Genetic Factors Modulate the Impact of Pubertal Androgen Excess on Insulin Sensitivity and Fertility
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Androgen Excess in Breast Cancer Development: Implications for Prevention and Treatment
26 2 Endocrine-Related G Secreto et al. Androgen excess in breast 26:2 R81–R94 Cancer cancer development REVIEW Androgen excess in breast cancer development: implications for prevention and treatment Giorgio Secreto1, Alessandro Girombelli2 and Vittorio Krogh1 1Epidemiology and Prevention Unit, Fondazione IRCCS – Istituto Nazionale dei Tumori, Milano, Italy 2Anesthesia and Critical Care Medicine, ASST – Grande Ospedale Metropolitano Niguarda, Milano, Italy Correspondence should be addressed to G Secreto: [email protected] Abstract The aim of this review is to highlight the pivotal role of androgen excess in the Key Words development of breast cancer. Available evidence suggests that testosterone f breast cancer controls breast epithelial growth through a balanced interaction between its two f ER-positive active metabolites: cell proliferation is promoted by estradiol while it is inhibited by f ER-negative dihydrotestosterone. A chronic overproduction of testosterone (e.g. ovarian stromal f androgen/estrogen balance hyperplasia) results in an increased estrogen production and cell proliferation that f androgen excess are no longer counterbalanced by dihydrotestosterone. This shift in the androgen/ f testosterone estrogen balance partakes in the genesis of ER-positive tumors. The mammary gland f estradiol is a modified apocrine gland, a fact rarely considered in breast carcinogenesis. When f dihydrotestosterone stimulated by androgens, apocrine cells synthesize epidermal growth factor (EGF) that triggers the ErbB family receptors. These include the EGF receptor and the human epithelial growth factor 2, both well known for stimulating cellular proliferation. As a result, an excessive production of androgens is capable of directly stimulating growth in apocrine and apocrine-like tumors, a subset of ER-negative/AR-positive tumors. -

139 Normal Bone Density in Male
SEPTEMBER-OCTOBER REV. HOSP. CLÍN. FAC. MED. S. PAULO 56(5):139-142, 2001 NORMAL BONE DENSITY IN MALE PSEUDOHERMAPHRODITISM DUE TO 5α- REDUCTASE 2 DEFICIENCY Elaine Maria Frade Costa, Ivo Jorge Prado Arnhold, Marlene Inacio and Berenice Bilharinho Mendonca RHCFAP/3050 COSTA EMF et al. - Normal bone density in male pseudohermaphroditism due to 5α-reductase 2 deficiency. Rev. Hosp. Clín. Fac. Med. S. Paulo 56(5):139-142, 2001. Bone is an androgen-dependent tissue, but it is not clear whether the androgen action in bone depends on testosterone or on dihydrotestosterone. Patients with 5α-reductase 2 deficiency present normal levels of testosterone and low levels of dihydrotestosterone, providing an in vivo human model for the analysis of the effect of testosterone on bone. Objective: To analyze bone mineral density in 4 adult patients with male pseudohermaphroditism due to 5α-reductase 2 deficiency. Results: Three patients presented normal bone mineral density of the lumbar column (L1-L4) and femur neck, and the other patient presented a slight osteopenia in the lumbar column. Conclusion: Patients with dihydrotestosterone deficiency present normal bone mineral density, suggesting that dihydrotestosterone is not the main androgen acting in bone. DESCRIPTOR: Bone mineral density. Male pseudohermaphroditism. 5α-reductase type 2 deficiency. It has been well documented in the fied androgenic receptors in these cells, fects require aromatization into estro- literature that gonadal steroids regulate thus demonstrating that both androgens gens with subsequent activation of the normal bone metabolism and that in- and estrogens act by a direct mecha- estrogenic receptor. Although it has adequate estrogen concentrations in fe- nism through their respective receptors. -

