Casodex® Tablets
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Prnu-BICALUTAMIDE
PRODUCT MONOGRAPH PrNU-BICALUTAMIDE Bicalutamide Tablets, 50 mg Non-Steroidal Antiandrogen NU-PHARM INC. DATE OF PREPARATION: 50 Mural Street, Units 1 & 2 October 16, 2009 Richmond Hill, Ontario L4B 1E4 Control#: 133521 Page 1 of 27 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION....................................................... 3 SUMMARY PRODUCT INFORMATION ............................................................................. 3 INDICATIONS AND CLINICAL USE ................................................................................... 3 CONTRAINDICATIONS ........................................................................................................ 3 WARNINGS AND PRECAUTIONS....................................................................................... 4 ADVERSE REACTIONS......................................................................................................... 5 DRUG INTERACTIONS ......................................................................................................... 9 DOSAGE AND ADMINISTRATION ................................................................................... 10 OVERDOSAGE...................................................................................................................... 10 ACTION AND CLINICAL PHARMACOLOGY.................................................................. 10 STORAGE AND STABILITY............................................................................................... 11 DOSAGE FORMS, COMPOSITION AND PACKAGING -
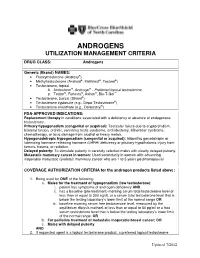
Androgens Utilization Management Criteria
ANDROGENS UTILIZATION MANAGEMENT CRITERIA DRUG CLASS: Androgens Generic (Brand) NAMES: • Fluoxymesterone (Androxy®) • Methyltestosterone (Android®, Methitest®, Testred®) • Testosterone, topical A. Androderm®, Androgel® - Preferred topical testosterone ® ® ® ™ B. Testim , Fortesta , Axiron , Bio-T-Gel • Testosterone, buccal (Striant®) • Testosterone cypionate (e.g., Depo-Testosterone®) • Testosterone enanthate (e.g., Delatestryl®) FDA-APPROVED INDICATIONS: Replacement therapy in conditions associated with a deficiency or absence of endogenous testosterone. Primary hypogonadism (congenital or acquired): Testicular failure due to cryptorchidism, bilateral torsion, orchitis, vanishing testis syndrome, orchidectomy, Klinefelter syndrome, chemotherapy, or toxic damage from alcohol or heavy metals. Hypogonadotropic hypogonadism (congenital or acquired): Idiopathic gonadotropin or luteinizing hormone-releasing hormone (LHRH) deficiency or pituitary-hypothalamic injury from tumors, trauma, or radiation. Delayed puberty: To stimulate puberty in carefully selected males with clearly delayed puberty. Metastatic mammary cancer in women: Used secondarily in women with advancing inoperable metastatic (skeletal) mammary cancer who are 1 to 5 years postmenopausal COVERAGE AUTHORIZATION CRITERIA for the androgen products listed above: 1. Being used for ONE of the following: a. Males for the treatment of hypogonadism (low testosterone): i. patient has symptoms of androgen deficiency AND ii. has a baseline (pre-treatment) morning serum total testosterone level of less than or equal to 300 ng/dL or a serum total testosterone level that is below the testing laboratory’s lower limit of the normal range OR iii. baseline morning serum free testosterone level, measured by the equilibrium dialysis method, of less than or equal to 50 pg/ml or a free serum testosterone level that is below the testing laboratory’s lower limit of the normal range, OR b. -

The Effects of Androgens and Antiandrogens on Hormone Responsive Human Breast Cancer in Long-Term Tissue Culture1
[CANCER RESEARCH 36, 4610-4618, December 1976] The Effects of Androgens and Antiandrogens on Hormone responsive Human Breast Cancer in Long-Term Tissue Culture1 Marc Lippman, Gail Bolan, and Karen Huff MedicineBranch,NationalCancerInstitute,Bethesda,Maryland20014 SUMMARY Information characterizing the interaction between an drogens and breast cancer would be desirable for several We have examined five human breast cancer call lines in reasons. First, androgens can affect the growth of breast conhinuous tissue culture for andmogan responsiveness. cancer in animals. Pharmacological administration of an One of these cell lines shows a 2- ho 4-fold stimulation of drogens to rats bearing dimathylbenzanthracene-induced thymidina incorporation into DNA, apparent as early as 10 mammary carcinomas is associated wihh objective humor hr following androgen addition to cells incubated in serum regression (h9, 22). Shionogi h15 cells, from a mouse mam free medium. This stimulation is accompanied by an ac many cancer in conhinuous hissue culture, have bean shown celemation in cell replication. Antiandrogens [cyproterona to be shimulatedby physiological concentrations of andro acetate (6-chloro-17a-acelata-1,2a-methylena-4,6-pregna gen (21), thus suggesting that some breast cancer might be diene-3,20-dione) and R2956 (17f3-hydroxy-2,2,1 7a-tnima androgen responsive in addition to being estrogen respon thoxyastra-4,9,1 1-Inane-i -one)] inhibit both protein and siva. DNA synthesis below control levels and block androgen Evidence also indicates that tumor growth in humans may mediahed stimulation. Prolonged incubahion (greahenhhan be significantly altered by androgens. About 20% of pahianhs 72 hn) in antiandrogen is lethal. -

