2020 Annual Overview of Healthcare in the GCC Growth Opportunities For
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sustaining the Health of a Nation
Hamad Medical Corporation Corporation Medical Hamad Annual Report 2011/12 Annual Report 2011/12 Sustaining the health of a nation Our vision is to be an internationally recognized integrated healthcare system, acclaimed for excellence in healthcare, education and research, and to play a premier role in the sustainability of health in Qatar. His Highness Sheikh Hamad Bin Khalifa Al-Thani Emir of the State of Qatar His Highness Sheikh Tamim Bin Hamad Al-Thani Heir Apparent Our belief in patient-centered healthcare means always putting the people of Qatar first. Hamad Medical Corporation 4 Annual Report 2011/12 We do that by excelling in three key areas: Clinical Services During 2011/12 Hamad Medical Corporation continued to enhance its services and facilities in order to deliver high-quality care of an international standard. Page 16 Research, Education and Training We believe research delivers valuable and tangible benefits to patients and has a direct and positive impact on the quality of clinical outcomes. Page 34 Support Services By continually investing in people, innovation and technology, we are setting a standard of true excellence. Page 40 Hamad Medical Corporation Annual Report 2011/12 5 Managing Director’s Foreword The last year has been an exciting and energizing one for Hamad Medical Corporation. We have made great progress on a range of the issues that matter most to our patients and our people. This has been made possible by the excellent work of our staff at all levels and by the enlightened leadership of our country which has placed universal, high quality healthcare and innovative education and research at the heart of our nation’s success. -

Internationalization of Academic Health Systems: Opportunities for Partnership
Internationalization of Academic Health Systems: Opportunities for Partnership Montreal, Quebec November 2012 1. Qatar 2. Hamad Medical Corporation as an Aspiring Academic Health System 3. Partnership 4. Key Questions 1. Qatar QATAR IS A SMALL, WEALTHY COUNTRY WITH GREAT AMBITION Geographically small: 11,437 sq km Small but diverse population: 1.8million people (approximately the same as the city of Montreal) of which 300,000 (one in six) are Qatari nationals Experienced rapid growth: The population has more than doubled in ten years Wealthy: highest GDP per capita in world (over $100,000) Reliant on oil and gas: responsible for 70% of government revenue; owns one-seventh of world’s gas reserves The Government’s main priority is to diversify the economy to make it sustainable. It also wants to play a bigger role on the world stage, while maintaining Qatari culture: - Played a key role in many international negotiations (such as in Darfur), established an award winning news network (Al Jazeera) and won the right to host the 2022 Football World Cup - Government’s vision is to transition to a ‘knowledge-based’ economy in order to reduce the dependence on oil and gas. One aspect of this is to become a world leader in healthcare and medical research 2. HMC as an Aspiring Academic Health System HMC IS A BUSY, GOVERNMENT FUNDED HOSPITAL SYSTEM UNDERGOING A PERIOD OF RAPID EXPANSION AND CHANGE HMC is a government funded non-profit provider. Through its eight hospitals and with an annual budget of c. $2bn it provides 90% of the acute healthcare in Qatar. -

Single Male Laborers' Health in Qatar
Improving Single Male Laborers’ Health in Qatar Policy Brief About Georgetown University in Qatar Established in 1789, Georgetown University is one of the world’s leading academic and research institutions, offering a unique educational experience that prepares the next generation of global citizens to lead and make a difference in the world. Georgetown University in Qatar (GU-Q), founded in 2005, empowers students and shapes the human capacity that the MENA region needs for the 21st century, providing a holistic educational experience built upon the highest academic standards. GU-Q’s Bachelor of Science in Foreign Service (BSFS) stresses multidisciplinary studies in a global context. It is the same globally respected program and curriculum offered at the Georgetown University Edmund A. Walsh School of Foreign Service in Washington D.C. The BSFS degree is offered in one of four majors: International Economics, International Politics, Culture and Politics, and International History. Students can also pursue a certificate in one of three concentrations: Arab and Regional Studies, American Studies, or Media and Politics. To learn more about GU-Q’s exciting events and programs, or to benefit from its wide array of research, please visit qatar.sfs.georgetown.edu Improving Single Male About the Center for International and Regional Studies (CIRS) Laborers’ Health in Qatar Established in 2005, the Center for International and Regional Studies at Georgetown University in Qatar is a premier research institute devoted to the academic study of regional and international issues through dialogue and exchange of ideas; research and scholarship; and engagement with national and international scholars, opinion makers, practitioners, and activists. -