CYP19A1 Gene Cytochrome P450 Family 19 Subfamily a Member 1
CYP19A1 gene cytochrome P450 family 19 subfamily A member 1 Normal Function The CYP19A1 gene provides instructions for making an enzyme called aromatase. This enzyme converts a class of hormones called androgens, which are involved in male sexual development, to different forms of the female sex hormone estrogen. In cells, aromatase is found in a structure called the endoplasmic reticulum, which is involved in protein production, processing, and transport. The activity (expression) of aromatase varies among different cell types depending on the cells' need for estrogen. In females, aromatase is most active in the ovaries, where it guides sexual development. In males, aromatase is most active in fat (adipose) tissue. In both males and females, estrogen plays a role in regulating bone growth and blood sugar levels. During fetal development, aromatase converts androgens to estrogens in the placenta, which is the link between the mother's blood supply and the fetus. This conversion in the placenta prevents androgens from directing sexual development in female fetuses. After birth, the conversion of androgens to estrogens takes place in multiple tissues. Health Conditions Related to Genetic Changes Aromatase deficiency More than 20 mutations in the CYP19A1 gene have been found to cause aromatase deficiency. This condition is characterized by reduced levels of estrogen and increased levels of androgens. These abnormal hormone levels lead to impaired sexual development in affected females and unusual bone growth, insulin resistance, and other signs and symptoms in both males and females with the condition. CYP19A1 gene mutations that cause aromatase deficiency decrease or eliminate aromatase activity. A lack of aromatase function results in an inability to convert androgens to estrogens before birth and throughout life. -

Virilization and Enlarged Ovaries in a Postmenopausal Woman
Please do not remove this page Virilization and Enlarged Ovaries in a Postmenopausal Woman Guerrero, Jessenia; Marcus, Jenna Z.; Heller, Debra https://scholarship.libraries.rutgers.edu/discovery/delivery/01RUT_INST:ResearchRepository/12643454200004646?l#13643490680004646 Guerrero, J., Marcus, J. Z., & Heller, D. (2017). Virilization and Enlarged Ovaries in a Postmenopausal Woman. In International Journal of Surgical Pathology (Vol. 25, Issue 6, pp. 507–508). Rutgers University. https://doi.org/10.7282/T3125WCP This work is protected by copyright. You are free to use this resource, with proper attribution, for research and educational purposes. Other uses, such as reproduction or publication, may require the permission of the copyright holder. Downloaded On 2021/09/25 21:27:45 -0400 Virilization and Enlarged Ovaries in a Postmenopausal Woman Abstract: A patient with postmenopausal bleeding and virilization was found to have bilaterally enlarged ovaries with a yellow cut surface. Histology revealed cortical stromal hyperplasia with stromal hyperthecosis. This hyperplastic condition should not be mistaken for an ovarian neoplasm. Key words: Ovary, ovarian neoplasms, virilization Introduction Postmenopausal women who present with clinical manifestations of hyperandrogenism are often presumed to have an androgen-secreting tumor, particularly if there is ovarian enlargement. Gross findings in the ovaries can help exclude an androgen-secreting ovarian tumor and histologic findings can confirm the gross findings. Case A 64 year old woman with abnormal hair growth, male pattern baldness, clitorimegaly and postmenopausal bleeding presented to the clinic for evaluation of a possible hormone secreting tumor. Pre-operative work-up revealed bilateral ovarian enlargement, measuring 4 cm in greatest dimension, without evidence of an ovarian or adrenal tumor. -

