Optimizing a Disease Severity Scale for Evaluating Travelers' Diarrhea in Adults Nicole Maier Walden University
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Fecal Incontinence/Anal Incontinence
Fecal Incontinence/Anal Incontinence What are Fecal incontinence/ Anal Incontinence? Fecal incontinence is inability to control solid or liquid stool. Anal incontinence is the inability to control gas and mucous in addition to the inability to control stool. The symptoms range from mild release of gas to a complete loss of control. It is a common problem affecting 1 out of 13 women under the age of 60 and 1 out of 7 women over the age of 60. Men can also be have this condition. Anal incontinence is a distressing condition that can interfere with the ability to work, do daily activities and enjoy social events. Even though anal incontinence is a common condition, people are uncomfortable discussing this problem with family, friends, or doctors. They often suffer in silence, not knowing that help is available. Normal anatomy The anal sphincters and puborectalis are the primary muscles responsible for continence. There are two sphincters: the internal anal sphincter, and the external anal sphincter. The internal sphincter is responsible for 85% of the resting muscle tone and is involuntary. This means, that you do not have control over this muscle. The external sphincter is responsible for 15% of your muscle tone and is voluntary, meaning you have control over it. Squeezing the puborectalis muscle and external anal sphincter together closes the anal canal. Squeezing these muscles can help prevent leakage. Puborectalis Muscle Internal Sphincter External Sphincter Michigan Bowel Control Program - 1 - Causes There are many causes of anal incontinence. They include: Injury or weakness of the sphincter muscles. Injury or weakening of one of both of the sphincter muscles is the most common cause of anal incontinence. -

Utility of the Digital Rectal Examination in the Emergency Department: a Review
The Journal of Emergency Medicine, Vol. 43, No. 6, pp. 1196–1204, 2012 Published by Elsevier Inc. Printed in the USA 0736-4679/$ - see front matter http://dx.doi.org/10.1016/j.jemermed.2012.06.015 Clinical Reviews UTILITY OF THE DIGITAL RECTAL EXAMINATION IN THE EMERGENCY DEPARTMENT: A REVIEW Chad Kessler, MD, MHPE*† and Stephen J. Bauer, MD† *Department of Emergency Medicine, Jesse Brown VA Medical Center and †University of Illinois-Chicago College of Medicine, Chicago, Illinois Reprint Address: Chad Kessler, MD, MHPE, Department of Emergency Medicine, Jesse Brown Veterans Hospital, 820 S Damen Ave., M/C 111, Chicago, IL 60612 , Abstract—Background: The digital rectal examination abdominal pain and acute appendicitis. Stool obtained by (DRE) has been reflexively performed to evaluate common DRE doesn’t seem to increase the false-positive rate of chief complaints in the Emergency Department without FOBTs, and the DRE correlated moderately well with anal knowing its true utility in diagnosis. Objective: Medical lit- manometric measurements in determining anal sphincter erature databases were searched for the most relevant arti- tone. Published by Elsevier Inc. cles pertaining to: the utility of the DRE in evaluating abdominal pain and acute appendicitis, the false-positive , Keywords—digital rectal; utility; review; Emergency rate of fecal occult blood tests (FOBT) from stool obtained Department; evidence-based medicine by DRE or spontaneous passage, and the correlation be- tween DRE and anal manometry in determining anal tone. Discussion: Sixteen articles met our inclusion criteria; there INTRODUCTION were two for abdominal pain, five for appendicitis, six for anal tone, and three for fecal occult blood. -

2.04.26 Fecal Analysis in the Diagnosis of Intestinal Dysbiosis and Irritable Bowel Syndrome
MEDICAL POLICY – 2.04.26 Fecal Analysis in the Diagnosis of Intestinal Dysbiosis and Irritable Bowel Syndrome BCBSA Ref. Policy: 2.04.26 Effective Date: July 1, 2021 RELATED MEDICAL POLICIES: Last Revised: June 8, 2021 None Replaces: N/A Select a hyperlink below to be directed to that section. POLICY CRITERIA | DOCUMENTATION REQUIREMENTS | CODING RELATED INFORMATION | EVIDENCE REVIEW | REFERENCES | HISTORY ∞ Clicking this icon returns you to the hyperlinks menu above. Introduction Intestinal dysbiosis is a condition that occurs when the microorganisms in the digestive tract are out of balance. This condition is believed to cause diseases of the digestive tract, including poor nutrient absorption, overgrowth of certain bacteria, and irritable bowel syndrome (IBS). Symptoms of these digestive problems are similar and may include: abdominal pain, excess gas, bloating, and changes in bowel movements (constipation or diarrhea, or both). One method of diagnosing digestive disorders is by testing a fecal sample. Using fecal analysis to diagnose intestinal dysbiosis, IBS, malabsorption, or small intestinal overgrowth of bacteria is unproven (investigational). More studies are needed to see if this testing improves health outcomes. Note: The Introduction section is for your general knowledge and is not to be taken as policy coverage criteria. The rest of the policy uses specific words and concepts familiar to medical professionals. It is intended for providers. A provider can be a person, such as a doctor, nurse, psychologist, or dentist. A provider also can be a place where medical care is given, like a hospital, clinic, or lab. This policy informs them about when a service may be covered. -

