Conservative Care Options for Work-Related Foot and Ankle Conditions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

OES Site Color Scheme 1
Nuisance Problems You will Grow to Love Thomas V Gocke, MS, ATC, PA-C, DFAAPA President & Founder Orthopaedic Educational Services, Inc. Boone, NC [email protected] www.orthoedu.com Orthopaedic Educational Services, Inc. © 2016 Orthopaedic Educational Services, Inc. all rights reserved. Faculty Disclosures • Orthopaedic Educational Services, Inc. Financial Intellectual Property No off label product discussions American Academy of Physician Assistants Financial PA Course Director, PA’s Guide to the MSK Galaxy Urgent Care Association of America Financial Intellectual Property Faculty, MSK Workshops Ferring Pharmaceuticals Consultant Orthopaedic Educational Services, Inc. © 2016 Orthopaedic Educational Services, Inc. all rights reserved. 2 LEARNING GOALS At the end of this sessions you will be able to: • Recognize nuisance conditions in the Upper Extremity • Recognize nuisance conditions in the Lower Extremity • Recognize common Pediatric Musculoskeletal nuisance problems • Recognize Radiographic changes associates with common MSK nuisance problems • Initiate treatment plans for a variety of MSK nuisance conditions Orthopaedic Educational Services, Inc. © 2016 Orthopaedic Educational Services, Inc. all rights reserved. Inflammatory Response Orthopaedic Educational Services, Inc. © 2016 Orthopaedic Educational Services, Inc. all rights reserved. Inflammatory Response* When does the Inflammatory response occur: • occurs when injury/infection triggers a non-specific immune response • causes proliferation of leukocytes and increase in blood flow secondary to trauma • increased blood flow brings polymorph-nuclear leukocytes (which facilitate removal of the injured cells/tissues), macrophages, and plasma proteins to injured tissues *Knight KL, Pain and Pain relief during Cryotherapy: Cryotherapy: Theory, Technique and Physiology, 1st edition, Chattanooga Corporation, Chattanooga, TN 1985, p 127-137 Orthopaedic Educational Services, Inc. © 2016 Orthopaedic Educational Services, Inc. -

Realignment Surgery As Alternative Treatment of Varus and Valgus Ankle Osteoarthritis
CLINICAL ORTHOPAEDICS AND RELATED RESEARCH Number 462, pp. 156–168 © 2007 Lippincott Williams & Wilkins Realignment Surgery as Alternative Treatment of Varus and Valgus Ankle Osteoarthritis Geert I. Pagenstert, MD*; Beat Hintermann, MD*; Alexej Barg, MD*; André Leumann, MD†; and Victor Valderrabano, MD, PhD† In patients with asymmetric (varus or valgus) ankle osteo- Level of Evidence: Level IV, therapeutic study. See the arthritis, realignment surgery is an alternative treatment to Guidelines for Authors for a complete description of levels of fusion or total ankle replacement in selected cases. To deter- evidence. mine whether realignment surgery in asymmetric ankle os- teoarthritis relieved pain and improved function, we clini- cally and radiographically followed 35 consecutive patients Surgical treatment for patients with symptomatic ankle with posttraumatic ankle osteoarthritis treated with lower osteoarthritis (OA) is controversial, particularly in me- leg and hindfoot realignment surgery. We further questioned if outcome correlated with achieved alignment. The average chanically induced, malaligned ankle OA in which joint patient age was 43 years (range, 26–68 years). We used a cartilage is partially preserved. These patients typically are standardized clinical and radiographic protocol. Besides dis- in their economically important, active middle ages be- tal tibial osteotomies, additional bony and soft tissue proce- cause early trauma is the predominant (70–80%) etiology dures were performed in 32 patients (91%). At mean fol- of their ankle OA.49,58 Currently, treatment recommenda- lowup of 5 years (range, 3–10.5 years), pain decreased by an tions after failed nonoperative therapy are polarized be- average of 4 points on a visual analog scale; range of ankle tween fusion2,11,33 and total ankle replacement motion increased by an average of 5°. -

