View HIV Sentinel Surveillance 2004 Country Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Newspaper Wise.Xlsx
PRINT MEDIA COMMITMENT REPORT FOR DISPLAY ADVT. DURING 2013-2014 CODE NEWSPAPER NAME LANGUAGE PERIODICITY COMMITMENT(%)COMMITMENTCITY STATE 310672 ARTHIK LIPI BENGALI DAILY(M) 209143 0.005310639 PORT BLAIR ANDAMAN AND NICOBAR 100771 THE ANDAMAN EXPRESS ENGLISH DAILY(M) 775695 0.019696744 PORT BLAIR ANDAMAN AND NICOBAR 101067 THE ECHO OF INDIA ENGLISH DAILY(M) 1618569 0.041099322 PORT BLAIR ANDAMAN AND NICOBAR 100820 DECCAN CHRONICLE ENGLISH DAILY(M) 482558 0.012253297 ANANTHAPUR ANDHRA PRADESH 410198 ANDHRA BHOOMI TELUGU DAILY(M) 534260 0.013566134 ANANTHAPUR ANDHRA PRADESH 410202 ANDHRA JYOTHI TELUGU DAILY(M) 776771 0.019724066 ANANTHAPUR ANDHRA PRADESH 410345 ANDHRA PRABHA TELUGU DAILY(M) 201424 0.005114635 ANANTHAPUR ANDHRA PRADESH 410522 RAYALASEEMA SAMAYAM TELUGU DAILY(M) 6550 0.00016632 ANANTHAPUR ANDHRA PRADESH 410370 SAKSHI TELUGU DAILY(M) 1417145 0.035984687 ANANTHAPUR ANDHRA PRADESH 410171 TEL.J.D.PATRIKA VAARTHA TELUGU DAILY(M) 546688 0.01388171 ANANTHAPUR ANDHRA PRADESH 410400 TELUGU WAARAM TELUGU DAILY(M) 154046 0.003911595 ANANTHAPUR ANDHRA PRADESH 410495 VINIYOGA DHARSINI TELUGU MONTHLY 18771 0.00047664 ANANTHAPUR ANDHRA PRADESH 410398 ANDHRA DAIRY TELUGU DAILY(E) 69244 0.00175827 ELURU ANDHRA PRADESH 410449 NETAJI TELUGU DAILY(E) 153965 0.003909538 ELURU ANDHRA PRADESH 410012 ELURU TIMES TELUGU DAILY(M) 65899 0.001673333 ELURU ANDHRA PRADESH 410117 GOPI KRISHNA TELUGU DAILY(M) 172484 0.00437978 ELURU ANDHRA PRADESH 410009 RATNA GARBHA TELUGU DAILY(M) 67128 0.00170454 ELURU ANDHRA PRADESH 410114 STATE TIMES TELUGU DAILY(M) -

7, Issue 266, Thursday, May 7, 2020 Maliyapham Palcha Kumsing 3418 Rs
Evening daily Imphal Times Regd.No. MANENG /2013/51092 Volume 7, Issue 266, Thursday, May 7, 2020 Maliyapham Palcha kumsing 3418 Rs. 2/- Manipuri woman dies in At least 8 dead, hundreds fall sick Mumbai’s KEM hospital after as toxic gas leaks in a chemical IT Correspondent Dr Pravin Bangar, Senior packed in a plastic bag Mumbai, May 7 Administrative Medical delays early Officer, KEM Hospital said decomposition of the plant in Vishakhapatnam Saya Begum, a 58-year-old that whether Saya Begum body an d prevents further woman from Manipur, who died of COVID-19 or other transmission of the virus. If Agency have been fully evacuated shock on the accident. Visakhapatnam Gas leak had accompanied her morbidity complications is the body has to be taken out Visakhapatnam, May 7 and shifted to other President Ram Nath mishap. husband to Mumbai’s KEM being verified. of the Mumbai city’s limits, places. Kovind has expressed Terming the incident as Hospital for the treatment As per the formalities the the relatives of the Eight people died and Several police personnel, sadness at the news of gas disturbing, Mr Shah said of her husband for COVID- last rites are required to be deceased have to make own around two hundred who came for the rescue leak in a plant near that Home Ministry is 19, reportedly passed away performed at the nearest transport arrangements, people fell sick in a major operation, also suffered Visakhapatnam which has continuously and closely on late Tuesday night. crematorium/ burial ground following all the mandated leak of Styrene vapour symptoms like claimed several lives. -

