In Primary Immunodeficiencies
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Abstracts from the 9Th Biennial Scientific Meeting of The
International Journal of Pediatric Endocrinology 2017, 2017(Suppl 1):15 DOI 10.1186/s13633-017-0054-x MEETING ABSTRACTS Open Access Abstracts from the 9th Biennial Scientific Meeting of the Asia Pacific Paediatric Endocrine Society (APPES) and the 50th Annual Meeting of the Japanese Society for Pediatric Endocrinology (JSPE) Tokyo, Japan. 17-20 November 2016 Published: 28 Dec 2017 PS1 Heritable forms of primary bone fragility in children typically lead to Fat fate and disease - from science to global policy a clinical diagnosis of either osteogenesis imperfecta (OI) or juvenile Peter Gluckman osteoporosis (JO). OI is usually caused by dominant mutations affect- Office of Chief Science Advsor to the Prime Minister ing one of the two genes that code for two collagen type I, but a re- International Journal of Pediatric Endocrinology 2017, 2017(Suppl 1):PS1 cessive form of OI is present in 5-10% of individuals with a clinical diagnosis of OI. Most of the involved genes code for proteins that Attempts to deal with the obesity epidemic based solely on adult be- play a role in the processing of collagen type I protein (BMP1, havioural change have been rather disappointing. Indeed the evidence CREB3L1, CRTAP, LEPRE1, P4HB, PPIB, FKBP10, PLOD2, SERPINF1, that biological, developmental and contextual factors are operating SERPINH1, SEC24D, SPARC, from the earliest stages in development and indeed across generations TMEM38B), or interfere with osteoblast function (SP7, WNT1). Specific is compelling. The marked individual differences in the sensitivity to the phenotypes are caused by mutations in SERPINF1 (recessive OI type obesogenic environment need to be understood at both the individual VI), P4HB (Cole-Carpenter syndrome) and SEC24D (‘Cole-Carpenter and population level. -

Repercussions of Inborn Errors of Immunity on Growth☆ Jornal De Pediatria, Vol
Jornal de Pediatria ISSN: 0021-7557 ISSN: 1678-4782 Sociedade Brasileira de Pediatria Goudouris, Ekaterini Simões; Segundo, Gesmar Rodrigues Silva; Poli, Cecilia Repercussions of inborn errors of immunity on growth☆ Jornal de Pediatria, vol. 95, no. 1, Suppl., 2019, pp. S49-S58 Sociedade Brasileira de Pediatria DOI: https://doi.org/10.1016/j.jped.2018.11.006 Available in: https://www.redalyc.org/articulo.oa?id=399759353007 How to cite Complete issue Scientific Information System Redalyc More information about this article Network of Scientific Journals from Latin America and the Caribbean, Spain and Journal's webpage in redalyc.org Portugal Project academic non-profit, developed under the open access initiative J Pediatr (Rio J). 2019;95(S1):S49---S58 www.jped.com.br REVIEW ARTICLE ଝ Repercussions of inborn errors of immunity on growth a,b,∗ c,d e Ekaterini Simões Goudouris , Gesmar Rodrigues Silva Segundo , Cecilia Poli a Universidade Federal do Rio de Janeiro (UFRJ), Faculdade de Medicina, Departamento de Pediatria, Rio de Janeiro, RJ, Brazil b Universidade Federal do Rio de Janeiro (UFRJ), Instituto de Puericultura e Pediatria Martagão Gesteira (IPPMG), Curso de Especializac¸ão em Alergia e Imunologia Clínica, Rio de Janeiro, RJ, Brazil c Universidade Federal de Uberlândia (UFU), Faculdade de Medicina, Departamento de Pediatria, Uberlândia, MG, Brazil d Universidade Federal de Uberlândia (UFU), Hospital das Clínicas, Programa de Residência Médica em Alergia e Imunologia Pediátrica, Uberlândia, MG, Brazil e Universidad del Desarrollo, -

Practice Parameter for the Diagnosis and Management of Primary Immunodeficiency