Community Health Nursing in Oman
: Curre re nt a R C e h v t i l e Al-Zadjali M., Health Care Current Reviews 2014, 2:3 a w e s H Health Care: Current Reviews DOI: 10.4172/2375-4273.1000128 ISSN: 2375-4273 Short Communication Open Access Community Health Nursing In Oman Al-Zadjali M1, Sinawi F1, Sheeba M1, Al Busaidi M1, Al Jabri S1 and Silbermann M2* 1The Oman Specialized Nursing Institute, Sultanate of Oman, Oman 2The Middle East Cancer Consortium, Israel *Corresponding author: Dr. Michael Silbermann, Executive Director, P.O. Box 7495, Haifa 31074, Israel, Tel: 972-505606335; E-mail: [email protected] Rec date: Jul 29, 2014, Acc date: Sep29, 2014; Pub date: Oct 1, 2014 Copyright:© 2014 Al-Zadjali M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Introduction adopted the global goal of “Health for All by Year 2000”. The primary healthcare services were given the priority in Oman since the Alma- Community health nursing is one of the nursing specialties that Ata declaration in 1978 as it was considered as the first portal of entry have always been valued for its role in providing care in a variety of to all levels of care as well as the key strategy for achieving the target of practice settings including homes, schools, work places or other the global goal. Consequently, in year 1980, the number of the health community institutions [1]. -

The Anglo-Omani Society Review 2018
REVIEW 2018 THE ANGLO-OMANI SOCIETY THE ANGLO-OMANI SOCIETY REVIEW 2018 COVER PHOTO: RAF Red Arrows flying over the Arches of Oman REVIEW 2018 Photo Credit: Julian Glyn-Owen THE ANGLO-OMANI SOCIETY CONTENTS 6 CHAIRMAN’S OVERVIEW 65 MUSCAT IN SEVILLE 9 AWARD OF ORDER TO COL. NIGEL KNOCKER 66 ANGLO-OMANI LUNCHEON 2017 10 THE ARCHES OF OMAN 69 THE SOCIETY’S GRANT SCHEME 15 DUQM – WHERE IT ALL BEGAN 70 AOS LECTURE PROGRAMME 18 THE GROWING PROBLEM OF PLASTICS 72 ARABIC LANGUAGE SCHEME POLLUTING OUR OCEANS 75 GAP YEAR SELECTION PROCESS 76 GAP YEAR SCHEME REPORT 20 OMAN’S SPECIAL SEAS: DIVING IN THE HALLANIYAT ISLANDS 25 VISIT TO OMAN BY THEIR ROYAL HIGHNESSES THE PRINCE OF WALES AND THE DUCHESS OF CORNWALL 80 NEW GENERATION GROUP 29 OMAN’S WHALES, DOLPHINS AND TURTLES 91 YOUTH ENGAGEMENT IN THE PRIVATE SECTOR 34 MAJLIS AL JINN – ‘THE MOST BEAUTIFUL IN THE SULTANATE LARGE CAVE IN THE WORLD’ 93 ENTREPRENEURIAL IDENTITIES 40 THE SOOTY FALCON: A FLAGSHIP SPECIES FOR BIRD CONSERVATION IN OMAN 96 MUSCAT AIRPORT 44 ‘CORRIDORS OF POWER’ – AN ART EXHIBITION 99 AOS INTERNSHIP PROGRAMME: BY OMANI ARTIST EMAN ALI MEET OUR ALUMNI! 48 DHOFAR – OMAN BOTANIC EXPEDITION 2018 102 RENAISSANCE DAY CELEBRATIONS “OMAN: LAND OF PEACE” 53 MUSCAT TO SALALAH – CROSS COUNTRY CYCLING RECORD ATTEMPT 105 OMAN’S APPROACH TO CLIMATE CHANGE 56 OMAN STATE COUNCIL DELEGATION 108 HEALTHCARE IN OMAN: 1970-2050 MARCH 2018 111 OMANI SOCIAL MEDIA, THE NEXT GENERATION 58 OMAN AND ITS NEIGHBOURS 113 OBITUARY – THE HON. IVOR LUCAS, CMG 60 THE OMANI-BRITISH BUSINESS COUNCIL 115 THE HISTORY OF THE SOCIETY 62 BP’S AL KHAZZAN PROJECT BUILDING OMAN’S FUTURE 117 BOOK REVIEWS 3 REVIEW 2018 THE ANGLO-OMANI SOCIETY Society Address 34, Sackville Street, London W1S 3ED +44 (0)20 7851 7439 Patron www.angloomanisociety.com HM Sultan Qaboos bin Said Advertising Christine Heslop 18 Queen’s Road, Salisbury, Wilts. -