Differential Diagnosis and Treatment of Iliotibial Band Pain Secondary to a Hypomobile Cuboid in a 24-Year-Old Female Tri-Athlete
INTERNATIONAL ACADEMY OF ORTHOPEDIC MEDICINE VOLUME 4, ISSUE 1 WINTER 2015/2016 Differential Diagnosis and Treatment of Iliotibial Band Pain Secondary to a Hypomobile Cuboid in a 24-Year-Old Female Tri-Athlete Femoroacetabular Impingement in the Adolescent Population: A Review Immediate Changes in Widespread Pressure Pain Sensitivity, Neck Pain, and Cervical Spine Range of Motion after Cervical or Thoracic Thrust Manipulation in Patients with Bilateral Chronic Mechanical Neck Pain: A Randomized Clinical Trial IAOM-US CONNECTION DIRECTORY is published by John Hoops PT, COMT The International Managing Editor Academy of Orthopedic Medicine-US (IAOM-US) Valerie Phelps PT, ScD, OCS, FAAOMPT PO Box 65179 Chief Editor / Education Director Tucson, AZ 85728 (p) 866.426.6101 Tanya Smith PT, ScD, FAAOMPT (f) 866.698.4832 Senior Editor (e) [email protected] (w) www.iaom-us.com John Woolf MS, PT, ATC, COMT Business Director CONTACT (p) 866.426.6101 Sharon Fitzgerald (f) 866.698.4832 Executive Assistant (e) [email protected] (w) www.iaom-us.com Andrea Cameron All trademarks are the property Administrative Assistant/ of their respective owners. Marketing Liaison The IAOM-US CONNECTION VOLUME 4 CONNECTION Differential Diagnosis and Dear Colleagues: Treatment of Iliotibial Band Pain Secondary to a Hypomobile Cuboid We hope you’ve had a happy and healthy 2015 2 in a 24-Year-Old Female Tri-Athlete and are ready to set your sights on 2016. Our 2016 course schedule is set, though we’re always adding new course locations and topics. If you haven’t had a chance to see what’s coming to your neck of the woods, here’s a link to the schedule. -

Imaging of the Bursae
Editor-in-Chief: Vikram S. Dogra, MD OPEN ACCESS Department of Imaging Sciences, University of HTML format Rochester Medical Center, Rochester, USA Journal of Clinical Imaging Science For entire Editorial Board visit : www.clinicalimagingscience.org/editorialboard.asp www.clinicalimagingscience.org PICTORIAL ESSAY Imaging of the Bursae Zameer Hirji, Jaspal S Hunjun, Hema N Choudur Department of Radiology, McMaster University, Canada Address for correspondence: Dr. Zameer Hirji, ABSTRACT Department of Radiology, McMaster University Medical Centre, 1200 When assessing joints with various imaging modalities, it is important to focus on Main Street West, Hamilton, Ontario the extraarticular soft tissues that may clinically mimic joint pathology. One such Canada L8N 3Z5 E-mail: [email protected] extraarticular structure is the bursa. Bursitis can clinically be misdiagnosed as joint-, tendon- or muscle-related pain. Pathological processes are often a result of inflammation that is secondary to excessive local friction, infection, arthritides or direct trauma. It is therefore important to understand the anatomy and pathology of the common bursae in the appendicular skeleton. The purpose of this pictorial essay is to characterize the clinically relevant bursae in the appendicular skeleton using diagrams and corresponding multimodality images, focusing on normal anatomy and common pathological processes that affect them. The aim is to familiarize Received : 13-03-2011 radiologists with the radiological features of bursitis. Accepted : 27-03-2011 Key words: Bursae, computed tomography, imaging, interventions, magnetic Published : 02-05-2011 resonance, ultrasound DOI : 10.4103/2156-7514.80374 INTRODUCTION from the adjacent joint. The walls of the bursa thicken as the bursal inflammation becomes longstanding. -