Practice parameter Practice parameter for the diagnosis and management of primary immunodeficiency Francisco A. Bonilla, MD, PhD, David A. Khan, MD, Zuhair K. Ballas, MD, Javier Chinen, MD, PhD, Michael M. Frank, MD, Joyce T. Hsu, MD, Michael Keller, MD, Lisa J. Kobrynski, MD, Hirsh D. Komarow, MD, Bruce Mazer, MD, Robert P. Nelson, Jr, MD, Jordan S. Orange, MD, PhD, John M. Routes, MD, William T. Shearer, MD, PhD, Ricardo U. Sorensen, MD, James W. Verbsky, MD, PhD, David I. Bernstein, MD, Joann Blessing-Moore, MD, David Lang, MD, Richard A. Nicklas, MD, John Oppenheimer, MD, Jay M. Portnoy, MD, Christopher R. Randolph, MD, Diane Schuller, MD, Sheldon L. Spector, MD, Stephen Tilles, MD, Dana Wallace, MD Chief Editor: Francisco A. Bonilla, MD, PhD Co-Editor: David A. Khan, MD Members of the Joint Task Force on Practice Parameters: David I. Bernstein, MD, Joann Blessing-Moore, MD, David Khan, MD, David Lang, MD, Richard A. Nicklas, MD, John Oppenheimer, MD, Jay M. Portnoy, MD, Christopher R. Randolph, MD, Diane Schuller, MD, Sheldon L. Spector, MD, Stephen Tilles, MD, Dana Wallace, MD Primary Immunodeficiency Workgroup: Chairman: Francisco A. Bonilla, MD, PhD Members: Zuhair K. Ballas, MD, Javier Chinen, MD, PhD, Michael M. Frank, MD, Joyce T. Hsu, MD, Michael Keller, MD, Lisa J. Kobrynski, MD, Hirsh D. Komarow, MD, Bruce Mazer, MD, Robert P. Nelson, Jr, MD, Jordan S. Orange, MD, PhD, John M. Routes, MD, William T. Shearer, MD, PhD, Ricardo U. Sorensen, MD, James W. Verbsky, MD, PhD GlaxoSmithKline, Merck, and Aerocrine; has received payment for lectures from Genentech/ These parameters were developed by the Joint Task Force on Practice Parameters, representing Novartis, GlaxoSmithKline, and Merck; and has received research support from Genentech/ the American Academy of Allergy, Asthma & Immunology; the American College of Novartis and Merck. -

SUPPLEMENTARY MATERIAL Effect of Next
SUPPLEMENTARY MATERIAL Effect of Next-Generation Exome Sequencing Depth for Discovery of Diagnostic Variants KKyung Kim1,2,3†, Moon-Woo Seong4†, Won-Hyong Chung3, Sung Sup Park4, Sangseob Leem1, Won Park5,6, Jihyun Kim1,2, KiYoung Lee1,2*‡, Rae Woong Park1,2* and Namshin Kim5,6** 1Department of Biomedical Informatics, Ajou University School of Medicine, Suwon 443-749, Korea 2Department of Biomedical Science, Graduate School, Ajou University, Suwon 443-749, Korea, 3Korean Bioinformation Center, Korea Research Institute of Bioscience and Biotechnology, Daejeon 305-806, Korea, 4Department of Laboratory Medicine, Seoul National University Hospital College of Medicine, Seoul 110-799, Korea, 5Department of Functional Genomics, Korea University of Science and Technology, Daejeon 305-806, Korea, 6Epigenomics Research Center, Genome Institute, Korea Research Institute of Bioscience and Biotechnology, Daejeon 305-806, Korea http//www. genominfo.org/src/sm/gni-13-31-s001.pdf Supplementary Table 1. List of diagnostic genes Gene Symbol Description Associated diseases ABCB11 ATP-binding cassette, sub-family B (MDR/TAP), member 11 Intrahepatic cholestasis ABCD1 ATP-binding cassette, sub-family D (ALD), member 1 Adrenoleukodystrophy ACVR1 Activin A receptor, type I Fibrodysplasia ossificans progressiva AGL Amylo-alpha-1, 6-glucosidase, 4-alpha-glucanotransferase Glycogen storage disease ALB Albumin Analbuminaemia APC Adenomatous polyposis coli Adenomatous polyposis coli APOE Apolipoprotein E Apolipoprotein E deficiency AR Androgen receptor Androgen insensitivity -

The Potential Use of Intestinal Stem Cells to Treat Patients with Intestinal Failure