Newspaper Wise.Xlsx
PRINT MEDIA COMMITMENT REPORT FOR DISPLAY ADVT. DURING 2012-2013 CODE NEWSPAPER NAME LANGUAGE PERIODICITY COMMITMENT (%)COMMITMENTCITY STATE 310672 ARTHIK LIPI BENGALI DAILY(M) 67059 0.002525667 PORT BLAIR ANDAMAN AND NICOBAR 100771 THE ANDAMAN EXPRESS ENGLISH DAILY(M) 579134 0.021812132 PORT BLAIR ANDAMAN AND NICOBAR 101067 THE ECHO OF INDIA ENGLISH DAILY(M) 1172263 0.044151362 PORT BLAIR ANDAMAN AND NICOBAR 100820 DECCAN CHRONICLE ENGLISH DAILY(M) 373181 0.01405525 ANANTHAPUR ANDHRA PRADESH 410198 ANDHRA BHOOMI TELUGU DAILY(M) 390958 0.014724791 ANANTHAPUR ANDHRA PRADESH 410202 ANDHRA JYOTHI TELUGU DAILY(M) 172950 0.006513878 ANANTHAPUR ANDHRA PRADESH 410345 ANDHRA PRABHA TELUGU DAILY(M) 366211 0.013792736 ANANTHAPUR ANDHRA PRADESH 410370 SAKSHI TELUGU DAILY(M) 398436 0.015006438 ANANTHAPUR ANDHRA PRADESH 410171 TEL.J.D.PATRIKA VAARTHA TELUGU DAILY(M) 180263 0.00678931 ANANTHAPUR ANDHRA PRADESH 410400 TELUGU WAARAM TELUGU DAILY(M) 265972 0.010017399 ANANTHAPUR ANDHRA PRADESH 410495 VINIYOGA DHARSINI TELUGU MONTHLY 4172 0.000157132 ANANTHAPUR ANDHRA PRADESH 410398 ANDHRA DAIRY TELUGU DAILY(E) 297035 0.011187336 ELURU ANDHRA PRADESH 410280 HELAPURI NEWS TELUGU DAILY(E) 67795 0.002553387 ELURU ANDHRA PRADESH 410449 NETAJI TELUGU DAILY(E) 152550 0.005745545 ELURU ANDHRA PRADESH 410405 VASISTA TIMES TELUGU DAILY(E) 62805 0.002365447 ELURU ANDHRA PRADESH 410012 ELURU TIMES TELUGU DAILY(M) 369397 0.013912732 ELURU ANDHRA PRADESH 410117 GOPI KRISHNA TELUGU DAILY(M) 239960 0.0090377 ELURU ANDHRA PRADESH 410009 RATNA GARBHA TELUGU DAILY(M) 209853 -

GOVERNMENT of MIZORAM EDUCATION DEPARTMENT Niz- D
GOVERNMENT OF MIZORAM EDUCATION DEPARTMENT DRAFT ANNUAL PLAN 1984-85 - 64 EDUCATION INCLUDING ART & 3 1 9 - 1 5 (LiTUKE, t e c h n i c a l e d u c a t i o n . niz- D SI No. I,tea Page No» * V w U% khkhhh^hkhl 2 . Proposed outlay for staff & building 2 3. GGneral Introduction 3 - 6 4. Scheme-wise Description 6 - 35 5. Statement I 36 - 81 6. Statement II 82 »• 100 7. Statement III 101 - 124 8. GN. 1 125 - 9, GN. 2 126 10 . GN. 3 127 - 132 1 U GN. 4 1s33 - t43 1 2 . GN* 5 144 13. OH. 6 145 14. EMP. I 146 - 148 15. EMP. II 149 - 151 16. TPP. 1 152- 154 4 17. TPP. 2 155 - 157 18. DP. 1 158 - 159 19. DP, 2 160 20 . DP. 3 161 - 181 NIEPA DC nilD01775 ~ ■ t-' ^ ^ ^ 1 / ^ p> HilJiiorial Inptinite of Educalbiial jSiSjBtiAvitfwdt^* Marft.>^Delhi41^S »OCNo.../.V^>- -". d m *..........*,;X.)./>I4\ ABSTRACT OF DR/^,FT AN^W L PLAN ^ 1 9 B4 -S 5 1 r (rfe jETpdr" ’Expdr ' '1983-84 iT 1984 ....... No’ Name of scheme ’plan M980-. ,1981- ’'^982- Appro- *?ropo- f ’outlay’SI ,82 '83 ved *pated ’sed ^ h i c n tsl ^ t ? t outlay -Expdr ’outlay mi'TP conter^^‘ -...... -'T B -1 .... 7 < Elementary 4 5 6 0 0 6 2 4 9 8 8 .. 1 4 9 7 ^ 0 7 1 1 0 0 0 1 4 9 . 5 5 2 0 3 6 0 , i e f ) 3 6 0 - Z. -

Annexure-Iii
