Bipolar Disorder: Microdosing Psilocybin to Lessen Depressive Symptoms
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Around the Corner Canadian Equity Research Emerging Companies and Industries to Watch 3 March 2020
Around the Corner Canadian Equity Research Emerging companies and industries to watch 3 March 2020 Tania Gonsalves, CFA | Analyst | Canaccord Genuity Corp. (Canada) | [email protected] | 1.416.996.8346 Scott McFarland | Associate | Canaccord Genuity Corp. (Canada) | [email protected] | 1.416.998.7202 Around the Corner highlights what we believe are some of the most exciting Psychedelic-derived medicines and therapies emergent private companies in Canada, and/or industry themes and trends which are yet to be fully represented in the Mental health miracle or another bad trip? public markets. When most of us think of psychedelic drugs, we think of the 1960s counterculture. We We aim to offer insight into early industry think of anti-establishment, anti-war, anti-capitalist hippies, Woodstock, tie-dye, Lucy in trends, educate investors about private the Sky, peace, love and bell bottom jeans. But before psychedelics became ingrained in companies that are making a mark, and the counterculture, they were found in a lab. The first wave of scientific research on identify companies that may enter the psychedelics took place between 1950-65. Sandoz Pharmaceutics, what is now Novartis public markets in the future. AG (NVS-NYSE), the third largest pharmaceutical company in the world, used to market We do not provide any ratings or price LSD and psilocybin for psychotherapeutic purposes. Psychedelics weren’t born of the targets, nor should any be inferred, for counterculture. They were killed by it. The proliferation of recreational use spurred any uncovered company featured in government intervention and by 1971, psilocybin, LSD, ibogaine, mescaline, peyote, Around the Corner. -

Responding to an Urgent Mental Health Crisis Challenges and Solutions for People Suffering with Treatment-Resistant Depression
Responding to an urgent mental health crisis Challenges and solutions for people suffering with treatment-resistant depression A White Paper from COMPASS Pathways August 2021 Contents Foreword from George Goldsmith ..............................................................................................................03 Introduction ........................................................................................................................................................05 Executive summary . .........................................................................................................................................06 Part I: Treatment-resistant depression - background and challenges .................................................08 o Mental health disorders o Depression: an overview o Major depressive disorder and treatment-resistant depression o Suicide and treatment-resistant depression o Mental health care spending and use of services Part II: Current approaches and limitations for treatment of depression ...........................................15 o A fragmented and inaccessible mental health care system o Treatment approaches for depression o Psychotherapy o Drug therapy o Physical (somatic) therapies o Lack of research and development for new drug treatments Part III: Emerging solutions in treatments for depression ......................................................................24 o Emerging treatment options and the challenges of getting these to patients o Psychedelic therapies: a new frontier -

Psilocybin-Assisted Psychotherapy: Treating Depression and Anxiety with Mushrooms
Dominican Scholar Physician Assistant Studies | Student Department of Physician Assistant Articles Studies 2020 Psilocybin-Assisted Psychotherapy: Treating Depression and Anxiety with Mushrooms Sofia Beck Dominican University of California https://doi.org/10.33015/dominican.edu/2020.PAS.10 Survey: Let us know how this paper benefits you. Recommended Citation Beck, Sofia, "Psilocybin-Assisted Psychotherapy: Treating Depression and Anxiety with Mushrooms" (2020). Physician Assistant Studies | Student Articles. 