1.92 log. Based on his colleagues at the 8th croi, held in Feb- pounds that have potent and these data, a once-daily dose of 200 mg ruary 2001 in Chicago (van der Horst, durable efficacy profiles, unique re- was selected for further long-term clinical 2001). FTC-302 was a blinded comparison sistance patterns, patient-friendly dosing study. “This is what we’re looking forward of emtricitabine and lamivudine, both in schedules, and minimal toxicities. To pro- to with emtricitabine,” commented Dr. combination with stavudine (Zerit) and vide prn with a glimpse of drugs current- Gulick. -

Plasma HIV-1 Tropism and the Risk of Short-Term Clinical Progression to AIDS Or Death
Plasma HIV-1 Tropism and the Risk of Short-Term Clinical Progression to AIDS or Death Casadellà, Maria; Cozzi-Lepri, Alessandro; Phillips, Andrew; Noguera-Julian, Marc; Bickel, Markus; Sedlacek, Dalibor; Zilmer, Kai; Clotet, Bonaventura; Lundgren, Jens D; Paredes, Roger; EuroSIDA in EuroCoord Published in: PloS one DOI: 10.1371/journal.pone.0166613 Publication date: 2017 Document version Publisher's PDF, also known as Version of record Document license: CC BY Citation for published version (APA): Casadellà, M., Cozzi-Lepri, A., Phillips, A., Noguera-Julian, M., Bickel, M., Sedlacek, D., Zilmer, K., Clotet, B., Lundgren, J. D., Paredes, R., & EuroSIDA in EuroCoord (2017). Plasma HIV-1 Tropism and the Risk of Short- Term Clinical Progression to AIDS or Death. PloS one, 12(1), [e0166613]. https://doi.org/10.1371/journal.pone.0166613 Download date: 28. Sep. 2021 RESEARCH ARTICLE Plasma HIV-1 Tropism and the Risk of Short- Term Clinical Progression to AIDS or Death Maria Casadellà1,2*, Alessandro Cozzi-Lepri3, Andrew Phillips3, Marc Noguera-Julian1,2,4, Markus Bickel5, Dalibor Sedlacek6, Kai Zilmer7, Bonaventura Clotet1,2,4,8, Jens D. Lundgren9, Roger Paredes1,2,4,8, EuroSIDA in EuroCOORD¶ 1 IrsiCaixa AIDS Research Institute, Badalona, Catalonia, Spain, 2 Universitat Autònoma de Barcelona, Catalonia, Spain, 3 Royal Free Hospital, London, United Kingdom, 4 Universitat de Vic-Universitat Central de Catalunya, Vic, Catalonia, Spain, 5 Goethe University, Frankfurt/Main, Germany, 6 Charles University a1111111111 Hospital, Plzen, Česka Republika, 7 West-Tallinn Central Hospital, Tallinn, Estonia, 8 HIV Unit, Hospital a1111111111 Universitari Germans Trias i Pujol, Badalona, Catalonia, Spain, 9 CHIP, Department of Infectious Diseases, Rigshospitalet, University of Copenhagen, Copenhagen, Denmark a1111111111 a1111111111 ¶ Membership of this author group is listed in the Acknowledgments. -

Review CCR5 Antagonists: Host-Targeted Antivirals for the Treatment of HIV Infection
Antiviral Chemistry & Chemotherapy 16:339–354 Review CCR5 antagonists: host-targeted antivirals for the treatment of HIV infection Mike Westby* and Elna van der Ryst Pfizer Global R&D, Kent, UK *Corresponding author: Tel: +44 1304 649876; Fax: +44 1304 651819; E-mail: [email protected] The human chemokine receptors, CCR5 and suggest that these compounds have a long plasma CXCR4, are potential host targets for exogenous, half-life and/or prolonged CCR5 occupancy, which small-molecule antagonists for the inhibition of may explain the delay in viral rebound observed HIV-1 infection. HIV-1 strains can be categorised by following compound withdrawal in short-term co-receptor tropism – their ability to utilise CCR5 monotherapy studies. A switch from CCR5 to (CCR5-tropic), CXCR4 (CXCR4-tropic) or both (dual- CXCR4 tropism occurs spontaneously in approxi- tropic) as a co-receptor for entry into susceptible mately 50% of HIV-infected patients and has been cells. CCR5 may be the more suitable co-receptor associated with, but is not required for, disease target for small-molecule antagonists because a progression. The possibility of a co-receptor natural deletion in the CCR5 gene preventing its tropism switch occurring under selection pressure expression on the cell surface is not associated by CCR5 antagonists is discussed. The completion with any obvious phenotype, but can confer of ongoing Phase IIb/III studies of maraviroc, resistance to infection by CCR5-tropic strains – the aplaviroc and vicriviroc will provide further insight most frequently sexually-transmitted strains. into co-receptor tropism, HIV pathogenesis and The current leading CCR5 antagonists in clinical the suitability of CCR5 antagonists as a potent development include maraviroc (UK-427,857, new class of antivirals for the treatment of HIV Pfizer), aplaviroc (873140, GlaxoSmithKline) and infection. -