ANNEXURE-III LIST OF PUBLICATION UNITS TO WHOM QUESTIONAIRE WAS SENT SL.NO. NAME OF PUBLICATION PLACE CODE LANGUAGE CIRCULATION 1 Pledge Hyderabad 100076 ENG 50463 2 Hindi Milap Hyderabad 120304 HIN 31167 3 Siyasat Hyderabad 160006 URD 42744 4 Andhra Jyothi Hyderabad 410093 TEL 33281 5 Andhra Prabha Hyderabad 410014 TEL 25000 6 Prajashakti Hyderabad 410173 TEL 11387 7 Tel.J.D.Patrika Vaartha Hyderabad 410151 TEL 101241 8 Ushodayam S.Dina.Patrika Hyderabad 410148 TEL 30719 9 Andhra Prabha Karimnagar 410207 TEL 25000 10 Deccan Chronicle Secunderabad 100447 ENG 222849 11 Andhra Bhoomi Secunderabad 410119 TEL 8258 12 Neti Manadesam Vijayawada 410214 TEL 25000 13 Vijayabhanu Visakhapatnam 410007 TEL 65256 14 Visakha Samachram Visakhapatnam 410123 TEL 55500 15 Assam Tribune Guwahati 100050 ENG 58547 16 North East Times Guwahati 100442 ENG 8418 17 Sentinel Guwahati 100074 ENG 44483 18 Purvanchal Prahari Guwahati 122350 HIN 14679 19 AJI Guwahati 300074 ASS 54466 20 Ajir-Asom Guwahati 300036 ASS 11160 21 Amar Asom Guwahati 300071 ASS 46916 22 Asomiya Khabar Guwahati 300078 ASS 46999 23 Asomiya Pratidin Guwahati 300068 ASS 59910 24 Dainik Agradoot Guwahati 300069 ASS 25000 25 Dainik Asam Guwahati 300001 ASS 12376 26 Jugasankha Guwahati 310558 BEN 82681 27 Dainik Sonar Cachar Silchar 310005 BEN 25000 28 The Hindustan Times Patna 100215 ENG 25000 29 Qaumi Tanzeem Patna 160014 URD 46842 30 Sangam Patna 100010 URD 47091 31 The Asian Age Ahmedabad 100719 ENG 22936 32 Alp Viram Ahmedabad 123493 HIN 76843 33 Gujarat Vaibhav Ahmedabad 123908 HIN 231315 -

Role of Media and Government Towards Sustainable Development in Assam
IRA International Journal of Management & Social Sciences ISSN 2455-2267 Vol. 14, Issue 02 (Special Issue) pg. 161-170. International Conference on Wellbeing: Lifespan Perspectives & Practices for Sustainable Communities, 2019. Role of Media and Government towards Sustainable Development in Assam Mohsina Rahman Assistant Professor, Department of Mass Communication, Assam Women’s University, India. DOI: 10.21013/jmss.v14.n2sp.p16 © Authors. Type of Review: Peer Reviewed under the Responsibility of the conference’s Scientific Committee. Disclaimer: The copyright to this work is retained by the authorship. This work contains the opinions & views of the authorship solely and the same are not the views or opinions of the IRA. IRA disclaims of any harm or loss caused due to the published content to any party. International Conference on Wellbeing: Lifespan Perspectives & Practices for Sustainable Communities, 2019. Pg.161 IRA International Journal of Management & Social Sciences ABSTRACT The North-East of India has been a hotly debated territory of India with voices coming up from different states such as Nagaland, Manipur and Assam demanding separate nations for themselves. These separatist agitations have got further confounded with a constant influx of Muslim immigrants from Bangladesh which began to impinge on the local cultural identities and demographics. This resulted in a prolonged militancy coupled with agitations yielding space for the Pakistani/Sri Lanka/Bangladesh based militants to infiltrate into India through porous borders of the North East and engage some disgruntled ultra outfits in the North East to wage a battle against India. In fact, Naga agitation for separate country bears a lot of similarity with the LTTE‟s struggle for separate Eelam in Sri Lanka. -

Wp(C) 5890/2009