7. https://doi.org/10.33015/dominican.edu/2020.PAS.10 This Article is brought to you for free and open access by the Department of Physician Assistant Studies at Dominican Scholar. It has been accepted for inclusion in Physician Assistant Studies | Student Articles by an authorized administrator of Dominican Scholar. For more information, please contact [email protected]. ABSTRACT Depression and anxiety are debilitating mental health conditions that affect a large portion of the United States. Current pharmacological treatments for these disorders require daily administration, are associated with a number of side effects, and can be ineffective for some. Emerging evidence in novel treatment options may necessitate a shift toward how we treat these psychiatric disorders. Studies involving the psychedelic serotonin agonist, psilocybin, are currently experiencing a resurgence as an alternative for patients who are unresponsive to traditional treatments. Clinical trials using psilocybin in combination with psychotherapy have demonstrated sustained reductions in depression and/or anxiety symptoms. When used in medical settings, it has shown to be safe, with few side effects and no risk of dependence. However, this psychedelic compound faces many stigmas and these results have yet to be compared to current treatments or in larger populations. -

Can Magic Mushrooms Heal Us? - the New York Times
3/22/2021 Opinion | Can Magic Mushrooms Heal Us? - The New York Times Can Magic Mushrooms Heal Us? A very promising mental health experiment is taking shape in Oregon. By Ezra Klein Opinion Columnist March 18, 2021 Gov. Kate Brown of Oregon announced the members of the state’s newly formed Psilocybin Advisory Board this week. Why does Oregon need an official board to offer advice about the active ingredient in magic mushrooms, you ask? Because Oregon is about to become the first state in the country to try to build a support infrastructure through which psychedelic mushrooms can be woven into everyday life. This framework is different from what we’ve seen before: not legalization, not medicalization, but therapeutic use, in licensed facilities, under the guidance of professionals trained to guide psychedelic experiences. Whoa. “Like many, I was initially skeptical when I first heard of Measure 109,” Brown said in a statement. “But if we can help people suffering from PTSD, depression, trauma and addiction — including veterans, cancer patients, and others — supervised psilocybin therapy is a treatment worthy of further consideration.” [Listen to “The Ezra Klein Show,” a podcast about ideas that matter.] Measure 109, the Oregon Psilocybin Services Act, approved as a ballot measure in November, is the brainchild of Tom and Sheri Eckert, who shared a therapy practice in Portland. In 2015, the Eckerts read an article by Michael Pollan in The New Yorker titled “The Trip Treatment.” The article described the emerging research around using psychedelics as a therapeutic tool and unearthed the largely forgotten pre-Timothy Leary period in which psychedelics were widely used by psychiatrists. -

Experience of Music Used with Psychedelic Therapy: a Rapid Review and Implications
Downloaded from https://academic.oup.com/jmt/advance-article-abstract/doi/10.1093/jmt/thaa006/5813582 by University of Birmingham user on 10 April 2020 Journal of Music Therapy, XX(XX), 2020, 1–33 doi:10.1093/jmt/thaa006 © The Author(s) 2020. Published by Oxford University Press on behalf of American Music Therapy Association. All rights reserved. For permissions, please e-mail: [email protected] Experience of Music Used With Psychedelic Therapy: A Rapid Review and Implications Clare O’Callaghan, AM, PhD, MMus, BMus, BSW, RMT Caritas Christi Hospice & Department of Psychosocial Cancer Care Research, St Vincent’s Hospital, Melbourne, Australia Department of Medicine, St Vincent’s Hospital, and Melbourne Conservatorium of Music, The University of Melbourne, Melbourne, Australia Daniel J. Hubik, MBBS, M. Psychiatry, FRANZCP Department of Psychosocial Cancer Care Research, St Vincent’s Hospital, Melbourne, Australia Justin Dwyer, MBBS Psychiatry, FRANZCP Department of Psychosocial Cancer Care Research, St Vincent’s Hospital, Melbourne, Australia Martin Williams, PhD Monash Institute of Pharmaceutical Sciences, Monash University, Melbourne, Australia PRISM Inc., Melbourne, Australia Margaret Ross, PsyD, BSocSci, MAPS, FCCLP Caritas Christi Hospice & Department of Psychosocial Cancer Care Research, St Vincent’s Hospital, Melbourne, Australia Bonny Method of Guided Imagery and Music emerged following dis- continuation of psychedelic therapy research in the early 1970s, but psychedelic therapy research has since revived. Music remains a vital component. This study examined participants’ experiences of music in psychedelic therapy research. A rapid review of qualitative and This study was conducted while the authors were clinically working at St Vincent’s Hospital Melbourne. Address correspondence concerning this article to Clare O’Callaghan, PhD, RMT, Caritas Christi Hospice, St Vincent’s Hospital, 41 Victoria Parade, Fitzroy, Australia, 3065. -
