The Bioeffects of a High Frequency Electromagnetic Field in the Microwave Range
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Biofilm Formation by Moraxella Catarrhalis
BIOFILM FORMATION BY MORAXELLA CATARRHALIS APPROVED BY SUPERVISORY COMMITTEE Eric J. Hansen, Ph.D. ___________________________ Kevin S. McIver, Ph.D. ___________________________ Michael V. Norgard, Ph.D. ___________________________ Philip J. Thomas, Ph.D. ___________________________ Nicolai S.C. van Oers, Ph.D. ___________________________ BIOFILM FORMATION BY MORAXELLA CATARRHALIS by MELANIE MICHELLE PEARSON DISSERTATION Presented to the Faculty of the Graduate School of Biomedical Sciences The University of Texas Southwestern Medical Center at Dallas In Partial Fulfillment of the Requirements For the Degree of DOCTOR OF PHILOSOPHY The University of Texas Southwestern Medical Center at Dallas Dallas, Texas March, 2004 Copyright by Melanie Michelle Pearson 2004 All Rights Reserved Acknowledgements As with any grand endeavor, there was a large supporting cast who guided me through the completion of my Ph.D. First and foremost, I would like to thank my mentor, Dr. Eric Hansen, for granting me the independence to pursue my ideas while helping me shape my work into a coherent story. I have seen that the time involved in supervising a graduate student is tremendous, and I am grateful for his advice and support. The members of my graduate committee (Drs. Michael Norgard, Kevin McIver, Phil Thomas, and Nicolai van Oers) have likewise given me a considerable investment of time and intellect. Many of the faculty, postdocs, students and staff of the Microbiology department have added to my education and made my experience here positive. Many members of the Hansen laboratory contributed to my work. Dr. Eric Lafontaine gave me my first introduction to M. catarrhalis. I hope I have learned from his example of patience, good nature, and hard work. -

Pdfفایلی 488.72 K
طؤظاري زانكؤي طةرميان Journal of Garmian University جملة جامعة كرميان http://garmian.edu.krd https://doi.org/10.24271/garmian.164 Isolation and identification of some uncommon bacterial species isolated from different clinical sample Rahman K. Faraj1 and Muhamed N. Maarof 2 1Kalar general hospital/2College of education for pure science-Tikrit university Abstract There are many opportunistic bacterial species that are uncommon and infrequently exist in clinical specimen, most of them are difficult to routine identification, even some of them are poorly documented in clinical specimen. also had no less role in the coordinates of the disease than common bacterial species. Six hundred and fifty samples were collected from patients attending to some hospitals in Sulaimanya City and Kalar General Hospital during the period from October 2015 to November 2016. Samples were firstly cultured on different media in order to isolate and identify bacterial isolates according to cultural characteristics, morphological features and biochemical reactions in addition to Vitek 2 system for identifying uncommon and infrequent isolates. The identification and susceptibility test were performed in Kalar General Hospital. Isolated 286(44%) bacterial strains from different clinical samples, 125 of them were identified by Vitek 2 automated system, while 23(8%) of isolates were considered as uncommon bacterial species. The antimicrobial susceptibility of uncommon isolates, showed significant variation against twenty four antibiotics. Four isolates; Acinatobacter -

Kocuria Varians Infective Endocarditis S Shashikala, R Kavitha, K Prakash, J Chithra, T Shailaja, P Shamsul Karim
The Internet Journal of Microbiology ISPUB.COM Volume 5 Number 2 Kocuria varians infective endocarditis S Shashikala, R Kavitha, K Prakash, J Chithra, T Shailaja, P Shamsul Karim Citation S Shashikala, R Kavitha, K Prakash, J Chithra, T Shailaja, P Shamsul Karim. Kocuria varians infective endocarditis. The Internet Journal of Microbiology. 2007 Volume 5 Number 2. Abstract Kocuria varians belongs to genus Micrococcus. Members of the genus Micrococcus are generally believed to be temporary residents on humans, most frequently found on the exposed skin. We report a case of prosthetic valve endocarditis caused by K.varians in a patient who had undergone aortic valve replacement 8yrs ago. He presented with fever of two weeks duration. Investigations revealed infective endocarditis of prosthetic valve. Blood culture samples grew K.varians. The patient was empirically started on ampicillin and gentamicin intravenously and later with vancomycin and rifampicin. But the patient died due to neurological complications. INTRODUCTION ampicillin 2gm, fourth hourly and gentamicin 60mg, eighth hourly. On third day of admission, he complained of Kocuria is a member of the Micrococcaceae family. 1 Their role as pathogens, when isolated from clinical specimens, headache and vomiting and the next day he developed can be difficult to determine. Since early reports of tremors of right hand and imbalance of gait. CT scan brain endocarditis caused by gram-positive cocci did not reliably done on tenth day of admission revealed subacute/old infarct differentiate between micrococci and coagulase-negative in right middle cerebral artery territory and small lesion at staphylococci, the frequency of micrococcal endocarditis right cerebellar hemisphere. -