IN THE GAUHATI HIGH COURT (THE HIGH COURT OF ASSAM, NAGALAND, MIZORAM AND ARUNACHAL PRADESH) WRIT PETITION (C) NO.5890 OF 2009 Petitioner: Jahiruddin Ahmed, Son of Late Jehinuddin Ahmed, PO & PS- Dibrugarh, Pin-786005, District- Dibrugarh, Assam. By Advocate: Ms. S.P. Hussain. Respondents : 1. State of Assam, Represented by the Commissioner and Secretary to the Government of Assam, Forest Department, Dispur, Guwahati-06. 2. Principal Chief Conservator of Forests, Assam, Guwahati. 3. District Forest Officer, Dibrugarh, Assam. By Advocate: Ms. B. Dutta, GA, Assam. B E F O R E HON’BLE MR. JUSTICE UJJAL BHUYAN Date of hearing : 08-03-2013 Date of Judgment : 02.08.2013 J U D G M E N T AND O R D E R (ORAL) Heard Ms. S.P. Hussain, learned Counsel for the petitioner and Ms. B. Dutta, learned Government Advocate, Assam, who has also produced the record. 2. In this writ petition, petitioner seeks quashing of select list dated 17-12-2009 published by the Principal Chief Conservator of Forests and Head of Forest Force, Assam for the post of Forest Guard. Petitioner also seeks quashing of the selection and appointment of the candidates against the post of Forest Guard pursuant to the advertisements dated 02-02-2008 and 08-09-2008. 3. Case of the petitioner is that he was engaged as a casual worker in the Dibrugarh Forest Division under the Forest Department, Government of Assam in the year 2001. In the year 2006, considering his computer operating skill, service of the petitioner was utilized as a computer operator and he has been working as such since then. -

37 Index of Adjudications AR 29-Section14
Index of Adjudications AR29 (2007-08) Section14 SNO Parties Nature of Complaint Date of Decision Category Section 13 Section 14 1 Complaint of the Government of Principles and Publication 7/27/2007 Cautioned y Tripura, Home Department, Agartala against Syandan Patrika, Bengali Daily, Agartala 2 Complaint of Dr. S.P. Thirumala Principles and Publication 7/27/2007 Directions y Rao, Secretary General, Karnataka State Federation of Consumers’ Organization against Star of Mysore 3 Complaint of Shri Hazi Saiyyad Atik Principles and Publication 7/27/2007 Settled y Miyan Chisti, Dargah Sharif, Ajmer, Rajasthan against the editor, Dainik Bhaskar, Ajmer, Rajasthan 4 Complaint of Superintendent of Principles and Publication 7/27/2007 Dismissed-not pursued y Police and Collector, Bhind, Madhya Pradesh against Dainik Nav Bharat, Gwalior 5 Complaint of Superintendent of Principles and Publication 7/27/2007 Dismissed-not pursued y Police and Collector, Bhind, Madhya Pradesh against Dainik Nav Bharat, Gwalior 6 Complaint of the President, Jamat-e- Principles and Publication 7/27/2007 Upheld y Islami Hind, Guwahati against the editor, Dainik Pratidin, Guwahati 7 Complaint of Shri Prasana Kumar, Principles and Publication 7/27/2007 Sub-judice y Proprietor AGP Photobank, Malviya Nagar, New Delhi against Incredible India, Durga Dass Publications, New Delhi Page 1 of 13 SNO Parties Nature of Complaint Date of Decision Category Section 13 Section 14 8 Complaint reference from the Principles and Publication 7/27/2007 Closed y Ministry of Home Affairs/Information & Broadcasting, Government of India, New Delhi against Press Trust of India 9 Complaint reference from the Principles and Publication 7/27/2007 Closed y Ministry of Home Affairs/Information & Broadcasting, Government of India, New Delhi against The Tribune, Chandigarh 10 Complaint reference from the Principles and Publication 7/27/2007 Closed y Ministry of Home Affairs/Information & Broadcasting, Government of India, New Delhi against Rashtriya Sahara, Noida 11 Complaint of Dr. -
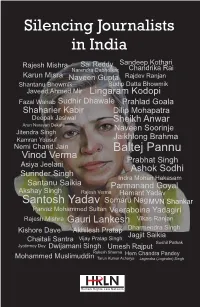
