[Lepirudin (Rdna) for Injection] Rx Only DESCRIPTION REFLUDAN
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Evolving Role of Direct Thrombin Inhibitors in Acute Coronary
View metadata, citation and similar papers at core.ac.uk brought to you by CORE Journal of the American College of Cardiology providedVol. by 41, Elsevier No. 4 - SupplPublisher S Connector © 2003 by the American College of Cardiology Foundation ISSN 0735-1097/03/$30.00 Published by Elsevier Science Inc. PII S0735-1097(02)02687-6 The Evolving Role of Direct Thrombin Inhibitors in Acute Coronary Syndromes John Eikelboom, MBBS, MSC, FRACP, FRCPA,* Harvey White, MB, CHB, DSC, FRACP, FACC,† Salim Yusuf, MBBS, DPHIL, FRCP (UK), FRCPC, FACC‡ Perth, Australia; Auckland, New Zealand; and Hamilton, Ontario, Canada The central role of thrombin in the initiation and propagation of intravascular thrombus provides a strong rationale for direct thrombin inhibitors in acute coronary syndromes (ACS). Direct thrombin inhibitors are theoretically likely to be more effective than indirect thrombin inhibitors, such as unfractionated heparin or low-molecular-weight heparin, because the heparins block only circulating thrombin, whereas direct thrombin inhibitors block both circulating and clot-bound thrombin. Several initial phase 3 trials did not demonstrate a convincing benefit of direct thrombin inhibitors over unfractionated heparin. However, the Direct Thrombin Inhibitor Trialists’ Collaboration meta-analysis confirms the superiority of direct thrombin inhibitors, particularly hirudin and bivalirudin, over unfractionated heparin for the prevention of death or myocardial infarction (MI) during treatment in patients with ACS, primarily due to a reduction in MI (odds ratio, 0.80; 95% confidence interval, 0.70 to 0.91) with little impact on death. The absolute risk reduction in the composite of death or MI at the end of treatment (0.8%) was similar at 30 days (0.7%), indicating no loss of benefit after cessation of therapy. -

201370Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 201370Orig1s000 MEDICAL REVIEW(S) M E M O R A N D U M DEPARTMENT OF HEALTH AND HUMAN SERVICES PUBLIC HEALTH SERVICE FOOD AND DRUG ADMINISTRATION CENTER FOR DRUG EVALUATION AND RESEARCH Date: July 8, 2011 From: Kathy M. Robie-Suh, M.D., Ph.D. Medical Team Leader Division of Hematology Products Subject: NDA 201370, resubmission April 11, 2011 Heparin Sodium Injection (heparin sodium, USP) Sponsor: Pfizer, Inc. 235 East 42nd Street New York, NY 10017-5755 To: NDA 201370 This is the second review cycle for this 505(b)(2) application for a new Heparin Sodium Injection product derived from porcine intestine. The presentations include several containing benzyl alcohol as a preservative and one preservative-free presentation. The first cycle review of the NDA found the application acceptable from a clinical viewpoint. However, manufacturing facilities inspection identified deficiencies that precluded approval and a Complete Response (CR) letter was issued on April 7, 2011. Labeling review was not completed at that time. In the current resubmission the sponsor has responded to the identified deficiencies deleting the two heparin supplier sites where deficiencies were found. The Amended Cross-Discipline Team Leader Review by Dr. Ali Al-Hakim (6/28/2011) comments that Office of Compliance has updated its recommendation in the Establishment Evaluation System and issued “ACCEPTABLE” overall recommendation for this NDA on June 27, 2011 and therefore the NDA is recommended for approval. No new clinical information is included in the resubmission. Clinical review of the original application and the resubmission was conducted by Dr. -