A Novel Null Mutation in P450 Aromatase Gene (CYP19A1
J Clin Res Pediatr Endocrinol 2016;8(2):205-210 DO I: 10.4274/jcrpe.2761 Ori gi nal Ar tic le A Novel Null Mutation in P450 Aromatase Gene (CYP19A1) Associated with Development of Hypoplastic Ovaries in Humans Sema Akçurin1, Doğa Türkkahraman2, Woo-Young Kim3, Erdem Durmaz4, Jae-Gook Shin3, Su-Jun Lee3 1Akdeniz University Faculty of Medicine Hospital, Department of Pediatric Endocrinology, Antalya, Turkey 2Antalya Training and Research Hospital, Clinic of Pediatric Endocrinology, Antalya, Turkey 3 Inje University College of Medicine, Department of Pharmacology, Inje University, Busan, Korea 4İzmir University Faculty of Medicine, Medical Park Hospital, Clinic of Pediatric Endocrinology, İzmir, Turkey ABS TRACT Objective: The CYP19A1 gene product aromatase is responsible for estrogen synthesis and androgen/estrogen equilibrium in many tissues, particularly in the placenta and gonads. Aromatase deficiency can cause various clinical phenotypes resulting from excessive androgen accumulation and insufficient estrogen synthesis during the pre- and postnatal periods. In this study, our aim was to determine the clinical characteristics and CYP19A1 mutations in three patients from a large Turkish pedigree. Methods: The cases were the newborns referred to our clinic for clitoromegaly and labial fusion. Virilizing signs such as severe acne formation, voice deepening, and clitoromegaly were noted in the mothers during pregnancy. Preliminary diagnosis was aromatase deficiency. Therefore, direct DNA sequencing of CYP19A1 was performed in samples from parents (n=5) and patients (n=3). WHAT IS ALREADY KNOWN ON THIS TOPIC? Results: In all patients, a novel homozygous insertion mutation in the fifth exon (568insC) was found to cause a frameshift in the open reading frame and to truncate Aromatase deficiency can cause various clinical phenotypes the protein prior to the heme-binding region which is crucial for enzymatic activity. -

What Is and What Is Not PCOS (Polycystic Ovarian Syndrome)?
What is and What is not PCOS (Polycystic ovarian syndrome)? Chhaya Makhija, MD Assistant Clinical Professor in Medicine, UCSF, Fresno. No disclosures Learning Objectives • Discuss clinical vignettes and formulate differential diagnosis while evaluating a patient for polycystic ovarian syndrome. • Identify an organized approach for diagnosis of polycystic ovarian syndrome and the associated disorders. DISCUSSION Clinical vignettes of differential diagnosis Brief review of Polycystic ovarian syndrome (PCOS) Therapeutic approach for PCOS Clinical vignettes – Case based approach for PCOS Summary CASE - 1 • 25 yo Hispanic F, referred for 5 years of amenorrhea. Diagnosed with PCOS, was on metformin for 2 years. Self discontinuation. Seen by gynecologist • Progesterone withdrawal – positive. OCP’s – intolerance (weight gain, headache). Denies galactorrhea. Has some facial hair (upper lips) – no change since teenage years. No neurological symptoms, weight changes, fatigue, HTN, DM-2. • Currently – plans for conception. • Pertinent P/E – BMI: 24 kg/m², BP= 120/66 mm Hg. Fine vellus hair (upper lips/side burns). CASE - 1 Labs Values Range TSH 2.23 0.3 – 4.12 uIU/ml Prolactin 903 1.9-25 ng/ml CMP/CBC unremarkable Estradiol 33 0-400 pg/ml Progesterone <0.5 LH 3.3 0-77 mIU/ml FSH 2.8 0-153 mIU/ml NEXT BEST STEP? Hyperprolactinemia • Reported Prevalence of Prolactinomas: of clinically apparent prolactinomas ranges from 6 –10 per 100,000 to approximately 50 per 100,000. • Rule out physiological causes/drugs/systemic causes. Mild elevations in prolactin are common in women with PCOS. • MRI pituitary if clinically indicated (to rule out pituitary adenoma). Prl >100 ng/ml Moderate Mild Prl =50-100 ng/ml Prl = 20-50 ng/ml Typically associated with Low normal or subnormal Insufficient progesterone subnormal estradiol estradiol concentrations. -