Hamad Medical Corporation Receives Prestigious Accreditation Award
HAMAD MEDICAL CORPORATION RECEIVES PRESTIGIOUS ACCREDITATION AWARD (DOHA, Qatar, 19 September 2016) – Hamad Medical Corporation (HMC) has been formally recognized by Joint Commission International (JCI) for being the first healthcare organization in the world to have all its hospitals qualified under the JCI Academic Medical Center accreditation program, demonstrating not only HMC’s commitment to continuous delivery of safe, high quality care but also Qatar’s leadership commitment to the health sector as a whole. This prestigious distinction was achieved following a comprehensive on-site survey earlier this year by specialist JCI surveyors who evaluated all of HMC's eight hospitals against a set of stringent internationally approved healthcare standards. All HMC hospitals have received the official Gold Seal of Approval® for accreditation under the JCI Academic Medical Center Hospital standards. Simultaneous accreditation across all hospitals is an outstanding achievement. It demonstrates a commitment to providing great care all the time, while sharing new learnings and developing innovative ways of delivering high quality care. The award was presented by Ms Paula Wilson, President and Chief Executive Officer of Joint Commission Resources and Joint Commission International and Dr Mark R. Chassin, President and Chief Executive Officer of The Joint Commission, to Her Excellency Dr Hanan Mohamed Al Kuwari, Qatar Minister of Public Health, during a special ceremony at JCI headquarters outside Chicago, Illinois in the United States. H.E. Dr Al Kuwari expressed her delight at receiving the commemorative award and certificate for HMC's achievement: "This recognition is an enormous achievement and accolade for Qatar's leading tertiary and secondary healthcare provider. -

The Development of the Qatar Healthcare System: a Review of the Literature
International Journal of Clinical Medicine, 2015, 6, 177-185 Published Online March 2015 in SciRes. http://www.scirp.org/journal/ijcm http://dx.doi.org/10.4236/ijcm.2015.63023 The Development of the Qatar Healthcare System: A Review of the Literature Annekathryn Goodman Massachusetts General Hospital, Division of Gynecologic Oncology, Department of Obstetrics and Gynecology, Obstetrics, Gynecology and Reproductive Biology Harvard Medical School, Boston, MA, USA Email: [email protected] Received 3 March 2015; accepted 18 March 2015; published 25 March 2015 Copyright © 2015 by author and Scientific Research Publishing Inc. This work is licensed under the Creative Commons Attribution International License (CC BY). http://creativecommons.org/licenses/by/4.0/ Abstract Background: Qatar, one of the smallest and wealthiest countries in the world, is a newly emerging healthcare system. Medical leadership in Qatar has had to create an infrastructure for medical care over the past twenty years. The purpose of this paper is to review the challenges and achieve- ments of the newly emerging Qatar healthcare system. Methods: PubMed was searched using MESH terms: Qatar, healthcare, medical development, medical insurance and medical history. Websites of the World Bank, CIA fact book, Qatar Ministry of Health, Hamad Medical Corporation, Organiza- tion for Economic Co-operation and Development and the US State department were searched for information about Qatar’s healthcare system and its history. Results: Qatar is a rapidly growing, multicultural country with over 80 nationalities represented. Qatar has developed a healthcare system with universal coverage. Up until 2014, the government has subsidized all care. There are plans to develop a medical insurance system. -