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by eScholarship - University of California UCLA UCLA Previously Published Works Title Concise Review: The Potential Use of Intestinal Stem Cells to Treat Patients With Intestinal Failure. Permalink https://escholarship.org/uc/item/1qr6h03t Journal Stem cells translational medicine, 6(2) ISSN 2157-6564 Authors Hong, Sung Noh Dunn, James CY Stelzner, Matthias et al. Publication Date 2016-09-16 DOI 10.5966/sctm.2016-0153 Peer reviewed eScholarship.org Powered by the California Digital Library University of California Tissue Engineering and Regenerative Medicine TISSUE ENGINEERING AND REGENERATIVE MEDICINE Concise Review: Review: The The Potential Potential Use Use of of Intestinal Intestinal Stem Stem Cells to to Treat Treat Patients Patients with With Intestinal Intestinal Failure Failure aDivision of Gastroenterology SUNG NOH HONG,a,b JAMES C.Y. DUNN,c MATTHIAS STELZNER,d,e MART´IN G. MART´INa and Nutrition, Department of Pediatrics, Mattel Children’s Key Words. Intestinal failure x Congenital diarrhea x Microvillus inclusion disease x x Hospital and David Geffen Congenital tufting enteropathy Intestinal stem cell School of Medicine, University of California Los ABSTRACT Angeles, Los Angeles, California, USA; bDepartment Intestinal failure is a rare life-threatening condition that results in the inability to maintain normal of Medicine, Samsung growth and hydration status by enteral nutrition alone. Although parenteral nutrition and whole or- Medical Center, gan allogeneic transplantation have improved the survival of these patients, current therapies are associated with a high risk for morbidity and mortality. Development of methods to propagate adult Sungkyunkwan University human intestinal stem cells (ISCs) and pluripotent stem cells raises the possibility of using stem cell- School of Medicine, Seoul, c based therapy for patients with monogenic and polygenic forms of intestinal failure. -

Statistical Analysis Plan
Cover Page for Statistical Analysis Plan Sponsor name: Novo Nordisk A/S NCT number NCT03061214 Sponsor trial ID: NN9535-4114 Official title of study: SUSTAINTM CHINA - Efficacy and safety of semaglutide once-weekly versus sitagliptin once-daily as add-on to metformin in subjects with type 2 diabetes Document date: 22 August 2019 Semaglutide s.c (Ozempic®) Date: 22 August 2019 Novo Nordisk Trial ID: NN9535-4114 Version: 1.0 CONFIDENTIAL Clinical Trial Report Status: Final Appendix 16.1.9 16.1.9 Documentation of statistical methods List of contents Statistical analysis plan...................................................................................................................... /LQN Statistical documentation................................................................................................................... /LQN Redacted VWDWLVWLFDODQDO\VLVSODQ Includes redaction of personal identifiable information only. Statistical Analysis Plan Date: 28 May 2019 Novo Nordisk Trial ID: NN9535-4114 Version: 1.0 CONFIDENTIAL UTN:U1111-1149-0432 Status: Final EudraCT No.:NA Page: 1 of 30 Statistical Analysis Plan Trial ID: NN9535-4114 Efficacy and safety of semaglutide once-weekly versus sitagliptin once-daily as add-on to metformin in subjects with type 2 diabetes Author Biostatistics Semaglutide s.c. This confidential document is the property of Novo Nordisk. No unpublished information contained herein may be disclosed without prior written approval from Novo Nordisk. Access to this document must be restricted to relevant parties.This -

Autoimmune Polyendocrine Syndromes