Pharmacoepidemiological.Study.Protocol.. ER1379468. A.Retrospective.Cohort.Study.To.Investigate.The.Initiation. And.Persistence.Of.Dual.Antiplatelet.Treatment.After
Pharmacoepidemiological.study.protocol.ER1379468. % . % % % % % Pharmacoepidemiological.study.protocol.. ER1379468. A.retrospective.cohort.study.to.investigate.the.initiation. and.persistence.of.dual.antiplatelet.treatment.after.. acute.coronary.syndrome.in.a.Finnish.setting.–.THALIA. % Author:(( ( ( Tuire%Prami( Protocol(number:(( %% ER1359468,%ME5CV51306( Sponsor:(( ( ( AstraZeneca%Nordic%Baltic% Protocol(version:(( ( 2.0( Protocol(date:(( ( ( 03%Jul%2014% ( . EPID%Research%Oy%. CONFIDENTIAL. % Pharmacoepidemiological.study.protocol.ER1379468... Version.2.0. 03.Jul.2014. Study Information Title% A% retrospective% cohort% study% to% investigate% the% initiation% and% persistence% of% dual% antiplatelet%treatment%after%acute%coronary%syndrome%in%a%Finnish%setting%–%THALIA% Protocol%version% ER1359468% identifier% ME5CV51306% EU%PAS%register% ENCEPP/SDPP/6161% number% Active%substance% ticagrelor%(ATC%B01AC24),%clopidogrel%(B01AC04),%prasugrel%(B01AC22)% Medicinal%product% Brilique,% Plavix,% Clopidogrel% accord,% Clopidogrel% actavis,% Clopidogrel% krka,% Clopidogrel% mylan,%Clopidogrel%orion,%Clopidogrel%teva%pharma,%Cloriocard,%Efient% Product%reference% N/A% Procedure%number% N/A% Marketing% AstraZeneca%Nordic%Baltic:%Brilique%(ticagrelor)% authorization% holder% financing%the%study% Joint%PASS% No% Research%question% To%describe%initiation%and%persistence%of%dual%antiplatelet%treatment%in%invasively%or%non5 and%objectives% invasively%treated%patients%hospitalized%for%acute%coronary%syndrome%% Country%of%study% Finland% Author% Tuire%Prami% -
Best Evidence for Antithrombotic Agent Reversal in Bleeding
3/16/2021 1 JAMES H. PAXTON, MD • DIRECTOR OF CLINICAL RESEARCH • DETROIT RECEIVING HOSPITAL (DRH), DEPARTMENT OF EMERGENCY MEDICINE, WAYNE STATE UNIVERSITY • ATTENDING PHYSICIAN • SINAI-GRACE HOSPITAL (SGH) • DETROIT RECEIVING HOSPITAL (DRH) 2 1 3/16/2021 DISCLOSURES • FUNDED RESEARCH SPONSORED BY: TELEFLEX INC, 410 MEDICAL, HOSPI CORP. 3 OBJECTIVES •AT THE CONCLUSION OF THIS LECTURE, THE LEARNER WILL: • RECOGNIZE COMMON ANTITHROMBOTIC MEDICATIONS ASSOCIATED WITH BLEEDING EMERGENCIES • BE ABLE TO EXPLAIN THE MECHANISMS OF ACTION FOR COMMON ANTITHROMBOTIC MEDICATIONS • UNDERSTAND THE EVIDENCE FOR RAPID REVERSAL OF ANTITHROMBOTIC MEDICATIONS, INCLUDING CONTROVERSIES AND BEST PRACTICES HAVE FEWER NIGHTMARES ABOUT SCENES LIKE THE ONE ON THE NEXT SLIDE? 4 2 3/16/2021 BLEEDING IS BAD 5 WHEN TO REVERSE? • WHEN RISK OF BLEEDING OUTWEIGHS RISK OF REVERSAL: • INTRACRANIAL HEMORRHAGE (ICH) • OTHER CNS HEMATOMA (E.G., INTRAOCULAR, SPINAL) • EXSANGUINATING GASTROINTESTINAL (GI) BLEED • UNCONTROLLED RETROPERITONEAL BLEED • HEMORRHAGE INTO EXTREMITY WITH COMPARTMENT SYNDROME • CONSIDER IN POSTERIOR EPISTAXIS, HEMOTHORAX, PERICARDIAL TAMPONADE 6 3 3/16/2021 ANTITHROMBOTIC AGENTS •ANTI-PLATELET DRUGS •ANTI-COAGULANTS •FIBRINOLYTICS 7 THROMBOGENESIS • Primary component in arterial thrombosis (“white clot”) • Target for antiplatelet drugs • Primary component in venous thrombosis (“red clot”) • Aggregated platelets + • Target for anticoagulants fibrin mesh • Target for fibrinolytics 8 4 3/16/2021 PLATELET AGGREGATION Antiplatelet Drugs Mechanism Aspirin* -

List Item Refludan : EPAR