Fish Bacterial Flora Identification Via Rapid Cellular Fatty Acid Analysis
Fish bacterial flora identification via rapid cellular fatty acid analysis Item Type Thesis Authors Morey, Amit Download date 09/10/2021 08:41:29 Link to Item http://hdl.handle.net/11122/4939 FISH BACTERIAL FLORA IDENTIFICATION VIA RAPID CELLULAR FATTY ACID ANALYSIS By Amit Morey /V RECOMMENDED: $ Advisory Committe/ Chair < r Head, Interdisciplinary iProgram in Seafood Science and Nutrition /-■ x ? APPROVED: Dean, SchooLof Fisheries and Ocfcan Sciences de3n of the Graduate School Date FISH BACTERIAL FLORA IDENTIFICATION VIA RAPID CELLULAR FATTY ACID ANALYSIS A THESIS Presented to the Faculty of the University of Alaska Fairbanks in Partial Fulfillment of the Requirements for the Degree of MASTER OF SCIENCE By Amit Morey, M.F.Sc. Fairbanks, Alaska h r A Q t ■ ^% 0 /v AlA s ((0 August 2007 ^>c0^b Abstract Seafood quality can be assessed by determining the bacterial load and flora composition, although classical taxonomic methods are time-consuming and subjective to interpretation bias. A two-prong approach was used to assess a commercially available microbial identification system: confirmation of known cultures and fish spoilage experiments to isolate unknowns for identification. Bacterial isolates from the Fishery Industrial Technology Center Culture Collection (FITCCC) and the American Type Culture Collection (ATCC) were used to test the identification ability of the Sherlock Microbial Identification System (MIS). Twelve ATCC and 21 FITCCC strains were identified to species with the exception of Pseudomonas fluorescens and P. putida which could not be distinguished by cellular fatty acid analysis. The bacterial flora changes that occurred in iced Alaska pink salmon ( Oncorhynchus gorbuscha) were determined by the rapid method. -

Kocuria Palustris Sp. Nov, and Kocuria Rhizophila Sp. Nov., Isolated from the Rhizoplane of the Narrow-Leaved Cattail (Typha Angustifolia)
International Journal of Systematic Bacteriology (1999),49, 167-1 73 Printed in Great Britain Kocuria palustris sp. nov, and Kocuria rhizophila sp. nov., isolated from the rhizoplane of the narrow-leaved cattail (Typha angustifolia) Gabor KOV~CS,’Jutta Burghardt,’ Silke Pradella,’ Peter Schumann,’ Erko Stackebrandt’ and KAroly Mhrialigeti’ Author for correspondence: Erko Stackebrandt. Tel: +49 531 2616 352. Fax: +49 531 2616 418. e-mail : [email protected] Department of Two Gram-positive, aerobic spherical actinobacteria were isolated from the Microbiology, Edtvds rhizoplane of narrow-leaved cattail (lypha angustifolia) collected from a Lordnd University, Budapest, Hungary floating mat in the Soroksdr tributary of the Danube river, Hungary. Sequence comparisons of the 16s rDNA indicated these isolates to be phylogenetic 2 DSMZ-German Collection of Microorganisms and neighbours of members of the genus Kocuria, family Micrococcaceae, in which Cell Cultures GmbH, they represent two novel lineages. The phylogenetic distinctness of the two Mascheroder Weg 1b, organisms TA68l and TAGA27l was supported by DNA-DNA similarity values of 38124 Braunschweig, Germany less than 55% between each other and with the type strains of Kocuria rosea, Kocuria kristinae and Kocuria varians. Chemotaxonomic properties supported the placement of the two isolates in the genus Kocuria. The diagnostic diamino acid of the cell-wall peptidoglycan is lysine, the interpeptide bridge is composed of three alanine residues. Predominant menaquinone was MK-7(H2). The fatty acid pattern represents the straight-chain saturated iso-anteiso type. Main fatty acid was anteiso-C,,,,. The phospholipids are diphosphatidylglycerol, phosphatidylglycerol and an unknown component. The DNA base composition of strains TA68l and TAGA27l is 69.4 and 69-6 mol% G+C, respectively. -