Diagnostic Approach to Chronic Constipation in Adults NAMIRAH JAMSHED, MD; ZONE-EN LEE, MD; and KEVIN W
Diagnostic Approach to Chronic Constipation in Adults NAMIRAH JAMSHED, MD; ZONE-EN LEE, MD; and KEVIN W. OLDEN, MD Washington Hospital Center, Washington, District of Columbia Constipation is traditionally defined as three or fewer bowel movements per week. Risk factors for constipation include female sex, older age, inactivity, low caloric intake, low-fiber diet, low income, low educational level, and taking a large number of medications. Chronic constipa- tion is classified as functional (primary) or secondary. Functional constipation can be divided into normal transit, slow transit, or outlet constipation. Possible causes of secondary chronic constipation include medication use, as well as medical conditions, such as hypothyroidism or irritable bowel syndrome. Frail older patients may present with nonspecific symptoms of constipation, such as delirium, anorexia, and functional decline. The evaluation of constipa- tion includes a history and physical examination to rule out alarm signs and symptoms. These include evidence of bleeding, unintended weight loss, iron deficiency anemia, acute onset constipation in older patients, and rectal prolapse. Patients with one or more alarm signs or symptoms require prompt evaluation. Referral to a subspecialist for additional evaluation and diagnostic testing may be warranted. (Am Fam Physician. 2011;84(3):299-306. Copyright © 2011 American Academy of Family Physicians.) ▲ Patient information: onstipation is one of the most of 1,028 young adults, 52 percent defined A patient education common chronic gastrointes- constipation as straining, 44 percent as hard handout on constipation is 1,2 available at http://family tinal disorders in adults. In a stools, 32 percent as infrequent stools, and doctor.org/037.xml. -

Review Article:Posterior Tibial Nerve Stimulation in Fecal Incontinence
Basic and Clinical September, October 2019, Volume 10, Number 5 Review Article: Posterior Tibial Nerve Stimulation in Fecal Incontinence: A Systematic Review and Meta-Analysis Arash Sarveazad1 , Asrin Babahajian2 , Naser Amini3 , Jebreil Shamseddin4 , Mahmoud Yousefifard5* 1. Colorectal Research Center, Iran University of Medical Sciences, Tehran, Iran. 2. Liver and Digestive Research Center, Research Institute for Health Development, Kurdistan University of Medical Sciences, Sanandaj, Iran. 3. Cellular and Molecular Research Center, Iran University of Medical Sciences, Tehran, Iran. 4. Molecular Medicine Research Center, Hormozgan Health Institute, Department of Parasitology, Faculty of Medicine, Hormozgan University of Medical Sciences, Bandar Abbas, Iran. 5. Physiology Research Center, Iran University of Medical Sciences, Tehran, Iran. Use your device to scan and read the article online Citation: Sarveazad, A., Babahajian, A., Amini, N., Shamseddin, J., & Yousefifard, M. (2019). Posterior Tibial Nerve Stimula- tion in Fecal Incontinence: A Systematic Review and Meta-Analysis. Basic and Clinical Neuroscience, 10(5), 419-432. http:// dx.doi.org/10.32598/bcn.9.10.290 : http://dx.doi.org/10.32598/bcn.9.10.290 A B S T R A C T Introduction: The present systematic review and meta-analysis aims to investigate the role of Posterior Tibial Nerve Stimulation (PTNS) in the control ofF ecal Incontinence (FI). Article info: Received: 29 Apr 2018 Methods: Two independent reviewers extensively searched in the electronic databases of Medline, Embase, Cochrane Central Register of Controlled Trials (CENTRAL), Web First Revision:15 May 2018 of Science, CINAHL, and Scopus for the studies published until the end of 2016. Only 28 Sep 2018 Accepted: randomized clinical trials were included. -