Context-Specific Efficacy of Apalutamide Therapy in Preclinical
cancers Article Context-Specific Efficacy of Apalutamide Therapy in Preclinical Models of Pten-Deficient Prostate Cancer Marco A. De Velasco 1,2,* , Yurie Kura 1,2, Naomi Ando 1, Noriko Sako 1, Eri Banno 1, Kazutoshi Fujita 1, Masahiro Nozawa 1, Kazuhiro Yoshimura 1 , Kazuko Sakai 2, Kazuhiro Yoshikawa 3, Kazuto Nishio 2 and Hirotsugu Uemura 1,* 1 Department of Urology Kindai, University Faculty of Medicine, Osaka-Sayama 589-8511, Japan; [email protected] (Y.K.); [email protected] (N.A.); [email protected] (N.S.); [email protected] (E.B.); [email protected] (K.F.); [email protected] (M.N.); [email protected] (K.Y.) 2 Department of Genome Biology, Kindai University Faculty of Medicine, Osaka-Sayama 589-8511, Japan; [email protected] (K.S.); [email protected] (K.N.) 3 Research Creation Support Center, Aichi Medical University, Nagakute 480-1195, Japan; [email protected] * Correspondence: [email protected] (M.A.D.V.); [email protected] (H.U.) Simple Summary: Next-generation antiandrogens have transformed the therapeutic landscape for castration-resistant prostate cancer. Their utility in other indications, such as high-risk castration- sensitive cancers and as combination therapy, are being investigated. Our aim was to profile the in vivo antitumor activity of apalutamide in phenotypically distinct mouse models of Pten-deficient castration-naïve and castration-resistant prostate cancer, using both early- and late-stage disease Citation: De Velasco, M.A.; Kura, Y.; models, and to profile the molecular responses. -

CASODEX (Bicalutamide)
HIGHLIGHTS OF PRESCRIBING INFORMATION • Gynecomastia and breast pain have been reported during treatment with These highlights do not include all the information needed to use CASODEX 150 mg when used as a single agent. (5.3) CASODEX® safely and effectively. See full prescribing information for • CASODEX is used in combination with an LHRH agonist. LHRH CASODEX. agonists have been shown to cause a reduction in glucose tolerance in CASODEX® (bicalutamide) tablet, for oral use males. Consideration should be given to monitoring blood glucose in Initial U.S. Approval: 1995 patients receiving CASODEX in combination with LHRH agonists. (5.4) -------------------------- RECENT MAJOR CHANGES -------------------------- • Monitoring Prostate Specific Antigen (PSA) is recommended. Evaluate Warnings and Precautions (5.2) 10/2017 for clinical progression if PSA increases. (5.5) --------------------------- INDICATIONS AND USAGE -------------------------- ------------------------------ ADVERSE REACTIONS ----------------------------- • CASODEX 50 mg is an androgen receptor inhibitor indicated for use in Adverse reactions that occurred in more than 10% of patients receiving combination therapy with a luteinizing hormone-releasing hormone CASODEX plus an LHRH-A were: hot flashes, pain (including general, back, (LHRH) analog for the treatment of Stage D2 metastatic carcinoma of pelvic and abdominal), asthenia, constipation, infection, nausea, peripheral the prostate. (1) edema, dyspnea, diarrhea, hematuria, nocturia, and anemia. (6.1) • CASODEX 150 mg daily is not approved for use alone or with other treatments. (1) To report SUSPECTED ADVERSE REACTIONS, contact AstraZeneca Pharmaceuticals LP at 1-800-236-9933 or FDA at 1-800-FDA-1088 or ---------------------- DOSAGE AND ADMINISTRATION ---------------------- www.fda.gov/medwatch The recommended dose for CASODEX therapy in combination with an LHRH analog is one 50 mg tablet once daily (morning or evening). -