Silencing Journalists in India
In India, journalists have come under repeated attacks in the recent times. They have been killed, arrested, and Silencing Journalists wrongly implicated in many cases. There have been increasing number of criminal cases against journalists. in India Many media houses have seen their offices ransacked. It is sufficient to say that there have not been darker times for Sai Reddy Sandeep Kothari Rajesh Mishra Chandrika Rai journalists in India as it has been in the recent past and now. Narendra Dabholkar Karun Misra Rajdev Ranjan It is in this context that this compilation is brought out. This Naveen Gupta Shantanu Bhowmik Sudip Datta Bhowmik compilation brings out the stories of the journalists who Javeed Ahmed Mir Lingaram Kodopi have been arrested and killed for performing their duty. Attack on Journalists in India Fazal Wahab Sudhir Dhawale Prahlad Goala “Journalism can never be silent: That is its greatest virtue Shaharier Kabir Dilip Mohapatra and its greatest fault. It must speak, and speak immedi- Deepak Jasiwal Sheikh Anwar ately, while the echoes of wonder, the claims of triumph Arun Narayan Dekate Naveen Soorinje and the signs of horror are still in the air.” Jitendra Singh Kamran Yousuf Jaikhlong Brahma — Henry Anatole Grunwald, Nemi Chand Jain Baltej Pannu former Managing Editor, Time Magazine Vinod Verma Prabhat Singh “Journalism will kill you, but it will keep you alive while Asiya Jeelani Ashok Sodhi you’re at it.” Surinder Singh Indra Mohan Hakasam — Horace Greeley, Santanu Saikia Parmanand Goyal founder and editor of New -

Silencing Journalists in India
Silencing Journalists in India Violation of Journalists’ Rights in India 2000-2018 Human Rights Law Network (HRLN) In Parnership with Press Club of India, Delhi Union of Journalists, Indian Women Press Corps, Brihmumbai Journalists Union, Mumbai Press Club and Media Studies Group 1 HUMAN RIGHTS LAW NETWORK • To protect fundamental human rights, increase access to basic resources for the marginalised communities, and eliminate discrimination. • To create a justice delivery system that is accessible, accountable, transparent, efficient and affordable, and works for the underprivileged. Raise the level of pro bono legal expertise for the poor to make the work uniformly competent as well as compassionate. • Professionally train a new generation of public interest lawyers and paralegals who are comfortable in the world of law as well as in social movements, and who learn from social movements to refine legal concepts and strategies. Silencing Journalists in India September 2019 © Socio Legal Information Centre* Research: Bonnie Smith, Sarita Ramamoorthy, Laxmi Murthy, Aditi Saxena Editor: Laxmi Murthy ISBN No.: 97881-934737-0-2 Design & Printed at: Shivam Sundram Published by Human Rights Law Network (Division of Socio-Legal Information Centre) 576, Masjid Road, Jangpura New Delhi - 110014 Phone No: +91-11-24374501 Disclaimer Text has been compiled from various sources for the purpose of this book. Photographs used are from those available on the internet through a generic search. *Any section of this volume may be reproduced without prior permission of HRLN for public interest purposes with appropriate acknowledgment. 2 3 INTRODUCTION: A Dangerous Profession Journalism in India has always been a difficult calling. -