Colonic and Anorectal Manifestations of Systemic Sclerosis
Current Gastroenterology Reports (2019) 21: 33 https://doi.org/10.1007/s11894-019-0699-0 LARGE INTESTINE (B CASH AND R CHOKSHI, SECTION EDITORS) Colonic and Anorectal Manifestations of Systemic Sclerosis Beena Sattar1 & Reena V. Chokshi2 Published online: 8 July 2019 # Springer Science+Business Media, LLC, part of Springer Nature 2019 Abstract Purpose of Review Systemic sclerosis is a chronic autoimmune disorder commonly involving the gastrointestinal tract, including the colon and anorectum. In this review, we summarize major clinical manifestations and highlight recent develop- ments in physiology, diagnostics, and treatment. Recent Findings The exact pathophysiology of systemic sclerosis is unclear and likely multifactorial. The role of the microbiome on gastrointestinal manifestations has led to a better understanding of potential pathogenic gut flora. Carbohydrate malabsorption is common. Evaluation using fecal calprotectin and high-resolution anorectal manometry may broaden our understanding of the etiologies of diarrhea and fecal incontinence and help with early recognition of pathology. Prucalopride, a high-affinity 5HT4 agonist, and pyridostigmine, an acetylcholinesterase inhibitor, may help improve colonic transit in patients with constipation. Intravenous immunoglobulins have been used to target muscarinic receptor antibodies that are believed to contribute to gastrointestinal dysmotility. Summary Colonic and anorectal manifestations of systemic sclerosis include constipation, diarrhea, and fecal incontinence, and can diminish quality of life for these patients. Recent studies regarding pathophysiology as well as diagnostic and treatment options are promising. Further targeted studies to facilitate early intervention and better management of refractory symptoms are still needed. Keywords Constipation . Diarrhea . Fecal incontinence . Anorectal . Scleroderma . Systemic sclerosis Introduction frequently involved, followed by the anorectum and small bowel. -

Pneumatosis Cystoides Intestinalis
IMAGE OF THE MONTH Annals of Gastroenterology (2020) 33, 1 Pneumatosis cystoides intestinalis Shunsuke Yamamotoa, Yusuke Takahashib, Hisashi Ishidaa National Hospital Organization Osaka National Hospital, Osaka, Japan A 70-year-old woman was referred to our hospital for further examinations because of findings from a previous examination. She had undergone colonoscopy at another hospital for fecal incontinence and multiple submucosal lesions had been found in the ascending colon. Colonoscopy showed several spherical or hump-shaped cystic lesions with diameters of 5-30 mm in the ascending colon (Fig. 1). All of them had normal surficial structures without erosions or ulcerations. Abdominal computed tomography revealed air-filled cysts within the bowel wall of the ascending colon (Fig. 2). From Figure 1 Colonoscopic images of multiple cystic lesions with diameters these findings, we diagnosed the case as pneumatosis cystoides of 5-30 mm in the ascending colon intestinalis (PCI). The etiology for the disease was unclear in this case. Since the patient did not have any specific symptoms directly related to the disease, we observed her conservatively. PCI is a rare disease characterized by cysts filled with gas in the intestinal wall. The following are considered as etiological factors for PCI: digestive tract stenosis, obstructive pulmonary disease, abdominal external injury or surgery, immunosuppression, systemic chemotherapy, and malnutrition [1-3]. As regards the pathogenesis, infiltration of intraluminal air into the injured mucosa and an invasion of gas-producing bacteria into the bowel wall have been described [2,3]. There is no standardized treatment strategy for the disease; however, most cases are free of symptoms and therefore can be managed conservatively. -