Ankle and Pantalar Arthrodesis
ANKLE AND PANTALAR ARTHRODESIS George E. Quill, Jr., M.D. In: Foot and Ankle Disorders Edited by Mark S. Myerson, M.D. Since reports in the late 19th Century, arthrodesis has been a successful accepted treatment method for painful disorders of the ankle, subtalar, and transverse tarsal joints. While the title of this chapter involves arthrodesis - the intentional fusion of a joint - as a form of reconstruction, this chapter will address not only surgical technique, but nonoperative methods of care as well. We will address the pathophysiology leading to ankle and hindfoot disability, succinctly review the existing literature on the topic of hindfoot and ankle arthrodesis, highlight the pathomechanics involved, and spend considerable time on establishing the diagnosis, indications, and preoperative planning when surgery is indicated. We also will discuss the rehabilitation of the postoperative patient, as well as the management of complications that may arise after ankle and pantalar arthrodesis. There are more than thirty different viable techniques that have been described in order to achieve successful ankle and hindfoot arthrodesis. It is not the purpose of this chapter to serve as compendium of all the techniques ever described. The author will, rather, attempt to distill into a useful amount of clinically applicable material this vast body of information that the literature and clinical experience provide. Ankle arthrodesis is defined as surgical fusion of the tibia to the talus. Surgical fusion of the ankle (tibiotalar) and subtalar (talocalcaneal) joints at the same operative sitting is termed tibiotalocalcaneal arthrodesis. Fusion of the talus to all the bones articulating with it (distal tibia, calcaneus, navicular, and cuboid) is termed pantalar arthrodesis. -

Multimodal Physical Therapy Management of a 24 Year-Old Male with Chronic Retrocalcaneal Pain: a Case Report Matthew Eh Rring Governors State University
Governors State University OPUS Open Portal to University Scholarship All Capstone Projects Student Capstone Projects Spring 2015 Multimodal Physical Therapy Management of a 24 Year-Old Male with Chronic Retrocalcaneal Pain: A Case Report Matthew eH rring Governors State University Follow this and additional works at: http://opus.govst.edu/capstones Part of the Physical Therapy Commons Recommended Citation Herring, Matthew, "Multimodal Physical Therapy Management of a 24 Year-Old Male with Chronic Retrocalcaneal Pain: A Case Report" (2015). All Capstone Projects. 124. http://opus.govst.edu/capstones/124 For more information about the academic degree, extended learning, and certificate programs of Governors State University, go to http://www.govst.edu/Academics/Degree_Programs_and_Certifications/ Visit the Governors State Physical Therapy Department This Project Summary is brought to you for free and open access by the Student Capstone Projects at OPUS Open Portal to University Scholarship. It has been accepted for inclusion in All Capstone Projects by an authorized administrator of OPUS Open Portal to University Scholarship. For more information, please contact [email protected]. MULTIMODAL PHYSICAL THERAPY MANAGEMENT OF A 24 YEAR-OLD MALE WITH CHRONIC RETROCALCANEAL PAIN: A CASE REPORT By Matthew Herring B.S., Lewis University, 2006 Capstone Project Submitted in partial fulfillment of the requirements For the Degree of Doctor of Physical Therapy Governors State University University Park, IL 60484 2015 ABSTRACT Background and Purpose: The multimodal approach reflects the type of individualized treatment commonly used in the clinical setting, in which many different interventions are available to the physical therapist. The purpose of this case report is to describe the physical therapy management process for a patient with chronic retrocalcaneal pain using a multimodal intervention approach. -
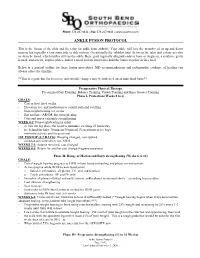
Ankle Fusion Protocol
Phone: 574.247.9441 ● Fax: 574.247.9442 ● www.sbortho.com ANKLE FUSION PROTOCOL This is the fusion of the tibia and the talus for ankle joint arthritis. Your ankle will lose the majority of its up and down motion, but typically retain some side to side motion. Occasionally the subtalar joint (between the talus and calcaneus) also needs to be fused, which further stiffens the ankle. Bone graft (typically allograft/cadaver bone or Augment, a synthetic graft) is used, and screws, staples, plates, and/or a metal rod are inserted to hold the bones together as they heal. Below is a general outline for these fusion procedures. MD recommendations and radiographic evidence of healing can always affect the timeline. **This is a guideline for recovery, and specific changes may be indicated on an individual basis** Preoperative Physical Therapy Pre surgical Gait Training, Balance Training, Crutch Training and Knee Scooter Training Phase I- Protection (Weeks 0 to 6) GOALS: - Cast or boot for 6 weeks - Elevation, ice, and medication to control pain and swelling - Non-weight bearing x 6 weeks - Hip and knee AROM, hip strengthening - Core and upper extremity strengthening WEEK 0-2: Nonweightbearing in splint - elevate the leg above the heart to minimize swelling 23 hours/day - ice behind the knee 30 min on/30 min off (Vascutherm or ice bag) - minimize activity and focus on rest 1ST POSTOP (5-7 DAYS): Dressing changed, cast applied - continue strict elevation, ice, NWB WEEKS 2-3: Sutures removed, cast changed WEEKS 4-5: Return for another cast change -
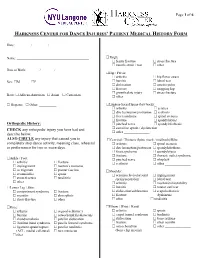
Harkness Center for Dance Injuries' Patient Medical History Form
Page 1 of 6 HARKNESS CENTER FOR DANCE INJURIES’ PATIENT MEDICAL HISTORY FORM Date: ________ / ________ / ________ Name: __________________________________________ Thigh: femur fracture stress fracture muscle strain / tear other_______________ Date of Birth: _______ / _______ / _______ Hip / Pelvis: arthritis hip flexor strain Sex: M F bursitis labral tear dislocation osteitis pubis fracture snapping hip growth plate injury stress fracture Race: African-American Asian Caucasian other _______________ Hispanic Other: __________ Lumbar-Sacral Spine (low back): arthritis sciatica disc herniation/protrusion scoliosis facet syndrome spinal stenosis fracture spondylolysis Orthopedic History: pinched nerve spondylolisthesis CHECK any orthopedic injury you have had and sacroiliac sprain / dysfunction other _______________ describe below. ALSO CIRCLE any injury that caused you to Cervical / Thoracic Spine (neck / mid back)/Ribs: completely stop dance activity, meaning class, rehearsal arthritis spinal stenosis or performance for two or more days. disc herniation/protrusion spondylolisthesis facet syndrome spondylolysis fracture thoracic outlet syndrome Ankle / Foot: pinched nerve whiplash arthritis fracture scoliosis other _______________ impingement morton’s neuroma os trigonum plantar fasciitis Shoulder: sesamoiditis sprain acromioclavicular joint impingement stress fracture tendinitis sprain/separation labral tear other________________ arthritis mechanical instability Lower Leg / Shin: -