SCIENTIFIC DISCUSSION This module reflects the initial scientific discussion and scientific discussion on procedures which have been finalised before 1 August 2003. For scientific information on procedures after this date please refer to module 8B. I Introduction Refludan contains Lepirudin ([Leu1-Thr2]-63-desulfohirudin) as the active substance. Lepirudin is a hirudin analogue produced in yeast cells transfected with an expression vector containing the hirudin gene. Refludan is presented as a powder to be reconstituted with water for injection or with isotonic saline for intravenous injection or infusion. It is supplied in one strength with a standardised content of 50 mg lepirudin per vial. The specific activity of lepirudin is approximately 16,000 (Antithrombin Units) ATU per mg, where one ATU is the amount of hirudin that neutralises one unit of the WHO preparation of thrombin (89/588). Lepirudin is a specific direct inhibitor of free and clot-bound thrombin and the proposed therapeutic indication is anticoagulation in adult patients with heparin-associated thrombocytopenia (HAT) type II and thromboembolic disease mandating parenteral antithrombotic therapy. HAT type II is a complication of heparin therapy, with a probable incidence of the order of 1% of heparin-treated patients. The disorder is characterised by, sometimes profouauthorisednd, thrombocytopenia and a high propensity for venous and arterial thromboembolic complications occurring during continued heparin treatment. Mortality and amputation rates of 20-30% and 10-20%, respectively, are cited in the more recent literature reviews. The chief underlying pathogenic mechanism seems to be a formation of antibodies directed mainly against a complex of heparin and Platelet Factor 4. -

Release of Alpha 2-Plasmin Inhibitor from Plasma Fibrin Clots by Activated Coagulation Factor XIII
Release of alpha 2-plasmin inhibitor from plasma fibrin clots by activated coagulation factor XIII. Its effect on fibrinolysis. J Mimuro, … , S Kimura, N Aoki J Clin Invest. 1986;77(3):1006-1013. https://doi.org/10.1172/JCI112352. Research Article When blood coagulation takes place in the presence of calcium ions, alpha 2-plasmin inhibitor (alpha 2PI) is cross-linked to fibrin by activated coagulation Factor XIII (XIIIa) and thereby contributes to the resistance of fibrin to fibrinolysis. It was previously shown that the cross-linking reaction is a reversible one, since the alpha 2PI-fibrinogen cross-linked complex could be dissociated. In the present study we have shown that the alpha 2PI-fibrin cross-linking reaction is also a reversible reaction and alpha 2PI which had been cross-linked to fibrin can be released from fibrin by disrupting the equilibrium, resulting in a decrease of its resistance to fibrinolysis. When the fibrin clot formed from normal plasma in the presence of calcium ions was suspended in alpha 2PI-deficient plasma of buffered saline, alpha 2PI was gradually released from fibrin on incubation. When alpha 2PI was present in the suspending milieu, the release was decreased inversely to the concentrations of alpha 2PI in the suspending milieu. The release was accelerated by supplementing XIIIa or the presence of a high concentration of the NH2-terminal 12-residue peptide of alpha 2PI (N-peptide) which is cross-linked to fibrin in exchange for the release of alpha 2PI. When the release of alpha 2PI from fibrin was accelerated by XIIIa or N-peptide, the fibrin became less resistant to the fibrinolytic process, resulting in an […] Find the latest version: https://jci.me/112352/pdf Release of a2-Plasmin Inhibitor from Plasma Fibrin Clots by Activated Coagulation Factor XIII Its Effect on Fibrinolysis Jun Mimuro, Shigeru Kimura, and Nobuo Aoki Institute ofHematology and Department ofMedicine, Jichi Medical School, Tochigi-Ken 329-04, Japan Abstract glutaminase, activated blood coagulation Factor XIII (XIIIa) (2-4). -