Legalising Access to Psilocybin to End the Agony of Cluster Headaches*
ORGANISATION FOR THE PREVENTION OF INTENSE SUFFERING WWW.PREVENTSUFFERING.ORG POLICY PAPER LEGALISING ACCESS TO PSILOCYBIN TO END THE AGONY OF CLUSTER HEADACHES* *SUICIDE HEADACHES/HORTON’S NEURALGIA An ethical and evidence-based approach to treating one of the most excruciating conditions known to medicine. OPISNOVEMBER 2020 Legalising Access to Psilocybin to End the Agony of Cluster Headaches An ethical and evidence-based approach to treating one of the most excruciating conditions known to medicine CONTENTS Executive summary 2 Cluster headaches: a public health emergency 3 Patients’ descriptions of their pain 5 Standard treatments: benefits and shortcomings 6 Efectiveness of psilocybin and related chemicals 7 Patient testimonials of efcacy 10 Patients’ experiences represent powerful, essential evidence 14 Safety of psilocybin and other indoleamines 15 Cost 16 Legal status 16 Consequences of current drug policies for cluster headache patients 17 Ethical considerations 18 Human rights perspective 19 Policy options and recommendations 20 Possible concerns and responses 22 Co-signatories 23 EXECUTIVE SUMMARY Approximately 8 million people worldwide are aficted with possibly the most excruciating condition known to medicine: cluster headaches. Patients endure immense sufering, and many commit suicide to escape the pain. Current medical options are inadequate. Fortunately there is now clear evidence that psilocybin and chemically related substances are efective for many patients in preventing and aborting attacks. However, their legal status in most countries makes it difcult for patients to access them. Governments can dramatically improve the quality of life for many of their citizens, with little or no additional cost or risk, by removing the legal barriers to cluster headache patients accessing psilocybin and related compounds for therapeutic purposes. -

Psychedelics and Mania Review Paper
medRxiv preprint doi: https://doi.org/10.1101/2021.04.02.21254838; this version posted April 7, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. It is made available under a CC-BY-NC-ND 4.0 International license . Evaluating the Risk of Psilocybin for the Treatment of Bipolar Depression: A Systematic Review of Published Case Studies David E. Garda, Mollie M. Pleetb, c, Ellen R. Bradleyb, c, Andrew Pennb, Matthew L. Gallensteina, Lauren S. Rileya, Meghan DellaCrossed, Emily Garfinklee, Erin E. Michalakf, Joshua D. Woolleyb, c aSan Francisco State University, San Francisco, CA USA bUniversity of California San Francisco, San Francisco, CA USA cSan Francisco Veteran's Affairs Medical Center, San Francisco, CA USA dThe Wright Institute, Berkeley, CA USA ePalo Alto University-Pacific Graduate School of Psychology, Palo Alto, CA USA fUniversity of British Columbia, Vancouver, BC Canada Corresponding author: David E. Gard, Ph.D. Department of Psychology, San Francisco State University 1600 Holloway Ave San Francisco, California 94132 USA [email protected] Sources of direct funding, support, or sponsorship ● Dr. Woolley is funded in part via VA CSR&D 1IK4CX002090-01. Grant title: Quantifying and Treating Social Deficits in Veterans with Mental Illness: a Five Year Plan. Role of the sponsor ● Not applicable Potential conflicts of interest ● Dr. Woolley is a paid consultant for Psilo Scientific Ltd. and Silo Pharma. Abstract: 250 words Text: 4998 words Number of Figures: 1 Number of Tables: 2 NOTE: This preprint reports new research that has not been certified by peer review and should not be used to guide clinical practice. -

STATE of HAWAII Testimony COMMENTING on HB2567