Kocuria Varians
CasE REPOrt Kocuria varians – An emerging cause of ocular infections Anita K Videkar1,*, Pranathi B1, Madhuri Gadde1 and Nashrah Nooreen1 1Department of Ophthalmology, Krishna Institute of Medical Sciences, Minister Road, Secunderabad Abstract Purpose: Kocuria varians, which is a nonpathogenic commensal of skin, mucosa and oropharynx. We report a rare case of recurrent conjunctivitis caused by gram positive aerobic microorganism Methods: A 58-year-old male with diabetes mellitus and hypertension presented to us with both eyes recurrent redness, watering, discharge and burning sensation since 3 months. On examination his best corrected visual acuity (BCVA) was 6/9, N6 in right eye and 6/6, N6 in left eye. On anterior segment examination there was upper In view of recurrent conjunctivitis, conjunctival swab was taken and sent for culture and sensitivity. and lower lid edema with matting of lashes, diffuse congestion, chemosis and pseudomembranes in both eyes. Results: culture showedThe organism no growth. was identified as Kocuria varians sensitive to chloramphenicol, gentamycin and resistant to levofloxacin. 2 weeks post treatment with chloramphenicol, patient improved symptomatically and repeat Conclusion: microbiologists to identify and enumerate the virulence and antibiotic susceptibility patterns of such bacteria and for ophthalmologists With increasing in improving reports of theinfections patient associated care and management. with these bacteria, it is now important for clinical Keywords: Kocuria varians; recurrent conjunctivitis; -

Moraxella Catarrhalis Y SU IMPLICACIÓN EN PATOLOGÍA INFECCIOSA
Moraxella catarrhalis Y SU IMPLICACIÓN EN PATOLOGÍA INFECCIOSA Óscar Esparcia y Josefina Magraner Servicio de Microbiología. Hospital Clínico Universitario de Valencia. Moraxella catarrhalis es un diplococo gram-negativo, aerobio, oxidasa positivo. Desde su descubrimiento, a finales del siglo XIX, ha sido objeto tanto de cambios en la nomenclatura y clasificación taxonómica como de su consideración de comensal o patógeno. Actualmente, es aceptado como el tercer patógeno más importante en el tracto respiratorio humano después de Streptococcus pneumoniae y Haemophilus influenzae. En los últimos 20 años, esta bacteria ha emergido como un importante patógeno causante de infecciones en el tracto respiratorio superior de niños y ancianos, e infecciones del tracto respiratorio inferior en adultos con enfermedad pulmonar obstructiva crónica (EPOC). Aproximadamente, el 90% de las cepas son productoras de β-lactamasas. TAXONOMÍA Inicialmente, M. catarrhalis había sido considerada como un organismo comensal, no patógeno, que formaba parte de la flora habitual nasofaringea. Debido también a su morfología, no es de extrañar que esta bacteria fuera englobada dentro del grupo de neisserias no patógenas de la orofaringe. El nombre de esta especie ha cambiado a lo largo de los años y su clasificación taxonómica ha sido causa de gran controversia. Moraxella catarrhalis fue descrita por primera vez en 1896 por Ghon y Pfeiffer y nombrada como Micrococcus catarrhalis. Posteriormente, esta bacteria se clasificó como Neisseria catarrhalis basándose en la similitud de sus características fenotípicas, morfología de las colonias y nicho ecológico con las especies de Neisseria. Berger, en 1963, demostró que el género originario Micrococcus catarrhalis contenía realmente dos especies distintas: Neisseria cinerea y N. -