Melagatran Und Ecarinzeit.Pdf
Wednesday , August 06, 2003 1 Effects of Lepirudin, Argatroban and Melagatran and Additional Influence of Phenprocoumon on Ecarin Clotting Time Tivadar Fenyvesi* M.D., Ingrid Jörg* M.D., Christel Weiss + Ph.D., Job Harenberg* M.D. Key words: direct thrombin inhibitors, ecarin clotti ng time, oral anticoagulants, enhancing effects *IV. Department of Medicine +Institute for Biometrics and Medical Statistics University Hospital Mannheim Theodor Kutzer Ufer 1 - 3 68167 Mannheim Germany *Corresponding author Phone: +49 -621 -383 -3378 E-ma il: tivadar.fenyvesi @med1.ma.uni -heidelberg.de Version 06.08.03 for Thromb Res Review Copy Elsevier 1 of 22 Wednesday , August 06, 2003 2 Abstract Introduction: Direct thrombin inhibitors (DTI) prolong the ecarin clotting time (ECT). Oral anticoagulants (OA) decrease prothrombin levels and thus interacts with actions of DTIs on the ECT method during concomitant therapy. Materials and methods: Actions of lepirudin, argatroban, and melagatran on ECT were investigated in normal plasma (NP) and in plasma of patients (n = 23 each) on stable therapy with phenprocoumon (OACP). Individual line characteristics were tested statistically. Results: Control ECT in OACP was prolonged compared to NP (50.1±0.9 vs. 45.7±0.8 sec; p < 0.001). Lepirudin prolonged the ECT linearly. Argatroban and melagatran delivered biphasic dose-response curves. OA showed additive effects on the ECT of lepirudin but not of argatroban and melagatran. Both in NP and OACP the first and second slopes of melagatran were steeper compared to argatroban (primary analysis; p<0.001). When using the same drug, slopes in OACP were steeper than in NP (secondary analysis; p<0.001). -

Refludan, INN-Lepirudin
ANNEXE I autorisé RÉSUMÉ DES CARACTÉRISTIQUES DU PRODUIT plus n'est médicament Ce 1 1. DENOMINATION DU MEDICAMENT Refludan, 20 mg, poudre pour solution injectable ou pour perfusion 2. COMPOSITION QUALITATIVE ET QUANTITATIVE Chaque flacon contient 20 mg de lépirudine. (La lépirudine est un produit ADN recombinant dérivé de cellules de levure) Pour une liste complète des excipients, voir rubrique 6.1. 3. FORME PHARMACEUTIQUE Poudre pour solution injectable ou pour perfusion. Poudre lyophilisée blanche à presque blanche. 4. DONNEES CLINIQUES 4.1 Indications thérapeutiques autorisé Inhibition de la coagulation chez des patients adultes atteints d'une thrombopénie induite par l'héparine (TIH) de type II et de maladie thrombo-embolique nécessitant un traitement antithrombotique par voie parentérale. plus Le diagnostic devrait être confirmé par le test d'activation plaquettaire induite par l'héparine (HIPAA = Heparin Induced Platelet Activation Assay) ou un test équivalent. n'est 4.2 Posologie et mode d’administration Le traitement par Refludan devrait être débuté sous le contrôle d'un médecin ayant une expérience des troubles de l’hémostase. Posologie initiale Inhibition de la coagulation chezmédicament des patients adultes atteints d'une TIH de type II et de maladie thrombo-embolique : Ce 0,4 mg/kg de poids corporel en bolus intraveineux, suivi de 0,15 mg/kg de poids corporel/heure en perfusion intraveineuse continue pendant 2 à 10 jours, voire plus si l'état clinique du patient le nécessite. La posologie dépend du poids corporel du patient jusqu'à 110 kg. Chez les patients pesant plus de 110 kg, la posologie ne doit pas dépasser celle calculée pour les patients pesant 110 kg (voir aussi tableaux 2 et 3 ci-après). -