An Osteopathic Approach to Reduction of Readmissions for Neonatal Jaundice
Osteopathic Family Physician (2013) 5, 17–23 REVIEW ARTICLE An osteopathic approach to reduction of readmissions for neonatal jaundice Rachel Click, DO,a Julie Dahl-Smith, DO,a Lindsay Fowler, DO,a Jacqueline DuBose, MD,a Margi Deneau-Saxton, RN, CCCE, CIMI, CLC, CPD,b Jennifer Herbert, MDc From aGeorgia Health Sciences University, Medical College of Georgia, Department of Family Medicine, GA; bGeorgia Health System, OB Labor and Delivery, GA; and cUniversity Primary Care, Evans, GA. KEYWORDS: Jaundice is a potentially life-threatening condition that continues to affect at-risk newborns, accounting Breastfeeding; for continued hospital readmissions. As family physicians, we should be cognizant of neonates who may Jaundice; be at risk for jaundice, including those with pathologic jaundice as well as newborns of breastfeeding Prevention; mothers, and ensure sufficient intervention is taken to help prevent further elevations in bilirubin levels. Hyperbilirubinemia; Interventions are likely to include evaluation for sepsis, education regarding feeding frequencies for both Neonatal massage breast- and bottle-fed neonates, reviewing maternal and hematologic risk factors for neonatal jaundice, and considering inborn errors of metabolism. An additional measure family physicians may consider is that of neonatal massage for those with elevated bilirubin levels. Neonatal massage, though not widely used, has been proven to promote excess bilirubin excretion, thus decreasing length of hospital stay; all the while, providing an intervention that allows parents to take an active role. r 2013 Elsevier Inc. All rights reserved. Introduction morbidity rate with bilirubin 4 20 mg/dL. “It has been estimated that the risk of kernicterus in infants with total Jaundice is a product of excess bilirubin (a product of serum bilirubin (TSB) greater than 30 mg/dL is about 1 in broken down red blood cells), which manifests as a 7 infants”.1 Less serious complications of hyperbilirubine- yellowing of the skin and eyes. -

INFORMED CARING JAUNDICE Neonatal Jaundice BILIARY
1 INFORMED CARING Situations with Adults and Children with Gallbladder, Liver and Pancreatic Disorders 2 JAUNDICE ä Does NOT mean hepatitis ä Increased breakdown of RBCs ä Altered bilirubin breakdown ä Impeded flow through liver or bile duct ä First seen in sclera, then skin 3 Neonatal Jaundice ä Not liver failure ä RBC breakdown ä Phototherapy 4 BILIARY ATRESIA ä Jaundice 2-3 weeks after birth ä Easy bruising ä Stools putty like ä Tea colored urine ä Abdominal/organ distension 5 4 F’s of Gallbladder ä Fair ä Fat X size of person X amount in diet ä Fertile X BCP X Multiparity ä Forty 6 Cholelithiasis ä Calculi within the duct or gallbladder ä Severe colicky, cramp-like pain X radiates to shoulder blade X Murphy's sign ä Cholecystitis: inflammation X Can be caused by trauma, fasting, TPN or abdominal surgery 7 Diagnostic Studies ä Ultrasound of abdomen 1 X not for the obese ä HIDA scan X nuclear medicine ä Cholangiograms X endoscopic X transvenous X intraoperative 8 Post-op Care ä High abdominal incision X respiratory compromise ä T-tube X patients need to know how to empty it X may clamp it prior to removal X caution not dislodged with movements ä NO Morphine X spasms of sphincter of Oddi 9 Post-op Nutrition ä Limited fat in diet X can have rapid transit times ä Potential fat soluble vitamin deficit X A, D, E and K ä Weight loss diet 10 LIVER FAILURE ä Cirrhosis ä Drug toxicity X acetaminophen, anesthetics, HCTZ, chemotherapy ä Infection ä Cancer ä ETOH is single most linked cause 11 LIVER FAILURE S/S ä Don’t show up until 80-90% failed -