Description of a Novel Actinobacterium Kocuria Assamensis Sp. Nov., Isolated from a Water Sample Collected from the River Brahmaputra, Assam, India
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by IR@NEIST - North East Institute of Science and Technology (CSIR) Antonie van Leeuwenhoek DOI 10.1007/s10482-010-9547-9 ORIGINAL PAPER Description of a novel actinobacterium Kocuria assamensis sp. nov., isolated from a water sample collected from the river Brahmaputra, Assam, India Chandandeep Kaur • Ishwinder Kaur • Revti Raichand • Tarun Chandra Bora • Shanmugam Mayilraj Received: 3 November 2010 / Accepted: 22 December 2010 Ó Springer Science+Business Media B.V. 2011 Abstract A Gram-positive, pale yellow pigmented (99.1%); however, the DNA–DNA relatedness value actinobacterium, strain S9-65T was isolated from a between strain S9-65T and K. palustris was 20.6%. water sample collected from the river Brahmaputra, On the basis of differential phenotypic characteristics Assam, India and subjected to a polyphasic taxo- and genotypic distinctiveness, strain S9-65T should nomic study. The physiological and biochemical be classified as representative of a novel species properties, major fatty acids (anteiso-C15:0 and Kocuria, for which the name Kocuria assamensis is anteiso-C17:0), estimated DNA G?C content proposed. The type strain is S9-65T (=MTCC (69.2 mol %) and 16S rRNA gene sequence analysis 10622T = DSM 23999T). showed that strain S9-65T belonged to the genus Kocuria. Strain S9-65T exhibited highest 16S rRNA Keywords DNA–DNA hybridization Á FAME Á gene sequence similarity with Kocuria palustris 16S rRNA gene sequence Institute of Microbial Technology Chandigarh and North East Introduction Institute of Science & Technology—a constituent laboratory of Council of Scientific and Industrial Research (CSIR), The genus Kocuria was proposed by Stackebrandt Government of India Chandandeep Kaur, Ishwinder Kaur, Both authors have et al. -
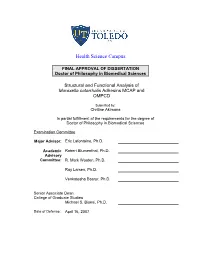
Structural and Functional Analysis of Moraxella Catarrhalis Adhesins MCAP and OMPCD
Health Science Campus FINAL APPROVAL OF DISSERTATION Doctor of Philosophy in Biomedical Sciences Structural and Functional Analysis of Moraxella catarrhalis Adhesins MCAP and OMPCD Submitted by: Chritine Akimana In partial fulfillment of the requirements for the degree of Doctor of Philosophy in Biomedical Sciences Examination Committee Major Advisor: Eric Lafontaine, Ph.D. Academic Robert Blumenthal, Ph.D. Advisory Committee: R. Mark Wooten, Ph.D. Ray Larsen, Ph.D. Venkatesha Basrur, Ph.D. Senior Associate Dean College of Graduate Studies Michael S. Bisesi, Ph.D. Date of Defense: April 16, 2007 Structural and Functional Analysis of Moraxella catarrhalis Adhesins McaP and OMPCD Christine Akimana University of Toledo Health Science Campus 2007 DEDICATION This dissertation is dedicated to my son, Bennett Kiza, who has filled my life with untold blessings. I would like to thank my husband, Nicolas Kiza, and my mother-in-law, whose support and encouragement has enabled me to complete this work. I also would like to thank my parents for their love, inspiration, and support, especially for their hard work that has enabled me to achieve so much in life. There are several people, family members, friends, and mentors, whose support and inspiration has helped me throughout my academic years. For those as well, I offer my full gratitude. ii ACKNOWLEDGEMENTS I would like to thank my major advisor Dr. Eric Lafontaine for giving me the opportunity to work on this very exciting project. I thank him for training me, for sharing his expertise, and for providing me with the opportunity to attend several scientific conferences. I also thank him for his kindness, support, and patience. -

Diagnostics of Neisseriaceae and Moraxellaceae by Ribosomal DNA
JOURNAL OF CLINICAL MICROBIOLOGY, Mar. 2001, p. 936–942 Vol. 39, No. 3 0095-1137/01/$04.00ϩ0 DOI: 10.1128/JCM.39.3.936–942.2001 Copyright © 2001, American Society for Microbiology. All Rights Reserved. Diagnostics of Neisseriaceae and Moraxellaceae by Ribosomal DNA Sequencing: Ribosomal Differentiation of Medical Microorganisms DAG HARMSEN,1* CHRISTIAN SINGER,1 JO¨ RG ROTHGA¨ NGER,2 TONE TØNJUM,3 4 5 2 GERRIT SYBREN DE HOOG, HAROUN SHAH, JU¨ RGEN ALBERT, 1 AND MATTHIAS FROSCH Institute of Hygiene and Microbiology,1 and Department of Computer Science II,2 University of Wu¨rzburg, Wu¨rzburg, Germany; Institute of Medical Microbiology, Department of Molecular Biology, University of Oslo, National Hospital, Oslo, Norway3; Centraalbureau voor Schimmelcultures, Utrecht, The Netherlands4; and National Collections of Type Cultures, Central Public Health Laboratory, London, United Kingdom5 Received 15 December 1999/Returned for modification 15 December 2000/Accepted 21 December 2000 Fast and reliable identification of microbial isolates is a fundamental goal of clinical microbiology. However, in the case of some fastidious gram-negative bacterial species, classical phenotype identification based on either metabolic, enzymatic, or serological methods is difficult, time-consuming, and/or inadequate. 16S or 23S ribosomal DNA (rDNA) bacterial sequencing will most often result in accurate speciation of isolates. There- fore, the objective of this study was to find a hypervariable rDNA stretch, flanked by strongly conserved regions, which is suitable for molecular species identification of members of the Neisseriaceae and Moraxellaceae. The inter- and intrageneric relationships were investigated using comparative sequence analysis of PCR-amplified partial 16S and 23S rDNAs from a total of 94 strains. -