Combination Therapy of Antiandrogen and XIAP Inhibitor for Treating Advanced Prostate Cancer
Combination Therapy of Antiandrogen and XIAP Inhibitor for Treating Advanced Prostate Cancer Michael Danquah, Charles B. Duke, Renukadevi Patil, Duane D. Miller & Ram I. Mahato Pharmaceutical Research An Official Journal of the American Association of Pharmaceutical Scientists ISSN 0724-8741 Volume 29 Number 8 Pharm Res (2012) 29:2079-2091 DOI 10.1007/s11095-012-0737-1 1 23 Your article is protected by copyright and all rights are held exclusively by Springer Science+Business Media, LLC. This e-offprint is for personal use only and shall not be self- archived in electronic repositories. If you wish to self-archive your work, please use the accepted author’s version for posting to your own website or your institution’s repository. You may further deposit the accepted author’s version on a funder’s repository at a funder’s request, provided it is not made publicly available until 12 months after publication. 1 23 Author's personal copy Pharm Res (2012) 29:2079–2091 DOI 10.1007/s11095-012-0737-1 RESEARCH PAPER Combination Therapy of Antiandrogen and XIAP Inhibitor for Treating Advanced Prostate Cancer Michael Danquah & Charles B. Duke III & Renukadevi Patil & Duane D. Miller & Ram I. Mahato Received: 4 February 2012 /Accepted: 9 March 2012 /Published online: 27 March 2012 # Springer Science+Business Media, LLC 2012 ABSTRACT Results CBDIV17 was more potent than bicalutamide and Purpose Overexpression of the androgen receptor (AR) and inhibited proliferation of C4-2 and LNCaP cells, IC50 for CBDIV17 anti-apoptotic genes including X-linked inhibitor of apoptosis was ∼12 μMand∼21 μM in LNCaP and C4-2 cells, respectively, protein (XIAP) provide tumors with a proliferative advantage. -

COVID-19—The Potential Beneficial Therapeutic Effects of Spironolactone During SARS-Cov-2 Infection
pharmaceuticals Review COVID-19—The Potential Beneficial Therapeutic Effects of Spironolactone during SARS-CoV-2 Infection Katarzyna Kotfis 1,* , Kacper Lechowicz 1 , Sylwester Drozd˙ zal˙ 2 , Paulina Nied´zwiedzka-Rystwej 3 , Tomasz K. Wojdacz 4, Ewelina Grywalska 5 , Jowita Biernawska 6, Magda Wi´sniewska 7 and Miłosz Parczewski 8 1 Department of Anesthesiology, Intensive Therapy and Acute Intoxications, Pomeranian Medical University in Szczecin, 70-111 Szczecin, Poland; [email protected] 2 Department of Pharmacokinetics and Monitored Therapy, Pomeranian Medical University, 70-111 Szczecin, Poland; [email protected] 3 Institute of Biology, University of Szczecin, 71-412 Szczecin, Poland; [email protected] 4 Independent Clinical Epigenetics Laboratory, Pomeranian Medical University, 71-252 Szczecin, Poland; [email protected] 5 Department of Clinical Immunology and Immunotherapy, Medical University of Lublin, 20-093 Lublin, Poland; [email protected] 6 Department of Anesthesiology and Intensive Therapy, Pomeranian Medical University in Szczecin, 71-252 Szczecin, Poland; [email protected] 7 Clinical Department of Nephrology, Transplantology and Internal Medicine, Pomeranian Medical University, 70-111 Szczecin, Poland; [email protected] 8 Department of Infectious, Tropical Diseases and Immune Deficiency, Pomeranian Medical University in Szczecin, 71-455 Szczecin, Poland; [email protected] * Correspondence: katarzyna.kotfi[email protected]; Tel.: +48-91-466-11-44 Abstract: In March 2020, coronavirus disease 2019 (COVID-19) caused by SARS-CoV-2 was declared Citation: Kotfis, K.; Lechowicz, K.; a global pandemic by the World Health Organization (WHO). The clinical course of the disease is Drozd˙ zal,˙ S.; Nied´zwiedzka-Rystwej, unpredictable but may lead to severe acute respiratory infection (SARI) and pneumonia leading to P.; Wojdacz, T.K.; Grywalska, E.; acute respiratory distress syndrome (ARDS). -