ESSR 2013 | 1 2 | ESSR 2013 Essrsport 2013 Injuries Musculoskeletal Radiology June 13–15, MARBELLA/SPAIN
Final Programme property of Marbella City Council ESSRSport 2013 Injuries MUSCULOSKELETAL RADIOLOGY JUNE 13–15, MARBELLA/SPAIN ESSRSport 2013 Injuries MUSCULOSKELETAL RADIOLOGY JUNE 13–15, MARBELLA/SPAIN Content 3 Welcome 4–5 ESSR Committee & Invited Speakers 6 General Information 11/13 Programme Overview ESSR 2013 | 1 2 | ESSR 2013 ESSRSport 2013 Injuries MUSCULOSKELETAL RADIOLOGY JUNE 13–15, MARBELLA/SPAIN from the ESSR 2013 Congress President ME Welcome LCO On behalf of the ESSR it is a pleasure to invite you to participate in the 20th Annual Scientific Meeting WE of the European Skeletal Society to be held in Marbella, Spain, on June 13–15, 2013, at the Palacio de Congresos located in the center of the city. The scientific programme will focus on “Sports Lesions”, with a refresher course lasting two days dedicated to actualised topics. The programme will include focus sessions and hot topics, as well as different sessions of the subcommittees of the society. There will be a special session on Interventional Strategies in Sports Injuries. The popular “hands on” ultrasound workshops in MSK ultrasound will be held on Thursday 13, 2013, during the afternoon, with the topic of Sports Lesions. Basic and advanced levels will be offered. A state-of-the-art technical exhibition will display the most advanced technical developments in the area of musculoskeletal pathology. The main lobby will be available for workstations for the EPOS as well as technical exhibits. Marbella is located in the south of Spain, full of life and with plenty of cultural and tourist interest, with architectural treasures of the traditional and popular Andalusian culture. -