Sl No Code NEWSPAPER PUBLICATION Lan/Per
Home Back Print Statement showing the quantum of advertisements issued by DAVP to various newspapers/periodicals during the year 2012- 13 ------------------------------------------------------------------------------------------------------------- Sl No Code NEWSPAPER PUBLICATION Lan/Per INSERTIONS SPACE(sq.CM) Amount(Rs) ------------------------------------------------------------------------------------------------------------- State : ANDAMAN AND NICOBAR------------------------------------------------------ 1 310672 ARTHIK LIPI PORTBLAIR BEN/D 11 9,722.82 67,059.00 2 100771 THE ANDAMAN EXPRESS PORTBLAIR ENG/D 259 1,32,899.00 8,18,036.00 3 101067 THE ECHO OF INDIA PORTBLAIR ENG/D 343 1,70,361.00 16,21,012.00 State : ANDHRA PRADESH------------------------------------------------------ 1 410441 PRAJA JYOTHI ADILABAD TEL/D 38 24,505.00 3,21,598.00 2 410469 PRAJA JYOTHI ADILABAD TEL/W 2 816.00 6,228.00 3 410198 ANDHRA BHOOMI ANANTHAPUR TEL/D 73 42,095.40 4,07,428.00 4 410202 ANDHRA JYOTHI ANANTHAPUR TEL/D 23 13,325.00 1,98,441.00 5 410345 ANDHRA PRABHA ANANTHAPUR TEL/D 54 39,296.00 3,74,874.00 6 100820 DECCAN CHRONICLE ANANTHAPUR ENG/D 47 25,965.60 4,07,040.00 7 410370 SAKSHI ANANTHAPUR TEL/D 35 20,973.75 5,41,577.00 8 410171 TEL.J.D.PATRIKA VAARTHA ANANTHAPUR TEL/D 23 14,419.00 1,83,424.00 9 410400 TELUGU WAARAM ANANTHAPUR TEL/D 33 23,804.00 2,65,972.00 10 410495 VINIYOGA DHARSINI ANANTHAPUR TEL/M 1 408.00 4,172.00 11 410219 ANDHRA JYOTHI CUDDAPPAH TEL/D 25 14,346.00 1,81,268.00 12 410391 BHARATHA SAKTHI CUDDAPPAH TEL/D 11 6,321.00 85,465.00 -

Journalistic Ethics in Coverage of Communal Issues ( with Special Reference to Assam) Debahuti Chakravorty
Journalistic ethics in coverage of Communal issues ( With special reference to Assam) Debahuti chakravorty empowers anybody in the world to Abstract: broadcast any kind of information to With the media's role as an informa- the masses not only within the coun- tion provider and a watchdog, the try but also throughout the world. freedom of media is considered very This now poses a major challenge for important for democratic countries media to remain truly "ethical". like India. Recognized as the fourth In sensitive state like Assam, where pillar of the democracy, Indian media regional media is not so advanced, the has been playing a decisive role in local as well as social media have keeping the masses informed and been found to disseminate informa- aware, right from the days of British tion about incidents which regional rule. Being one of the most powerful media have not been able to cover tools for shaping public opinion, and some of the consequences of this Indian media shoulders a tremendous uncalled for spread of information responsibility towards the people of have been downright disastrous. The the country. And like any other power researcher in this research will discuss in the world, it needs to be regulated unethical practices by local media and or controlled to ensure ethical gather- social media while covering some ing and distribution of non-misrepre- communal issues of the state. The sented content for the enlightenment research paper will also give insights of the masses. about the consequences of such Journalistic ethics or media ethics act unethical practices of media.