Hormonal Treatment Strategies Tailored to Non-Binary Transgender Individuals
Journal of Clinical Medicine Review Hormonal Treatment Strategies Tailored to Non-Binary Transgender Individuals Carlotta Cocchetti 1, Jiska Ristori 1, Alessia Romani 1, Mario Maggi 2 and Alessandra Daphne Fisher 1,* 1 Andrology, Women’s Endocrinology and Gender Incongruence Unit, Florence University Hospital, 50139 Florence, Italy; [email protected] (C.C); jiska.ristori@unifi.it (J.R.); [email protected] (A.R.) 2 Department of Experimental, Clinical and Biomedical Sciences, Careggi University Hospital, 50139 Florence, Italy; [email protected]fi.it * Correspondence: fi[email protected] Received: 16 April 2020; Accepted: 18 May 2020; Published: 26 May 2020 Abstract: Introduction: To date no standardized hormonal treatment protocols for non-binary transgender individuals have been described in the literature and there is a lack of data regarding their efficacy and safety. Objectives: To suggest possible treatment strategies for non-binary transgender individuals with non-standardized requests and to emphasize the importance of a personalized clinical approach. Methods: A narrative review of pertinent literature on gender-affirming hormonal treatment in transgender persons was performed using PubMed. Results: New hormonal treatment regimens outside those reported in current guidelines should be considered for non-binary transgender individuals, in order to improve psychological well-being and quality of life. In the present review we suggested the use of hormonal and non-hormonal compounds, which—based on their mechanism of action—could be used in these cases depending on clients’ requests. Conclusion: Requests for an individualized hormonal treatment in non-binary transgender individuals represent a future challenge for professionals managing transgender health care. For each case, clinicians should balance the benefits and risks of a personalized non-standardized treatment, actively involving the person in decisions regarding hormonal treatment. -

Epigenetic Therapy with Panobinostat Combined with Bicalutamide Rechallenge in Castration- Resistant Prostate Cancer Anna C
Published OnlineFirst January 3, 2019; DOI: 10.1158/1078-0432.CCR-18-1589 Clinical Trials: Targeted Therapy Clinical Cancer Research Epigenetic Therapy with Panobinostat Combined with Bicalutamide Rechallenge in Castration- Resistant Prostate Cancer Anna C. Ferrari1, Joshi J. Alumkal2, Mark N. Stein3, Mary-Ellen Taplin4, James Babb5, Ethan S. Barnett6, Alejandro Gomez-Pinillos5, Xiaomei Liu5, Dirk Moore6, Robert DiPaola7, and Tomasz M. Beer2 Abstract Purpose: This study assesses the action of panobino- Results: In the model, panobinostat/bicalutamide demon- stat, a histone deacetylase inhibitor (HDACI), in restor- strated synergistic antitumor effect while reducing AR activity. ing sensitivity to bicalutamide in a castration-resistant The dose-limiting toxicity was not reached. The probabilities of prostate cancer (CRPC) model and the efficacy and safety remaining rPF were 47.5% in the A arm and 38.5% in the B arm, of the panobinostat/bicalutamide combination in CRPC exceeding the protocol-specified threshold of 35%. The A arm patients resistant to second-line antiandrogen therapy but not the B arm exceeded expectations for times (medians) to (2ndLAARx). rP (33.9 and 10 weeks), and from PSA progression to rP (24 and Patients and Methods: The CWR22PC xenograft and 5.9 weeks). A arm/B arm events included: adverse events (AE), isogenic cell line were tested for drug interactions on 62%/19%; treatment stopped for AEs, 27.5%/11.5%; dose tumor cell growth and on the androgen receptor (AR), reduction required, 41%/4%. The principal A-arm grade 3 AR-splice variant7, and AR targets. A phase I trial had a AEs were thrombocytopenia (31%) and fatigue (14%). -