The new england journal of medicine review article medical progress Autoimmune Polyendocrine Syndromes George S. Eisenbarth, M.D., Ph.D., and Peter A. Gottlieb, M.D. From the Barbara Davis Center for Child- he autoimmune polyendocrine syndromes are diverse, and hood Diabetes, University of Colorado their diversity is a characteristic that is both clinically important and instruc- Health Sciences Center, Denver. Address re- t 1-4 print requests to Dr. Eisenbarth at the Bar- tive when their basic immunologic features are considered (Table 1). These bara Davis Center for Childhood Diabetes, syndromes include monogenic disorders (such as autoimmune polyendocrine syn- University of Colorado Health Sciences Cen- drome type I, which has classic and characteristic disease associations5) and complex ter, 4200 E. Ninth Ave., Box B140, Denver, CO 80262, or at george.eisenbarth@uchsc. genetic disorders (such as autoimmune polyendocrine syndrome type II, in which the 6 edu. component diseases are more variable ). Some of the component disorders are common (e.g., thyroid autoimmunity and celiac disease), whereas others are rare (e.g., Addison’s N Engl J Med 2004;350:2068-79. Copyright © 2004 Massachusetts Medical Society. disease and myasthenia gravis). Some of the disorders are usually asymptomatic (e.g., celiac disease); others are symptomatic but typically diagnosed after years of illness (Addison’s disease, which features severe fatigue and nausea, and pernicious anemia, which causes neuropathic symptoms); and still others are clinically dramatic at the time of diagnosis (type 1A diabetes, also known as immune-mediated diabetes and formerly called insulin-dependent diabetes). The term “polyendocrine” itself is a misnomer, in that not all patients have multiple endocrine disorders, and many have nonendocrine autoimmune diseases. -

Abstracts Arch Dis Child: First Published As 10.1136/Archdischild-2012-302724.0957 on 1 October 2012
Abstracts Arch Dis Child: first published as 10.1136/archdischild-2012-302724.0957 on 1 October 2012. Downloaded from antituberculosis therapy and fever resolved after 45 days. A nurse is É Karaszi, K Kalocsai, K Kardics, Z Liptai, A Trethon. Pediatric Infectology, St. László going to her house daily to check the patient’s adherence during the Hospital, Budapest, Hungary one year treatment. Background and Aims A ten year-old girl with hyper IgE syn- drome caused by DOCK8 mutation was admitted to our hospital due to neuropsychiatric symptoms. Cranial MRI revealed multifo- cal cerebral lesions. Our aim was to clarify the etiology of these lesions by extended microbiology tests and comprehensive search in the literature then provide her with proper treatment options. Methods Multiple blood and cerebrospinal fluid samples and were examined for bacterial and fungal culture, Aspergillus and Crypto- coccus antigen, HSV, CMV, Mycobacterium and Toxoplasma PCR, panfungal PCR and for Toxocara and E. hystolytica serology. Brain biopsy was also done for histology, bacterial and fungal culture. Results All diagnostic assays showed negative results therefore causative agents could not be identified For treatment, ceftriaxon and metronidazole combination was initially used accompanied by slight clinical and neuroradiological progression. Considering the possible presence of vascular brain lesions, high dose paren- teral steroid treatment was introduced together with preemptive parenteral voriconazol therapy. Further progression in the clini- cal and radiological status was observed. Although there is no Abstract 953 Figure 1 Chest radiography of miliary tuberculosis report of cerebral toxoplasmosis in this disorder, empirical anti- toxoplasma treatment was initiated with significant clinical Conclusion The diagnosis of MT can be clearly invoked with a improvement and radiological regression after 6-week therapy. -

Allogeneic Hematopoietic Cell Transplantation for Genetic Diseases and Acquired Anemias