Cuboid Syndrome in a College Basketball Player: a Case Report
CASE REVIEW Joseph J. Piccininni, Report Editor Cuboid Syndrome in a College Basketball Player: A Case Report Stephanie M. Mazerolle, PhD, ATC • University of Connecticut UBOID SYNDROME is a condition involv- Table 1. Clinical Presentation ing some degree of disruption of the of Cuboid Subluxation C normal structural congruity of the calca- • No edema or discoloration neo-cuboid (CC) joint.1-3 The condition is associated with several clinical terms for • Pain that may radiate to heel, mimicking heel spur midfoot pathology, including cuboid fault syndrome, pain dropped cuboid, subluxed cuboid, and lateral plantar • May or may not present with palpable defect in neuritis. The literature suggests that cuboid subluxation plantar fascia is associated with a lateral ankle sprain mechanism, • Point tenderness at calcaneo-cuboid joint and styloid occurring most often with a combination of inversion process of 5th metatarsal and plantar flexion.4 The inversion ankle sprain is the • Inability to “work through” the pain during the push- most common athletic injury, which accounts for 10- off phase of the gait cycle 15% of all sport participation time lost to injury.5 • Increased pain with stair climbing 1 Cuboid subluxations and dislocations are rare. The • Increased pain with side-to-side movements or majority of such cases reported in the literature have lateral movements involved long distance runners and ballet dancers.1,4 CC joint dysfunction following a traumatic episode usually results from a dislocation or subluxation injury, but lateral aspect of the foot. She reported having expe- foot pain and chronic instability of the lateral column rienced a traumatic episode three weeks earlier. -

Patient Medical History Form
Date of Visit: ________ / ________ / ________ ID # (R=Research) +MR# Patient Medical History Form Name: __________________________________________ Knee: arthritis osgood-schlatter’s Date of Birth: _______ / _______ / _______ Sex: M F bursitis osteochondritis dissecans Social Security ______-_____-________ chondromalacia patellar dislocation iliotibial band syndrome patella femoral syndrome Race: African-American Asian Caucasian ligament sprain/rupture patellar tendinitis Hispanic Other: __________ (ACL, medial collateral) torn meniscus other________________ Address:___________________________________________ ______________________________________________ Thigh: femur fracture stress fracture City: _________________ State: _______ ZIP: ________ muscle strain / tear other_______________ Primary Phone: _______ - ________ - __________ Hip / Pelvis: Email: ___________________________________________ arthritis hip flexor strain bursitis labral tear Emergency Contact Information: dislocation osteitis pubis Name: ___________________________________________ fracture snapping hip growth plate injury stress fracture Relation: ______________ Phone:_____________________ other _______________ Health Insurance Information: Lumbar-Sacral Spine (low back): Name of Insurance Co: _____________________________ arthritis sciatica Name of Policy Holder: _____________________________ disc herniation/protrusion scoliosis facet syndrome spinal stenosis Policy #: _________________ Group#: ________________ fracture spondylolsysis -

Management Strategies for Cuboid Syndrome
CASE REVIEW Joe J. Piccininni, EdD, CAT(C) Management Strategies for Cuboid Syndrome Jennifer L. Roney, MS, ATC • University of Utah; Melissa L. Yamashiro, ATC • Orthopedic Specialty Group; and Charlie A. Hicks-Little, PhD, ATC • University of Utah Cuboid syndrome refers to a subluxation and Woodle3 reported that nearly all cases of the cuboid or calcaneo-cuboid joint dys- of cuboid syndrome were associated with function.1,2 Cuboid syndrome only accounts pes planus. Pronation of the subtalar joint for 4% of sports-related foot injuries, but provides the peroneal longus muscle with a represents 17% of foot injuries among ballet greater mechanical advantage.5 The intrinsic dancers.2,3 The purpose of this report is to foot muscles, predominantly the flexors, are present an effective management strategy believed to play an important role in stabiliz- for cuboid syndrome. ing the transverse tarsal joint during gait.4 The stability of the Current conservative management of Key PointsPoints articulation between the cuboid syndrome includes manual therapy, Cuboid syndrome is rarely found in ath- cuboid and the distal taping, padding, and use of an orthosis.5-10 letes, other than ballet dancers. portion of the calca- Newell and Woodle3 described a cuboid neus is maintained by manipulation technique that was later Current management options include a number of ligaments referred to as the “black snake heel whip.”1 manual techniques, taping, padding, and and a joint capsule. The patient stands with the affected leg in orthotics. The peroneus longus a knee-flexed, non-weight-bearing position. tendon runs through The clinician grasps the forefoot, placing the The “four mini-stirrup” taping can help the peroneal groove on thumbs on the plantar aspect of the cuboid manage cuboid syndrome.