Symptomatic Approach to Gas, Belching and Bloating 21
20 Osteopathic Family Physician (2019) 20 - 25 Osteopathic Family Physician | Volume 11, No. 2 | March/April, 2019 Gennaro, Larsen Symptomatic Approach to Gas, Belching and Bloating 21 Review ARTICLE to escape. This mechanism prevents the stomach from becoming IRRITABLE BOWEL SYNDROME (IBS) Symptomatic Approach to Gas, Belching and Bloating damaged by excessive dilation.2 IBS is abdominal pain or discomfort associated with altered with OMT Treatment Options Many patients with GERD report increased belching. Transient bowel habits. It is the most commonly diagnosed GI disorder lower esophageal sphincter (LES) relaxation is the major and accounts for about 30% of all GI referrals.7 Criteria for IBS is recurrent abdominal pain at least one day per week in the Carly Gennaro, DO1; Helaine Larsen, DO1 mechanism for both belching and GERD. Recent studies have shown that the number of belches is related to the number of last three months associated with at least two of the following: times someone swallows air. These studies have concluded that 1) association with defecation, 2) change in stool frequency, 1 Good Samaritan Hospital Medical Center, West Islip, NY patients with GERD swallow more air in response to heartburn and 3) change in stool form. Diagnosis should be made using these therefore belch more frequently.3 There is no specific treatment clinical criteria and limited testing. Common symptoms are for belching in GERD patients, so for now, physicians continue to abdominal pain, bloating, alternating diarrhea and constipation, treat GERD with proton pump inhibitors (PPIs) and histamine-2 and pain relief after defecation. Pain can be present anywhere receptor antagonists with the goal of suppressing heartburn and in the abdomen, but the lower abdomen is the most common KEYWORDS: ABSTRACT: Intestinal gas production is a normal physiologic progress. -
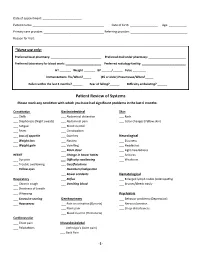
Patient Review of Systems Please Mark Any Condition with Which You Have Had Significant Problems in the Last 6 Months
Date of appointment: ________________________ Patient name: ____________________________________________ Date of birth: _________________ Age: ___________ Primary care provider: _____________________________________ Referring provider: ___________________________________ Reason for Visit: _____________________________________________________________________________________________ *Nurse use only: Preferred local pharmacy: _______________________________ Preferred mail order pharmacy: _______________________ Preferred laboratory for blood work: ______________________ Preferred radiology facility: ___________________________ HT _______ Weight _______ BP ______/______ Pulse ________ Immunizations: Flu/When?_____ (65 or older) Pneumovax/When?_____ Fallen within the last 3 months? ______ Fear of falling?______ Difficulty ambulating? ______ Patient Review of Systems Please mark any condition with which you have had significant problems in the last 6 months: Constitution Gastrointestinal Skin ___ Chills ___ Abdominal distention ___ Rash ___ Diaphoresis (Night sweats) ___ Abdominal pain ___ Color changes (Yellow skin) ___ Fatigue ___ Blood in stool ___ Fever ___ Constipation ___ Loss of appetite ___ Diarrhea Neurological ___ Weight loss ___ Nausea ___ Dizziness ___ Weight gain ___ Vomiting ___ Headaches ___ Black stool ___ Light-headedness HEENT ___ Change in bowel habits ___ Seizures ___ Eye pain ___ Difficulty swallowing ___ Weakness ___ Trouble swallowing ___ Gas/flatulence ___ Yellow eyes ___ Heartburn/indigestion ___ Bowel accidents Hematological -

5223.0210 GASTROINTESTINAL TRACT. Subpart 1. General. the Following Schedule Is for the Evaluation of Permanent Partial Disability of the Gastrointestinal Tract
1 REVISOR 5223.0210 5223.0210 GASTROINTESTINAL TRACT. Subpart 1. General. The following schedule is for the evaluation of permanent partial disability of the gastrointestinal tract. The evaluation must include a thorough history and physical examination. Additional studies, such as radiographic, metabolic, absorptive, endoscopic, and biopsy may be necessary to determine the functioning of these organs. Disability shall not be determined until after completion of all medically accepted diagnostic and therapeutic efforts. The percentages indicated in this schedule are the disability of the whole body for the corresponding class. For evaluative purposes, the digestive tract has been divided into (1) the esophagus, stomach, duodenum, small intestine, and pancreas, (2) the colon and rectum, (3) the anus, and (4) the liver and biliary tract. Subp. 2. Upper digestive tract (esophagus, stomach, duodenum, small intestine, and pancreas). A. Class 1, 2 percent. (1) Symptoms or signs of upper digestive tract disease are present and there is anatomic loss or alteration; continuous treatment is not required; and weight can be maintained at the desirable level; or (2) There are no complications after surgical procedures. B. Class 2, 15 percent. Symptoms and signs of organic upper digestive tract disease are present or there is anatomic loss or alteration; dietary restriction and drugs are required for control of symptoms, signs, or nutritional deficiency; and loss of weight below the desirable weight does not exceed 10 percent. C. Class 3, 35 percent. (1) symptoms and signs of organic upper digestive tract disease are present or there is anatomic loss or alteration; and dietary restrictions and drugs do not completely control symptoms, signs, or nutritional state; or (2) there is 10 to 20 percent loss of weight below the desirable weight and the weight loss is ascribable to a disorder of the upper digestive tract.