DAVID Y. IGE BRUCE S. ANDERSON, PHD GOVERNOR OF HAWAII DIRECTOR OF HEALTH STATE OF HAWAII DEPARTMENT OF HEALTH P. O. Box 3378 Honolulu, HI 96801-3378 [email protected] Testimony COMMENTING on HB2567 RELATING TO PSILOCYBIN. REP. JOHN M. MIZUNO, CHAIR HOUSE COMMITTEE ON HEALTH Hearing Date: January 30, 2020 Room Number: 329 1 Fiscal Implications: $50,000 appropriation is recommended for meeting facilitation and 2 research services. 3 Department Testimony: The Department of Health (DOH) takes no position on the merits of 4 medicinal psilocybin. 5 However, establishing the Working Group pursuant to Session Law subjects it to chapter 92 6 “sunshine” or “open meetings” requirements that increase administrative burden but which to not 7 add commensurate value to the public – no public assets are at stake and there is no binding 8 public policy impacts. 9 The department respectfully recommends exempting the Working Group from chapter 92, or 10 preferably establishing it through Concurrent Resolution. 11 If Session Law is the preferred method, DOH recommends a modest appropriation for meeting 12 facilitation and basic research services. Since there is no existing academic or professional 13 foundation for medicinal psilocybin the Working Group will need research support to synthesize 14 the multidisciplinary elements for this novel public policy topic. 15 Thank you for the opportunity to testify. 16 House Committee on Health Clarity Project Strongly Supports: HB2567 Dear Chair Mizuno, Vice Chair Kobayashi, and Members of the Committee, My name is Helen Cho, and I am here today representing the Clarity Project, a citizen’s initiative that aims to expand patient access to include psilocybin-assisted therapy modalities in Hawaii. -

The Therapeutic Potential of Psilocybin
molecules Review The Therapeutic Potential of Psilocybin Henry Lowe 1,2,3,4, Ngeh Toyang 2,3 , Blair Steele 1,*, Henkel Valentine 1, Justin Grant 1,5, Amza Ali 1,5, Wilfred Ngwa 6 and Lorenzo Gordon 7 1 Biotech R & D Institute, University of the West Indies, Mona 99999, Jamaica; [email protected] (H.L.); [email protected] (H.V.); [email protected] (J.G.); [email protected] (A.A.) 2 Vilotos Pharmaceuticals Inc., Baltimore, MD 21202, USA; ngeh.toyang@flavocure.com 3 Flavocure Biotech Inc., Baltimore, MD 21202, USA 4 Institute of Human Virology (IHV), University of Maryland School of Medicine, Baltimore, MD 21202, USA 5 The Psyence Group, Toronto, ON M5J 2J1, Canada 6 Brigham and Women’s Hospital, Dana-Farber Cancer Institute, Harvard Medical School, Boston, MA 02215, USA; [email protected] 7 Caribbean School of Medical Sciences, Kingston 99999, Jamaica; [email protected] * Correspondence: [email protected]; Tel.: +876-926-8502 Abstract: The psychedelic effects of some plants and fungi have been known and deliberately ex- ploited by humans for thousands of years. Fungi, particularly mushrooms, are the principal source of naturally occurring psychedelics. The mushroom extract, psilocybin has historically been used as a psychedelic agent for religious and spiritual ceremonies, as well as a therapeutic option for neuropsychiatric conditions. Psychedelic use was largely associated with the “hippie” counterculture movement, which, in turn, resulted in a growing, and still lingering, negative stigmatization for psychedelics. As a result, in 1970, the U.S. government rescheduled psychedelics as Schedule 1 drugs, ultimately ending scientific research on psychedelics. -
Yale Manual for Psilocybin-Assisted Therapy of Depression
Yale Manual for Psilocybin-Assisted Therapy of Depression Version 4.2 Revised August 2019 Manual Co-Authors Jeffrey Guss, MD RoBert Krause, DNP APRN-BC Jordan Sloshower, MD, MSc Ryan Wallace, MD, MPH 2 Acknowledgements We express deep gratitude to Both the early and contemporary pioneers of this work—the scientists, authors, practitioners, guides, research volunteers, and organizations whose work with entheogens kept their possibilities alive - and who campaigned to revive and extend the study of entheogens for the benefit of others. Without these pioneers, this study and the majority of research related to the transformative and therapeutic benefits of entheogens would not exist. Thanks to funders: Yale University Department of Psychiatry Carey and Claudia TurnBull Heffter Research Institute Usona Research Institute Additional thanks: Dr. Jeffrey Guss, MD of NYU for his role as mentor and guide Members and faculty of the Yale Psychedelic Science Group 3 TABLE OF CONTENTS 1.0 INTRODUCTION 1.1 Goals of this Manual 1.2 Essential Elements of the Therapeutic Method 1.2a General Elements of Psychedelic-Assisted Therapy 1.2b Theoretical Orientations of Psilocybin-Assisted Therapy for Depression 1.2c Why utilize Acceptance and Commitment Therapy in Psilocybin- assisted therapy for Major Depressive Disorder? 2.0 THERAPIST FOUNDATION 2.1 Essential Therapist Background 2.2 Specialized Therapist Skills 3.0 SET and SETTING: THERAPIST PREPARATION 3.1 Set: The participant’s inner world 3.2 Preparing the Physical Setting 3.3 Preparing Social Support -