MEDICAL POLICY POLICY TITLE ALLOGENEIC HEMATOPOIETIC CELL TRANSPLANTATION FOR GENETIC DISEASES AND ACQUIRED ANEMIAS POLICY NUMBER MP-9.055 Original Issue Date (Created): 10/1/2014 Most Recent Review Date (Revised): 2/24/2021 Effective Date: 8/1/2021 POLICY PRODUCT VARIATIONS DESCRIPTION/BACKGROUND RATIONALE DEFINITIONS BENEFIT VARIATIONS DISCLAIMER CODING INFORMATION REFERENCES POLICY HISTORY I. POLICY Allogeneic hematopoietic cell transplantation is considered medically necessary for select patients with the following disorders: Hemoglobinopathies Sickle cell anemia for children or young adults with either a history of prior stroke or at increased risk of stroke or end-organ damage. Homozygous β -thalassemia (i.e., thalassemia major Bone marrow failure syndromes Aplastic anemia including hereditary (including Fanconi anemia, dyskeratosis congenita, Shwachman-Diamond, Diamond-Blackfan) or acquired (e.g., secondary to drug or toxin exposure) forms. Primary immunodeficiencies Absent or defective T cell function (e.g., severe combined immunodeficiency, Wiskott- Aldrich syndrome, X-linked lymphoproliferative syndrome) Absent or defective natural killer function (e.g. Chediak-Higashi syndrome) Absent or defective neutrophil function (e.g. Kostmann syndrome, chronic granulomatous disease, leukocyte adhesion defect) (See Policy Guideline # 1.) Inherited metabolic disease Lysosomal and peroxisomal storage disorders except Hunter, Sanfilippo, and Morquio syndromes (See Policy Guideline # 2) Page 1 MEDICAL POLICY POLICY TITLE ALLOGENEIC HEMATOPOIETIC CELL TRANSPLANTATION FOR GENETIC DISEASES AND ACQUIRED ANEMIAS POLICY NUMBER MP-9.055 Genetic disorders affecting skeletal tissue Infantile malignant osteopetrosis (Albers-Schonberg disease or marble bone disease) POLICY GUIDELINES Guideline 1 The following lists the immunodeficiencies that have been successfully treated by allogeneic hematopoietic cell transplantation (allo-HCT) (Gennery & Cant et al, 2008). -

Primary Immune Regulatory Disorders and Targeted Therapies REVIEW
Kolukısa B. and Barış S: Immune Dysregulation and Therapies REVIEW DOI: 10.4274/tjh.galenos.2021.2020.0724 Turk J Hematol 2021;38:1-14 Primary Immune Regulatory Disorders and Targeted Therapies Primer İmmün Regülatuvar Hastalıklar ve Hedeflenmiş Tedaviler Burcu Kolukısa1,2,3, Safa Barış1,2,3 1Marmara University Faculty of Medicine, Division of Pediatric Allergy and Immunology, İstanbul, Turkey 2İstanbul Jeffrey Modell Diagnostic and Research Center for Primary Immunodeficiencies, İstanbul, Turkey 3The Işıl Berat Barlan Center for Translational Medicine, İstanbul, Turkey Abstract Öz Primary immune regulatory disorders (PIRDs) are a group of Primer immündisregülasyon hastalıkları (PİRH), immün sistemin diseases belonging to inborn errors of immunity. They usually doğuştan gelen bozuklukları içerisinde yer alan bir grup hastalıktır. exhibit lymphoproliferation, autoimmunities, and malignancies, Çoğunlukla lenfoproliferasyon, otoimmünite ve malignite bulguları with less susceptibility to recurrent infections. Unlike classical sergilerler ve bu grupta tekrarlayan enfeksiyonlara yatkınlık daha primary immune deficiencies, autoimmune manifestations, such as az olabilmektedir. Ayrıca diğer klasik primer immün yetmezliklerden cytopenias, enteropathy can be the first symptom of diseases, and farklı olarak otoimmün bulgular (örneğin; sitopeniler, enteropati) they are typically resistant to treatment. Increasing awareness of hastalığın ilk semptomu olarak çıkabilmekte ve tipik olarak tedaviye PIRDs among specialists and a multidisciplinary team approach would direnç gösterebilmektedir. Primer immün disregülasyon hastalıkları provide early diagnosis and treatment that could prevent end-organ hakkındaki farkındalığın artırılması ve multidisipliner yaklaşımlar, damage related to the diseases. In recent years, many PIRDs have been erken tanı ve tedaviyi mümkün kılarak, hastalıkla ilişkili gelişebilecek described, and understanding the immunological pathways linked to uç-organ hasarlarını önlemeye yardımcı olabilecektir. -