Isolation of Two Kocuria Species Capable of Growing on Various Polycyclic Aromatic Hydrocarbons
African Journal of Biotechnology Vol. 9(24), pp. 3611-3617, 14 June, 2010 Available online at http://www.academicjournals.org/AJB ISSN 1684–5315 © 2010 Academic Journals Full Length Research Paper Isolation of two Kocuria species capable of growing on various polycyclic aromatic hydrocarbons Rifat Zubair Ahmed1*, Nuzhat Ahmed1 and Geoffrey Michael Gadd2 1Centre for Molecular Genetics, University of Karachi, Karachi 75270, Pakistan. 2Division of Molecular Microbiology, College of Life Sciences, University of Dundee, Dundee DD1 5EH, Scotland, UK Accepted 16 March, 2010 Different samples collected from crude oil contaminated beach were enriched for isolation of bacterial strains capable of growing on naphthalene, phenanthrene and fluoranthene. Respiratory reduction of WST-1{4-[3-(4-iodophenyl)-2-(4-nitrophenyl)-2H-5-tetrazolio]-1,3-benzene disulfonate} to a colored formazan showed that one isolated strain CMG2028, identified as Kocuria flava by 16s rRNA, grew on naphthalene and phenanthrene while CMG2042, identified as Kocuria rosea grew on all three polycyclic aromatic hydrocarbons (PAHs). In naphthalene degradation test, 64 and 47% residual naphthalene was extracted after ten days of incubation from culture medium of K. rosea CMG2042 and K. flava CMG2028, respectively, when provided with 0.5 mg ml-1 concentration as sole carbon source. Due to addition of 0.5 mg ml-1 yeast extract as additional carbon source, residual naphthalene extracted was 41 and 55% from K. rosea CMG2042 and K. flava CMG2028, respectively. Both strains exhibited growth on 0.01 mg ml-1 phenanthrene and fluoranthene in yeast extract added or omitted medium but only K. rosea CMG2042 degraded 9% phenanthrene as a sole carbon source. -

Culturable Endophytic Bacteria Associated with Medicinal Plant Ferula Songorica: Molecular Phylogeny, Distribution and Screening for Industrially Important Traits
3 Biotech (2016) 6:209 DOI 10.1007/s13205-016-0522-7 ORIGINAL ARTICLE Culturable endophytic bacteria associated with medicinal plant Ferula songorica: molecular phylogeny, distribution and screening for industrially important traits 1,2,5 1,3 2 1 Yong-Hong Liu • Jian-Wei Guo • Nimaichand Salam • Li Li • 1 1,5 1,4 1,2 Yong-Guang Zhang • Jian Han • Osama Abdalla Mohamad • Wen-Jun Li Received: 15 June 2016 / Accepted: 14 September 2016 Ó The Author(s) 2016. This article is published with open access at Springerlink.com Abstract Xinjiang, a region of high salinity and drought, Overall endophytic species richness of the sample was 58 is a host to many arid and semi-arid plants. Many of these taxa while the sample has statistical values of 4.02, 0.97, plants including Ferula spp. have indigenous pharmaceu- 0.65 and 16.55 with Shannon’s, Simpson, Species evenness tical histories. As many of the medicinal properties of and Margalef, respectively. Root tissues were found to be plants are in tandem with the associated microorganisms more suitable host for endophytes as compared to leaf and residing within the plant tissues, it is advisable to explore stem tissues. Among these endophytic strains, 88 % can the endophytic potential of such plants. In the present grow on nitrogen-free media, 19 % solubilize phosphate, study, diversity of culturable bacteria isolated from while 26 and 40 % are positive for production of protease medicinal plants Ferula songorica collected from and cellulase, respectively. The results confirm that the Hebukesaier, Xinjiang were analyzed. A total of 170 medicinal plant Ferula songorica represents an extremely endophytic bacteria belonging to three phyla, 15 orders, 20 rich reservoir for the isolation of diverged bacteria with families and 27 genera were isolated and characterized by potential for growth promoting factors and biologically 16S rRNA gene sequencing.