Precision Medicine in Qatar Could Initial Translation of This Vision
GENOMICS Precision medicine: paving the way to better healthcare in Qatar Dr Lotfi Chouchane tells International Innovation about Qatar scientists’ groundbreaking efforts to bring precision medicine to the nation, outlining the potential advantages it holds and the challenges that lie ahead Precision medicine represents a tailored small size of the Qatari population and the lagged behind. This is reflected in the modest response to an individual’s healthcare needs. recent launch of Qatar Genome Project will presence of biotech companies in the Qatar What are the more specific benefits of this reinforce the implementation of a precision Science & Technology Park. approach for a population such as that medicine programme. of Qatar? What are the challenges surrounding What were the main objectives of launching precision medicine, including cultural The Qatari population is small, comprising the Qatar Genome Project? misconceptions and difficulties in about 300,000 individuals. We showed capacity building? recently that it is genetically diverse; at Qatar not only wants to provide accessible least three different genetic signatures were healthcare services to the entire population The most challenging task is how to convince identified, reflecting the history of human but also to deliver precision medicine and healthcare practitioners of the attractiveness migration to Qatar. Similar population healthcare services managed according to of precision medicine for their daily practice. stratification is expected to be found in other world-class standards. The Qatar Genome Without their buying into it, it would be difficult Gulf Cooperation Council (GCC) populations. Project is an ambitious programme that to make patients adhere and contribute to the This genetic diversity will undoubtedly aims to provide whole genome sequences success of the programme. -

QATAR Information Sheet
QATAR Information Sheet © International Affiliate of the Academy of Nutrition and Dietetics 2020 Credentialing Verification Authority: Qatar Council for Healthcare Practitioners Communication: Arabic, English Ongoing Nutrition Activities in Qatar 1. National Dietetic Association None at the moment. Related organizations Qatar Diabetes Association • Address: Rawdat Al Khail , Al Muntaza, Doha, State of Qatar • Phone Number: (+974) 44547341 • Website: httPs://qda.org.qa/home/ 2. National Nutrition Programmes/Projects • DeveloPment of Qatar Dietary Guidelines To download PDF coPy: httPs://www.moPh.gov.qa/Admin/Lists/PublicationsAttachments/Attachmen ts/68/MOPH_DIETARY_BOOKLET_ENG.PDF • Several awareness campaigns, such as: o World Food Day § Held on October 16 each year § Aim is to emphasize the need of eradicating hunger, and instilling it as a moral and human responsibility of all § To commemorate the day, Qatar Charity distributed 100,000 meals to refugees and Poor families in Palestine, Turkey, and Lebanon § At Hamad Medical Corporation, awareness booth was also installed in one of its facilities o World Obesity Day § Held on October 28, 2019 at Hamad General Hospital § Led by Bariatric dietitians of Hamad Medical Corporation § The campaign includes various booths installed Presenting food Portion sizes, healthy cooking tiPs and reciPes, information on Fad diets, diet Pre and Post Bariatric surgery, with educational materials distributed, and lecture Presentation on Diet and Obesity o World Diabetes Day § Every November 14 each year § Led by Ministry of Public Health, in cooPeration with Hamad Medical Corporation, Primary Health Care Corporation, Sidra Medicine and Qatar Diabetes Association § Part of Qatar National Diabetes Strategy 2016-2022 § The campaign includes nutrition, Physical activity, and awareness by conducting questionnaires, counselling Patients, conducting workshoPs, and launching of its website 3. -
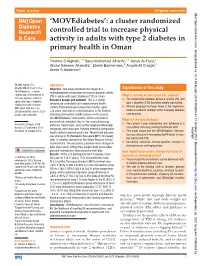
A Cluster Randomized Controlled Trial to Increase Physical Activity in Adults with Type 2 Diabetes in Primary Health in Oman
Clinical Care/Education/Nutrition Open access Original research BMJ Open Diab Res Care: first published as 10.1136/bmjdrc-2018-000605 on 31 October 2018. Downloaded from ‘MOVEdiabetes’: a cluster randomized controlled trial to increase physical activity in adults with type 2 diabetes in primary health in Oman Thamra S Alghafri,1,2 Saud Mohamed Alharthi,1,2 Yahya Al-Farsi,3 Abdul Hakeem Alrawahi,4 Elaine Bannerman,5 Angela M Craigie,5 Annie S Anderson5 To cite: Alghafri TS, ABSTRACT Alharthi SM, Al-Farsi Y, et al. Objective This study examined the impact of a Significance of this study ‘MOVEdiabetes’: a cluster multicomponent intervention to increase physical activity randomized controlled trial to (PA) in adults with type 2 diabetes (T2D) in Oman. What is already known about this subject? increase physical activity in Research design and methods This is a cluster ► The relationship between physical activity (PA) and adults with type 2 diabetes type 2 diabetes (T2D) has been widely researched. in primary health in Oman. randomized controlled trial in eight primary health ► Minimal progress has been made in the implemen- BMJ Open Diab Res Care centers. Participants were physically inactive, aged tation of research findings within everyday diabetes 2018;6:e000605. doi:10.1136/ ≥18 years, and with no contraindication to PA. Patients bmjdrc-2018-000605 attending intervention health centers (n=4) received care practice. the ‘MOVEdiabetes’ intervention, which consisted of What are the new findings? personalized, individual face-to-face consultations by Received 22 August 2018 ► The current 1-year intervention was delivered in a dietitians. Pedometers and monthly telephone WhatsApp copyright. -