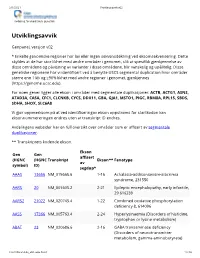
Utviklingsavvik V02
2/1/2021 Utviklingsavvik v02 Avdeling for medisinsk genetikk Utviklingsavvik Genpanel, versjon v02 * Enkelte genomiske regioner har lav eller ingen sekvensdekning ved eksomsekvensering. Dette skyldes at de har stor likhet med andre områder i genomet, slik at spesifikk gjenkjennelse av disse områdene og påvisning av varianter i disse områdene, blir vanskelig og upålitelig. Disse genetiske regionene har vi identifisert ved å benytte USCS segmental duplication hvor områder større enn 1 kb og ≥90% likhet med andre regioner i genomet, gjenkjennes (https://genome.ucsc.edu). For noen gener ligger alle ekson i områder med segmentale duplikasjoner: ACTB, ACTG1, ASNS, ATAD3A, CA5A, CFC1, CLCNKB, CYCS, DDX11, GBA, GJA1, MSTO1, PIGC, RBM8A, RPL15, SBDS, SDHA, SHOX, SLC6A8 Vi gjør oppmerksom på at ved identifiseringav ekson oppstrøms for startkodon kan eksonnummereringen endres uten at transkript ID endres. Avdelingens websider har en full oversikt over områder som er affisert av segmentale duplikasjoner. ** Transkriptets kodende ekson. Ekson Gen Gen affisert (HGNC (HGNC Transkript Ekson** Fenotype av symbol) ID) segdup* AAAS 13666 NM_015665.6 1-16 Achalasia-addisonianism-alacrimia syndrome, 231550 AARS 20 NM_001605.2 2-21 Epileptic encephalopathy, early infantile, 29 616339 AARS2 21022 NM_020745.4 1-22 Combined oxidative phosphorylation deficiency 8, 614096 AASS 17366 NM_005763.4 2-24 Hyperlysinaemia (Disorders of histidine, tryptophan or lysine metabolism) ABAT 23 NM_020686.6 2-16 GABA transaminase deficiency (Disorders of neurotransmitter metabolism, gamma-aminobutyrate) -

Gross Deletions in TCOF1 Are a Cause of Treacher–Collins–Franceschetti Syndrome
European Journal of Human Genetics (2012) 20, 769–777 & 2012 Macmillan Publishers Limited All rights reserved 1018-4813/12 www.nature.com/ejhg ARTICLE Gross deletions in TCOF1 are a cause of Treacher–Collins–Franceschetti syndrome Michael Bowman1, Michael Oldridge1, Caroline Archer1, Anthony O’Rourke1, Joanna McParland2, Roel Brekelmans3, Anneke Seller1 and Tracy Lester*,1 Treacher–Collins–Franceschetti syndrome (TCS) is an autosomal dominant craniofacial disorder characterised by midface hypoplasia, micrognathia, downslanting palpebral fissures, eyelid colobomata, and ear deformities that often lead to conductive deafness. A total of 182 patients with signs consistent with a diagnosis of TCS were screened by DNA sequence and dosage analysis of the TCOF1 gene. In all, 92 cases were found to have a pathogenic mutation by sequencing and 5 to have a partial gene deletion. A further case had a novel in-frame deletion in the alternatively spliced exon 6A of uncertain pathogenicity. The majority of the pathogenic sequence changes were found to predict premature protein termination, however, four novel missense changes in the LIS1 homology motif at the 5¢ end of the gene were identified. The partial gene deletions of different sizes represent B5.2% of all the pathogenic TCOF1 mutations identified, indicating that gene rearrangements account for a significant proportion of TCS cases. This is the first report of gene rearrangements resulting in TCS. These findings expand the TCOF1 mutation spectrum indicating that dosage analysis should be performed