PDF Hosted at the Radboud Repository of the Radboud University Nijmegen
PDF hosted at the Radboud Repository of the Radboud University Nijmegen The following full text is a publisher's version. For additional information about this publication click this link. http://hdl.handle.net/2066/148229 Please be advised that this information was generated on 2017-12-05 and may be subject to change. THE POLYCYSTIC OVARY SYNDROME SOME PATHOPHYSIOLOGICAL, DIAGNOSTICAI, AND THERAPEUTICAL ASPECTS M.J. HEINEMAN THE POLYCYSTIC OVARY SYNDROME SOME PATHOPHYSIOLOGICAL, DIAGNOSTICAL AND THERAPEUTICAL ASPECTS PROMOTOR PROF DR R ROLLAND THE POLYCYSTIC OVARY SYNDROME SOME PATHOPHYSIOLOGICAL, DIAGNOSTICAL AND THERAPEUTICAL ASPECTS PROEFSCHRIFT ICR VLRKRIIbING VAN Dì С.RAAD VAN DOCTOR IN DE GENEFSKUNDE AAN DE кАТНОІІНКЬ UMVERSIIHI IF NIJMEGEN OP GF/AG VAN DE RECTOR MAGNIFICUS PROF DR I H G I GlbbBERb VOI GENS BESLUIT \ΛΝ НЕТ COI LFGL \AN DI ( ANEN IN HET OPFNHAAR 11· VERDEDIGEN OP VRIJDAG 17 DECEMIH R I9S: DFS NAMIDDAGS TE 2 UUR PRFCIFS DOOR MAAS JAN HEINEMAN OEBORFN TF VFl Ρ (GFI DFRI AND) DRlk ΓΛΜΜΙΝΟΑ B\ ARMIfcM To the women who volunteered as subjects for this study, and to the many couples suffering from infertility who inspired me to undertake this investigation. WOORD VOORAF Het in dit proefschrift beschreven onderzoek vond plaats op de Poli kliniek voor Gynaecologische Endocrinologie en Infertiliteit (hoofd: Prof. Dr. R. Rolland) van het Instituut voor Obstetric en Gynaecologie (hoofden: Prof. Dr. Т.К. A.B. Eskes en Prof. Dr. J.L. Mastboom) van het Sint Radboudziekenhuis, Katholieke Universiteit, Nijmegen. Het was voor mij een unieke ervaring te ondervinden welke enorme mogelijkheden er binnen de Medische Faculteit en in het bijzonder bin nen het Instituut voor Obstetric en Gynaecologie bestaan tot het ver richten van wetenschappelijk onderzoek. -
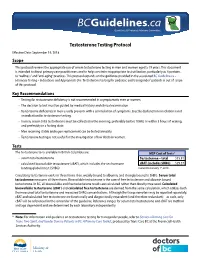
2. Testosterone Testing
Guidelines & Protocols Advisory Committee Testosterone Testing Protocol Effective Date: September 19, 2018 Scope This protocol reviews the appropriate use of serum testosterone testing in men and women aged ≥ 19 years. This document is intended to direct primary care practitioners and to help constrain inappropriate test utilization, particularly as it pertains to “wellness” and “anti-aging” practices. This protocol expands on the guidance provided in the associated BC Guideline.ca – Hormone Testing – Indications and Appropriate Use. Testosterone testing for pediatric and transgender* patients is out of scope of this protocol. Key Recommendations • Testing for testosterone deficiency is not recommended in asymptomatic men or women. • The decision to test must be guided by medical history and clinical examination. • Testosterone deficiency in men usually presents with a constellation of symptoms. Erectile dysfunction in isolation is not an indication for testosterone testing. • In men, serum total testosterone must be collected in the morning, preferably before 10AM, or within 3 hours of waking, and preferably in a fasting state. • Men receiving stable androgen replacement can be tested annually. • Testosterone testing is not useful for the investigation of low libido in women. Tests The testosterone tests available in British Columbia are: MSP Cost of Tests1 • serum total testosterone Testosterone – total $15.81 • calculated bioavailable testosterone (cBAT), which includes the sex hormone cBAT (includes SHBG) $29.37 binding globulin test (SHBG) Current to January 1st, 2018 Circulating testosterone exists in three forms: free, weakly bound to albumin, and strongly bound to SHBG. Serum total testosterone measures all three forms. Bioavailable testosterone is the sum of free testosterone and albumin bound testosterone. -