Neuroradiology Fine Needle Spinal Procedures and Anticoagulation: Fine Needle Spinal Procedure: 20 Gauge Needle Or Smaller
Neuroradiology Fine Needle Spinal Procedures and Anticoagulation: Fine needle spinal procedure: 20 gauge needle or smaller. Typically 20 or 22 gauge is used. Medication Recommendation Aspirin & NSAIDS -Does NOT need to be stopped. Warfarin -Stop 5 days prior. -Check INR: INR ≤ 1.2 is normal. Proceed. *INR of 1.3 or 1.4 requires 24 hrs of post procedure monitoring. INR of ≥1.5LP not done. Thrombolytics (tPA) Unsafe. Should not be used pre or post procedure. Time frame uncertain. Heparin SQ (DVT prophylaxis) -Check platelets if on heparin ≥5 days. 5000 units SQ BID -No contraindication or delay if standard dosing of 5000 units SQ BID. -If given ≥ TID or > 5,000 units/dose or > 10,000 units /day: follow heparin IV protocol. Heparin IV -Wait 2-4 hours after last dose of IV heparin. -Document normal PTT. -Check platelets if on heparin ≥5 days. -Wait at least 1 hr after procedure to restart heparin drip. LMWH (Enoxaparin) prophylaxis -Wait 12 hrs after last dose to perform procedure. 30 mg SQ BID or -Wait 24 hrs after LP to restart med. 40 mg SQ daily LMHW (Enoxaparin) treatment -Wait 24 hrs after last dose to perform procedure. 1-1.5 mg/kg/day -Wait 24 hrs to restart med. Fondaparinux (Arixtra) -Withhold based on Cr. Cr Cl >50 wait 2-3 days; Cr Cl < 50 wait 3-5 days Clopidogrel (Plavix) Stop 5 days prior. Ticlopidine (Ticlid) Stop 14 days prior. Abciximab (ReoPro) (IIb/IIIa) Stop 2 days prior. Eptifibatide (Integrilin) (IIb/IIIa) Stop 4-8 HOURS prior. Tirofiban (Aggrastat) (IIb/IIIa) Stop 8 HOURS prior. -

Cleveland Clinic Anticoagulation Management Program (C-Camp)
CLEVELAND CLINIC ANTICOAGULATION MANAGEMENT PROGRAM (C-CAMP) 1 Table of Contents I. EXECUTIVE SUMMARY ......................................................................................................................................... 6 II. VENOUS THROMBOEMBOLISM RISK ASSESSMENT AND PROPHYLAXIS ............................................. 9 III. RECOMMENDED PROPHYLAXIS OPTIONS FOR THE PREVENTION OF VENOUS THROMBOEMBOLISM. ........................................................................................................................................ 10 IIIA. RECOMMENDED PROPHYLAXIS OPTIONS FOR THE PREVENTION OF VENOUS THROMBOEMBOLISM BASED ON RISK FACTOR ASSESSMENT ............................................................. 12 A) UNFRACTIONATED HEPARIN (UFH) ................................................................................................................... 14 B) LOW MOLECULAR WEIGHT HEPARIN (LMWH) ENOXAPARIN (LOVENOX®) .............................................. 14 C) FONDAPARINUX/ (ARIXTRA®) …………………………………………………………………………..……16 D) RIVAROXABAN (XARELTO®) .......................................................................................................................... 16 E) DESIRUDIN (IPRIVASK®)………………………………………………………………………………..…….17 F) WARFARIN/COUMADIN®) ............................................................................................................................... 16 G) ASPIRIN……………………………………………………………………………………………………..……18 H) INTERMITTENT PNEUMATIC COMPRESSION DEVICES ..................................................................................... -