Feminizing Hormone Therapy
FEMINIZING HORMONE THERAPY Julie Thompson, PA-C Medical Director of Trans Health, Fenway Health April 2020 fenwayhealth.org GOALS AND OBJECTIVES 1. Review process of initiating hormone therapy through the informed consent model 2. Provide an overview of feminizing hormone therapy 3. Review realistic expectations and benefits of hormone therapy vs their associated risks 4. Discuss recommendations for monitoring fenwayhealth.org PROTOCOLS AND STANDARDS OF CARE fenwayhealth.org WPATH STANDARDS OF CARE, 2011 The criteria for hormone therapy are as follows: 1. Well-documented, persistent (at least 6mo) gender dysphoria 2. Capacity to make a fully informed decision and to consent for treatment 3. Age of majority in a given country 4. If significant medical or mental health concerns are present, they must be reasonably well controlled fenwayhealth.org INFORMED CONSENT MODEL ▪ Requires healthcare provider to ▪ Effectively communicate benefits, risks and alternatives of treatment to patient ▪ Assess that the patient is able to understand and consent to the treatment ▪ Informed consent model does not preclude mental health care! ▪ Recognizes that prescribing decision ultimately rests with clinical judgment of provider working together with the patient ▪ Recognizes patient autonomy and empowers self-agency ▪ Decreases barriers to medically necessary care fenwayhealth.org INITIAL VISITS ▪ Review history of gender experience and patient’s goals ▪ Document prior hormone use ▪ Assess appropriateness for gender affirming medical treatment ▪ WPATH criteria -

An Unexpected Target for Androgen Deprivation Therapy with Prognosis and Diagnostic Implications
Author Manuscript Published OnlineFirst on October 11, 2013; DOI: 10.1158/0008-5472.CAN-13-1462 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. 1 Androgen glucuronidation: an unexpected target for androgen deprivation therapy with prognosis and diagnostic implications. Laurent Grosse1, Sophie Pâquet1, Patrick Caron1, Ladan Fazli2, Paul S. Rennie2, Alain Bélanger3 and Olivier Barbier1 1Laboratory of Molecular Pharmacology, CHU-Québec Research Centre and Faculty of Pharmacy, Laval University, Québec, Canada 2 Vancouver Prostate Centre at VGH, University of British Columbia, Vancouver, British Columbia, Canada. 3CHU-Québec Research Centre and Faculty of Medicine, Laval University, Québec, Canada Running title: Ablation therapy improves androgen glucuronidation in PCa Keywords: Prostate cancer, androgen ablation therapy, glucuronidation, biomarker, drug target. Financial support: This study was supported by grants from the Canadian Institutes of Health Research (CIHR), the Terry Fox foundation and the Canadian Foundation for Innovation. S. Pâquet is holder of scholarships from CIHR and the Fonds pour la Recherche en Santé du Québec (FRSQ). L. Grosse is supported by a scholarship from the Fonds pour l’Enseignement et la Recherche (FER) from the Faculty of Pharmacy, Laval University (Québec). O. Barbier is holder of salary grants from the CIHR (New Investigator Award #MSH95330) and FRSQ (Junior 2 Scholarship). Address correspondence to: Olivier Barbier, Ph.D. Laboratory of Molecular Pharmacology CHU-Québec Research Centre 2705, boulevard Laurier Québec (QC) G1V 4G2, Canada Phone: 418 654 2296 Fax: 418 654 2769 Email: [email protected] Conflict of interests: Authors have nothing to disclose. Downloaded from cancerres.aacrjournals.org on September 26, 2021. -

WO 2018/111890 Al 21 June 2018 (21.06.2018) W !P O PCT
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2018/111890 Al 21 June 2018 (21.06.2018) W !P O PCT (51) International Patent Classification: EE, ES, FI, FR, GB, GR, HR, HU, IE, IS, IT, LT, LU, LV, C07K 16/28 (2006.01) A61K 31/4166 (2006.01) MC, MK, MT, NL, NO, PL, PT, RO, RS, SE, SI, SK, SM, 59/595 (2006.01) TR), OAPI (BF, BJ, CF, CG, CI, CM, GA, GN, GQ, GW, KM, ML, MR, NE, SN, TD, TG). (21) International Application Number: PCT/US20 17/065841 Declarations under Rule 4.17: (22) International Filing Date: — as to applicant's entitlement to apply for and be granted a 12 December 2017 (12.12.2017) patent (Rule 4.1 7(H)) — as to the applicant's entitlement to claim the priority of the (25) Filing Language: English earlier application (Rule 4.17(Hi)) (26) Publication Langi English — of inventorship (Rule 4.1 7(iv)) (30) Priority Data: Published: 62/433,158 12 December 2016 (12.12.2016) US — with international search report (Art. 21(3)) — with sequence listing part of description (Rule 5.2(a)) (71) Applicant (for all designated States except AL, AT, BE, BG, CH, CN, CY, CZ, DE, DK, EE, ES, FI, FR, GB, GR, HR, HU, IE, IN, IS, IT, LT, LU, LV, MC, MK, MT, NL, NO, PL, P T RO, RS, SE, SI, SK, SM, TR): GENENTECH, INC. [US/US]; 1 DNA Way, South San Francisco, CA 94080-4990 (US).