Unravelling the Link Between Insulin Resistance and Androgen Excess
Unravelling the link between insulin resistance and androgen excess by Michael O’Reilly A thesis submitted to The University of Birmingham for the degree of DOCTOR OF PHILOSOPHY School of Clinical and Experimental Medicine College of Medical and Dental Sciences The University of Birmingham August 2015 University of Birmingham Research Archive e-theses repository This unpublished thesis/dissertation is copyright of the author and/or third parties. The intellectual property rights of the author or third parties in respect of this work are as defined by The Copyright Designs and Patents Act 1988 or as modified by any successor legislation. Any use made of information contained in this thesis/dissertation must be in accordance with that legislation and must be properly acknowledged. Further distribution or reproduction in any format is prohibited without the permission of the copyright holder. Abstract Abstract Insulin resistance and androgen excess are the cardinal phenotypic features of polycystic ovary syndrome (PCOS). The severity of hyperandrogenism and metabolic dysfunction in PCOS are closely correlated. Aldoketoreductase type 1C3 (AKR1C3) is an important source of androgen generation in human adipose tissue, and may represent a link between androgen metabolism and metabolic disease in PCOS. We performed integrated in vitro studies using a human preadipocyte cell line and primary cultures of human adipocytes, coupled with in vivo deep phenotyping of PCOS women and age- and BMI-matched controls. We have shown that insulin upregulates AKR1C3 activity in primary female subcutaneous adipocytes. AKR1C3 mRNA expression increased with obesity. Androgens were found to increase lipid accumulation in human adipocytes. In clinical studies, androgen exposure induced relative suppression of adipose lipolysis in PCOS women, supporting a role for androgens in lipid accumulation. -

46,XX DSD and Antley-Bixler Syndrome Due to Novel Mutations In
case report 46,XX DSD and Antley-Bixler syndrome due to novel mutations in the cytochrome P450 oxidoreductase gene DDS 46,XX e síndrome de Antley-Bixler causada por novas mutações no gene da enzima P450 oxidorredutase Guilherme Guaragna-Filho1,2, Carla Cristina Telles de Sousa Castro1,2, Rodrigo Ribeiro De Carvalho3, Fernanda Borchers Coeli3, Lúcio Fábio Caldas Ferraz3, Reginaldo José Petroli3, Maricilda Palandi De Mello3, Letícia Esposito Sewaybricker1,2, Sofia Helena Valente Lemos-Marini1,Lilia Freire Rodrigues D'Souza-Li1, Márcio Lopes Miranda4, Andréa Trevas Maciel-Guerra2,5, Gil Guerra-Junior1,2 SUMMARY 1 Departamento de Pediatria, Deficiency of the enzyme P450 oxidoreductase is a rare form of congenital adrenal Unidade de Endocrinologia hyperplasia with characteristics of combined and partial impairments in steroidogenic Pediátrica, Faculdade de Ciências Médicas, Universidade enzyme activities, as P450 oxidoreductase transfers electrons to CYP21A2, CYP17A1, Estadual de Campinas (FCM- and CYP19A1. It results in disorders of sex development and skeletal malformations Unicamp), Campinas, SP, Brazil similar to Antley-Bixley syndrome. We report the case of a 9-year-old girl who was born 2 Grupo Interdisciplinar de Estudos da Determinação e Diferenciação with virilized genitalia (Prader stage V), absence of palpable gonads, 46,XX karyotype, do Sexo (GIEDDS), FCM- and hypergonadotropic hypogonadism. During the first year of life, ovarian cyst, par- Unicamp, Campinas, SP, Brazil tial adrenal insufficiency, and osteoarticular changes, such as mild craniosynostosis, 3 Centro de Biologia Molecular e carpal and tarsal synostosis, and limited forearm pronosupination were observed. Her Engenharia Genética (CBMEG), Unicamp, Campinas, SP, Brazil mother presented severe virilization during pregnancy. -

Aromatase Deficiency, a Rare Syndrome: Case Report