Neuraxial Or Nerve Procedures
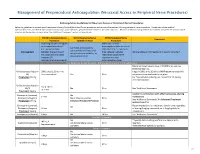
Management of Periprocedural Anticoagulation (Neuraxial Access or Peripheral Nerve Procedures) Anticoagulation Guidelines for Neuraxial Access or Peripheral Nerve Procedures Below are guidelines to prevent spinal hematoma following Epidural/Intrathecal/Spinal procedures and perineural hematoma following peripheral nerve procedures. Procedures include epidural injections/infusions, intrathecal injections/infusions/pumps, spinal injections, peripheral nerve catheters, and plexus infusions. Decisions to deviate from guideline recommendations given the specific clinical situation are the decision of the provider. See ‘Additional Comments’ section for more details. PRIOR to Neuraxial/Nerve WHILE Neuraxial/Nerve AFTER Neuraxial/Nerve Comments Procedure Catheter in Place Procedure How long should I hold prior When can I restart to neuraxial procedure? anticoagulants after neuraxial Can I give anticoagulants (i.e., minimum time procedures? (i.e., minimum concurrently with neuraxial, Anticoagulant between the last dose of time between catheter What additional information do I need to consider? peripheral nerve catheter, or anticoagulant and spinal removal or spinal/nerve plexus placement? injection OR injection and next neuraxial/nerve placement) anticoagulation dose) Low-Molecular Weight Heparins, Unfractionated Heparin, and Fondaparinux Maximum total heparin dose of 10,000 units per day (5000 SQ Q12 hrs) Unfractionated Heparin 5000 units Q 12 hrs – no Heparin 5000 units SQ 8 hrs is NOT recommended with SQ time restrictions Yes 2 hrs concurrent -
The Efficacy and Safety of Hirudin Plus Aspirin Versus Warfarin in the Secondary Prevention of Cardioembolic Stroke Due to Nonva
Int. J. Med. Sci. 2021, Vol. 18 1167 Ivyspring International Publisher International Journal of Medical Sciences 2021; 18(5): 1167-1178. doi: 10.7150/ijms.52752 Research Paper The efficacy and safety of Hirudin plus Aspirin versus Warfarin in the secondary prevention of Cardioembolic Stroke due to Nonvalvular Atrial Fibrillation: A multicenter prospective cohort study Chang-geng Song#, Li-jie Bi#, Jing-jing Zhao, Xuan Wang, Wen Li, Fang Yang, Wen Jiang Department of Neurology, Xijing Hospital, Fourth Military Medical University, Xi’an, China. #These authors contributed equally to the manuscript. Corresponding author: Dr. Wen Jiang, Tel: +86 29 84771319; E-mail: [email protected]. © The author(s). This is an open access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/). See http://ivyspring.com/terms for full terms and conditions. Received: 2020.09.02; Accepted: 2020.12.22; Published: 2021.01.09 Abstract Background: To investigate the efficacy and safety of hirudin plus aspirin therapy compared with warfarin in the secondary prevention of cardioembolic stroke due to nonvalvular atrial fibrillation (NVAF). Methods: Patients with cardioembolic stroke due to NVAF were prospectively enrolled from 18 collaborating hospitals from Dec 2011 to June 2015. Fourteen days after stroke onset, eligible patients were assigned to the hirudin plus aspirin group (natural hirudin prescribed as the traditional Chinese medicine Maixuekang capsule, 0.75 g, three times daily, combined with aspirin 100 mg, once daily) or the warfarin group (dose-adjusted warfarin targeting international normalized ratio (INR) 2-3, with an initial daily dose of 1.25 mg).