Development of a Model to Deliver Primary Health Care in Qatar
Open access Original research Integ Health J: first published as 10.1136/ihj-2020-000040 on 30 December 2020. Downloaded from Development of a model to deliver primary health care in Qatar Mohamed Ahmed Syed , Hanan Al Mujalli, Catherine Maria Kiely, Hamda Abdulla A/Qotba To cite: Syed MA, Al Mujalli H, ABSTRACT Key messages Kiely CM, et al. Development Background Healthcare providers around the world of a model to deliver are seeking to manage the rising burden of chronic What is already known about this subject? primary health care in Qatar. conditions against a backdrop of both growing and ageing Integrated Healthcare Journal Many studies have been published highlighting the populations as well as greater expectations of health ► 2020;2:e000040. doi:10.1136/ importance of family medicine and primary care services. This paper describes the development of an ihj-2020-000040 models, however, few have focused on their de- integrated primary care model ‘the family medicine model velopment and adaptation to meet local context in Received 01 March 2020 (FMM)’ to deliver primary healthcare in Qatar to better delivering primary care, in particular, in the Middle Revised 12 October 2020 address some of the healthcare challenges faced. Eastern Region. Accepted 08 December 2020 Methods A developmental approach was adopted in defining an FMM for Qatar that could potentially address What does this study add? health needs of its population, while acknowledging local ► This study describes the development and adapta- context and addressing complexities. A literature review tion of a family medicine model (FMM) to deliver uni- was undertaken followed by field visits and setting up of versal integrated publicly funded primary healthcare a working group in order to identify, develop and adapt a in Qatar. -
Annual Report اﻟـــﺘـــﻘـــﺮﻳــــﺮ اﻟـــﺴـــﻨـــﻮي 2012 2012
AR • 2012 1 ANNUAL REPORT اﻟـــﺘـــﻘـــﺮﻳــــﺮ اﻟـــﺴـــﻨـــﻮي 2012 2012 Her Highness Sheikha Moza Bint Nasser, Chairperson of Qatar Foundation, receives a 10th anniversary gift from Alreem Al-Nabti and Mohammed Al Hajri. Our faculty, students and staff are tremendously proud to be playing an important role in the progress of our host nation. ANNUAL REPORT JULY 1, 2011 TO JUNE 30, 2012 Leadership Report 02 Joint Advisory Board 05 Education 07 Foundation Program and 19 Pre-Medical Education CONTENTS Clinical Care 27 Research 33 Global and Public Health 41 Student Life 47 Outreach 53 Statistics 58 AR • 2012 2 Leadership Report It gives me great pleasure to present to you this annual report on Weill Cornell Medical College in Qatar’s (WCMC-Q) progress and achievements over the past 12 months. At any moment, there are countless stories to be told about the efforts of students and medical educators, the work of distinguished researchers, the care rendered by physicians, and the connections this college has with its surrounding communities. What is shown in this report is just a small representation of how WCMC-Q is building a world-class medical college in Qatar. Since 2011, we have witnessed many exciting signs that our college is excelling in its tripartite mission of excellence in education, research and clinical care. Our five-year strategic plan was implemented in 2010, having been developed in the context of this tripartite mission and with full alignment to the goals of Qatar’s National Vision 2030. The plan provided a formal structure for us to define our aspirations in all of these areas.