J Clin Res Pediatr Endocrinol 2013;5(2):129-132 DO I: 10.4274/Jcrpe.970 Case Report Aromatase Deficiency, a Rare Syndrome: Case Report Emine Kartal Baykan1, Mehmet Erdoğan1, Samim Özen2, Şükran Darcan2, L. Füsun Saygılı1 1Ege University Faculty of Medicine, İnternal Medicine Department of Endocrinology and Metabolism Unit, İzmir, Turkey 2Ege University Faculty of Medicine, Department of Pediatric Endocrinology and Metabolism Unit, İzmir, Turkey Introduction Aromatase deficiency (AD) is a rare syndrome. Its incidence is not known worldwide, and there are only a limited number of case reports in the literature. In these ABS TRACT patients, due to CYP19A1 gene mutation, abnormal protein Aromatase deficiency (AD) is a rare autosomal recessive inheritance synthesis occurs leading to aromatase dysfunction and syndrome. Its worldwide incidence is unknown, and there are few case reports in the literature. Aromatase dysfunction develops due consequently to a decrease in estrogen synthesis (1). to CYP19A1 gene mutation and a decrease in estrogen synthesis. Due to estrogen deficiency, disorders of sex development Estrogen deficiency can induce delayed epiphyseal closure, eunuchoid and progressive virilization at puberty develop in females. body habitus, osteopenia, and osteoporosis in both genders. Our patient In the males, prepubertal development is normal. Delayed was a 27-year-old male who presented with bone pain, recurrent bone fractures associated with minimal trauma starting in puberty, and epiphyseal closure, eunuchoid body habitus, osteopenia, a progressive increase in height. Laboratory tests revealed that the and osteoporosis develop in both genders (2). In this blood levels of follicle-stimulating hormone and luteinizing hormone presentation, in the context of the case report of a patient were above normal, testosterone level was normal, and estrogen with aromatase deficiency-related delayed epiphyseal closure was undetectable. -

Molecular Basis of Aromatase Deficiency in an Adult Female with Sexual Infantilism and Polycystic Ovaries YUJI ITO*T, CAROLYN R
Proc. Natl. Acad. Sci. USA Vol. 90, pp. 11673-11677, December 1993 Genetics Molecular basis of aromatase deficiency in an adult female with sexual infantilism and polycystic ovaries YUJI ITO*t, CAROLYN R. FISHER*t, FELIX A. CONTEt, MELVIN M. GRUMBACH*, AND EVAN R. SIMPSON*t§ *The Cecil H. and Ida Green Center for Reproductive Biology Sciences, and tThe Departments of Obstetrics/Gynecology and Biochemistry, The University of Texas Southwestern Medical Center, 5323 Harry Hines Boulevard, Dallas, TX 75235; and *Department of Pediatrics, University of California at San Francisco, San Francisco, CA 94143 Communicated by Ronald W. Estabrook, September 10, 1993 (receivedfor review July 20, 1993) ABSTRACT We identified two mutations in the CYP19 most other species, estrogen biosynthesis does not occur in gene responsible for aromatase deficiency in an 18-year-old such a wide distribution of tissues, but rather is limited to at 46,XX female with ambiguous external genitalia at birth, pri- most two sites (namely, the gonads and the brain). We have mary amenorrhea and sexual infantilism, and polycystic ova- presented evidence that the tissue-specific expression of the ries. The coding exons, namely exons II-X, of the CYP19 gene CYP19 gene is regulated, in part, by the use oftissue-specific were amplified by PCR from genomic DNA and sequenced promoters through mechanisms involving alternative splicing directy. Direct sequencing of the ampled DNA from the (16). Thus, whereas expression in the ovary is driven by a patient revealed two single-base changes, at bp 1303 (C-+ T) and proximal promoter, expression in placenta involves a distal bp 1310 (G -p A) in exon X, which were newly found missense element at least 40 kb upstream from the start of translation.