Vitekta Pi.Pdf
HIGHLIGHTS OF PRESCRIBING INFORMATION -----------------------DOSAGE FORMS AND STRENGTHS-------------------- These highlights do not include all the information needed to use Tablets: 85 mg and 150 mg (3) VITEKTA safely and effectively. See full prescribing information for VITEKTA. --------------------------------CONTRAINDICATIONS------------------------------ VITEKTA® (elvitegravir) tablets, for oral use There are no contraindications to VITEKTA. (4) Initial U.S. Approval: 2012 Due to the need to use VITEKTA with a protease inhibitor coadministered with ritonavir, consult prescribing information of -------------------------------INDICATIONS AND USAGE------------------------- coadministered protease inhibitor and ritonavir for their VITEKTA is a human immunodeficiency virus type 1 (HIV-1) integrase contraindications. (4) strand transfer inhibitor used in combination with an HIV protease inhibitor coadministered with ritonavir and with other antiretroviral -------------------------WARNINGS AND PRECAUTIONS---------------------- drug(s) indicated for the treatment of HIV-1 infection in antiretroviral Do not use with protease inhibitors coadministered with cobicistat. treatment-experienced adults. (1) (5.2) Do not use with other elvitegravir-containing drugs, including Limitations of Use: STRIBILD. (5.2) There are no comparative pharmacokinetic or clinical data Immune reconstitution syndrome: May necessitate further evaluation evaluating VITEKTA with cobicistat as single entities compared to and treatment. (5.3) STRIBILD®. (1) --------------------------------ADVERSE REACTIONS----------------------------- VITEKTA coadministered with protease inhibitors and cobicistat is The most common adverse drug reaction to VITEKTA (all grades) is not recommended. (1) diarrhea. (6.1) Coadministration of VITEKTA with dosage regimens or HIV-1 protease inhibitors other than those presented in Table 1 is not To report SUSPECTED ADVERSE REACTIONS, contact Gilead recommended. (1) Sciences, Inc. at 1-800-GILEAD-5 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. -

Correlating HIV Tropism with Immunological Response Under Cart
!"#$%&'%()*+,& -$%%,+"()./& 012& 3%$4)56& 7)(8& 1669.$+$/)*"+& :,54$.5,& ;.<,%& *':3& -$%,*,4($%&;5,&".<&=)5,"5,&>%$/%,55)$.& & !"#$$%& '()%*+,& -*(./012(& 3456.07899"$:%*;,& !<*=& '6.0>,& ?%*0& @"*=0%A1207B*01"5"C,& 3(D0.%& E%*$FG,& @$()F1& ?(*:0.%::0H,& ?(.I%$& '(::%=(FJ,& K5"L(1& M$0L2(0:+,& (.)& :5%& 3N011&BOP&Q"5"*:&3:I)F& !"#$%&'$()* +,)#$#-./* 0%1()23%42* 5,#3%6,&,4%* 7* 8%2%)91$(2:/* ;4,<%)9,2.* #=* 5(9%$/* >??@* 5(9%$/* AB,2:%)$(46C* DAB,99* EF+* G#H#)2* A2'6.* IAEGAJ* 0(2(* G%42%)/* ;4,<%)9,2.* E#91,2($* K('9(44%/* !?!L* K('9(44%/* AB,2:%)$(46* MF492,2'2%* #=* "%6,&($* +,)#$#-./* N(2,#4($* G%42%)* =#)* O%2)#<,)'9%9/* ;4,<%)9,2.* #=* PQ),&H/* R?LS* PQ),&H/* AB,2:%)$(46* >F492,2'2%*=#)*F4=%&2,#'9*0,9%(9%9/*;4,<%)9,2.*#=*5%)4%/*M?!?*5%)4/*AB,2:%)$(46* L;4,<%)9,2.*E#91,2($9*IE;TJ/*K(U#)(2#).*#=*+,)#$#-./*!D?L*T%4V<%/*AB,2:%)$(46W* X0%1()23%42*#=*0%)3(2#$#-./*O%-,#4($*E#91,2($*#=*5%$$,4:#4(/*XL?!*5%$$,4:#4(/*T%4%<(/*AB,2:%)$(46W* S0,<,9,#4* #=* F4=%&2,#'9* 0,9%(9%9* (46* E#91,2($* Y1,6%3,#$#-./* ;4,<%)9,2.* E#91,2($* 5(9%$/* >?M!* 5(9%$/* AB,2:%)$(46* * 8D1:*(4:&N"*)&4"I.:R&+ST& K%U:&N"*)&4"I.:R&>V>+& & Q"**%1W".)%.4%R&& X"%$$%YD()%*ZI.0D(1Y45,&VVC+&H;&;HJ&VS&T+& & ! "! '?5(%"*(& '(42=*"I.)R&[(:0%.:1&0.9%4:%)&N0:5&:5%&5IL(.&0LLI.")%9040%.4F&A0*I1&:FW%&+&\BOP7+]& L(F& %UW%*0%.4%& ".$F& 1ID"W:0L($& Q^C& 4%$$& *%4"A%*F& N50$%& :*%(:%)& N0:5& 4"LD0.(:0".& :5%*(WF& \48_K]Y& `0::$%& 01& 2."N.& (D"I:& N5%:5%*& A0*($& W*"W%*:0%1& 1I45& (1& 4%$$& :*"W01L& 4"I$)& W$(F& (& *"$%& 9"*& 1I45& 0.4"LW$%:%& 0LLI.%& *%1W".1%Y& K5I1& :501& 1:I)F& N(1&