Clinical Trials of Psilocybin and Ecstasy As Treatments for Depression And
Feature THE RISE OF PSYCHEDELIC PSYCHIATRY Clinical trials of psilocybin and ecstasy as treatments for depression and post-traumatic stress disorder are starting to give results, but approvals will be challenging. By Paul Tullis n a sunny day in London in 2015, Kirk lovely, and especially Robin,” Rutter recalls. bejewelled structures. Then his mind went to Rutter rode the Tube to Hammer- Carhart-Harris led him to a room with a mag- work on his grief. smith Hospital in hopes of finally netic resonance imaging (MRI) machine, so The Imperial study was one of a spate of putting an end to his depression. researchers could acquire a baseline of his clinical trials launched over the past few years Rutter had lived with the condi- brain activity. Then he showed Rutter where using illicit psychedelic drugs such as psilo- tion off and on for years, but the he would spend his time while on the drug. cybin, lysergic acid diethylamide (LSD) and burden had grown since the death Carhart-Harris asked him to lie down and played MDMA (3,4-methylenedioxymethampheta- of his mother in 2011, followed by a him some of the music that would accompany mine, also known as molly or ecstasy) to treat Orelationship break-up and a car accident the the session. He explained that he would have mental-health disorders, generally with the year after. It felt as if his brain was stuck on on hand a drug that could neutralize the hallu- close guidance of a psychiatrist or psycho- what he describes as “an automatic circuit”, cinogen, if necessary. -
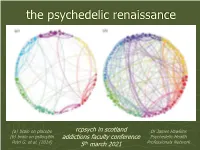
Psychedelics, Trauma & Addiction
the psychedelic renaissance (a) brain on placebo rcpsych in scotland Dr James Hawkins (b) brain on psilocybin addictions faculty conference Psychedelic Health Petri G. et al. (2014) 5th march 2021 Professionals Network sequence of talks this morning jake hawthorn introduction to psychedelics mdma-assisted psychotherapy ben sessa for alcohol use disorder broader research evidence, james hawkins mechanisms and education for addiction treatments a quick ’aerial view’ ➢ broader overall context ➢ what evidence supports the use of psychedelics in addiction treatment? ➢ how do psychedelic treatments work? ➢ education, training & the psychedelic health professionals network broader overall context ❖ who? ❖ why? ❖ what? ❖ how? ❖ where? who takes psychedelics? extrapolating mdma psilocybin psychedelics from dutch & us figures 3% annual 9.7% lifetime 17.4% lifetime scotland 5.5 m 165,000 533,500 957,000 uk 6 6 6 53.9 m 1.6 x 10 5.2 x 10 9.4 x 10 Van Laar MW, Van Gestel B, Cruts AAN, et al. (2019) Nationale Drug Monitor. Jaarbericht 2018. Utrecht, The Netherlands: Trimbos Instituut. Yockey, A. & King, K. (2021). “Use of psilocybin (“mushrooms”) among US adults: 2015–2018” J Psychedelic Studies. Jan 21. SAMHSA. (2020). ”17.4% of US adults have used a psychedelic." why do people take psychedelics? what are psychedelics? ‘psychedelic’ means ’mind revealing’ … a term introduced by British psychiatrist, Humphrey Osmond, in the 1950’s ❖ classic psychedelics (5-HT2A receptor agonists) ▪ psilocybin, LSD, DMT/ayahuasca, mescaline ❖ entactogens/empathogens ▪ MDMA, MDA, MMDA, 2C-series, etc ❖ dissociatives ▪ ketamine, nitrous oxide, salvia divinorum, PCP ❖ unique substances ▪ ibogaine, mad honey, etc classification by Kim Kuypers, researcher at Maastricht University, Netherlands how are psychedelics taken? different methods of ❖ orally ingestion produce different outcomes: ❖ inhaled ❖ nasally bioavailability ❖ sublingually predictability ❖ intramuscularly speed of onset ❖ intravenously duration of action ❖ rectally, etc side effects risk profile where: set Kettner, H.