Resuscitation Skills – Part Three Basic Airway Management
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ABCDE Approach
The ABCDE and SAMPLE History Approach Basic Emergency Care Course Objectives • List the hazards that must be considered when approaching an ill or injured person • List the elements to approaching an ill or injured person safely • List the components of the systematic ABCDE approach to emergency patients • Assess an airway • Explain when to use airway devices • Explain when advanced airway management is needed • Assess breathing • Explain when to assist breathing • Assess fluid status (circulation) • Provide appropriate fluid resuscitation • Describe the critical ABCDE actions • List the elements of a SAMPLE history • Perform a relevant SAMPLE history. Essential skills • Assessing ABCDE • Needle-decompression for tension • Cervical spine immobilization pneumothorax • • Full spine immobilization Three-sided dressing for chest wound • • Head-tilt and chin-life/jaw thrust Intravenous (IV) line placement • • Airway suctioning IV fluid resuscitation • • Management of choking Direct pressure/ deep wound packing for haemorrhage control • Recovery position • Tourniquet for haemorrhage control • Nasopharyngeal (NPA) and oropharyngeal • airway (OPA) placement Pelvic binding • • Bag-valve-mask ventilation Wound management • • Skin pinch test Fracture immobilization • • AVPU (alert, voice, pain, unresponsive) Snake bite management assessment • Glucose administration Why the ABCDE approach? • Approach every patient in a systematic way • Recognize life-threatening conditions early • DO most critical interventions first - fix problems before moving on -
TCCC CLS Skill Instructions Mod 7 25 JAN 20
MODULE 07: AIRWAY MANAGEMENT IN TFC SKILL INSTRUCTIONS 25 JAN 2020 COMBAT LIFESAVER (CLS) TACTICAL COMBAT CASUALTY CARE SKILL INSTRUCTIONS HEAD-TILT/CHIN-LIFT INSTRUCTION TASK: Open an airway using the head-tilt/chin-lift maneuver CONDITION: Given a simulated scenario where a casualty and responder are in combat gear and the casualty is unconscious without a patent airway STANDARD: EffeCtively open the airway by performing the head-tilt/chin-lift maneuver following all steps and measures correctly without Causing further harm to the Casualty EQUIPMENT: N/A PERFORMANCE MEASURES: step-by-step instructions NOTE: Do not use if a spinal or neck injury is suspected. 01 Roll the Casualty onto their back, if necessary, and place them on a hard, flat surface. 02 Kneel at the level of the Casualty’s shoulders. Position yourself at the side of the Casualty. 03 Open the mouth and looK for visible airway obstruCtions (e.g., laCerations, obstructions, broken teeth, burns, or swelling or other debris, such as vomit). NOTE: If foreign material or vomit is in the mouth, remove it as quiCKly as possible. NOTE: Do not perform a blind finger sweep. 04 PlaCe one hand on the Casualty's forehead and apply firm, backward pressure with the palm to tilt the head back. 05 PlaCe the fingertips of the other hand under the bony part of the lower jaw and lift, bringing the Chin forward. NOTE: Do not use the thumb to lift the chin. 06 While maintaining the open airway position, place an ear over the casualty's mouth and nose, looking toward the chest and stomaCh. -

Tracheal Intubation Following Traumatic Injury)
CLINICAL MANAGEMENT UPDATE The Journal of TRAUMA Injury, Infection, and Critical Care Guidelines for Emergency Tracheal Intubation Immediately after Traumatic Injury C. Michael Dunham, MD, Robert D. Barraco, MD, David E. Clark, MD, Brian J. Daley, MD, Frank E. Davis III, MD, Michael A. Gibbs, MD, Thomas Knuth, MD, Peter B. Letarte, MD, Fred A. Luchette, MD, Laurel Omert, MD, Leonard J. Weireter, MD, and Charles E. Wiles III, MD for the EAST Practice Management Guidelines Work Group J Trauma. 2003;55:162–179. REFERRALS TO THE EAST WEB SITE and impaired laryngeal reflexes are nonhypercarbic hypox- Because of the large size of the guidelines, specific emia and aspiration, respectively. Airway obstruction can sections have been deleted from this article, but are available occur with cervical spine injury, severe cognitive impairment on the Eastern Association for the Surgery of Trauma (EAST) (Glasgow Coma Scale [GCS] score Յ 8), severe neck injury, Web site (www.east.org/trauma practice guidelines/Emergency severe maxillofacial injury, or smoke inhalation. Hypoventi- Tracheal Intubation Following Traumatic Injury). lation can be found with airway obstruction, cardiac arrest, severe cognitive impairment, or cervical spinal cord injury. I. STATEMENT OF THE PROBLEM Aspiration is likely to occur with cardiac arrest, severe cog- ypoxia and obstruction of the airway are linked to nitive impairment, or severe maxillofacial injury. A major preventable and potentially preventable acute trauma clinical concern with thoracic injury is the development of Hdeaths.1–4 There is substantial documentation that hyp- nonhypercarbic hypoxemia. Lung injury and nonhypercarbic oxia is common in severe brain injury and worsens neuro- hypoxemia are also potential sequelae of aspiration. -

Airway – Oropharyngeal: Insertion; Maintenance; Suction; Removal
Policies & Procedures Title: AIRWAY – OROPHARYNGEAL: INSERTION; MAINTENANCE; SUCTION; REMOVAL I.D. Number: 1159 Authorization Source: Nursing Date Revised: September 2014 [X] SHR Nursing Practice Committee Date Effective: October 2002 Date Reaffirmed: January 2016 Scope: SHR Acute, Parkridge Centre Any PRINTED version of this document is only accurate up to the date of printing 30-May-16. Saskatoon Health Region (SHR) cannot guarantee the currency or accuracy of any printed policy. Always refer to the Policies and Procedures site for the most current versions of documents in effect. SHR accepts no responsibility for use of this material by any person or organization not associated with SHR. No part of this document may be reproduced in any form for publication without permission of SHR. 1. PURPOSE 1.1 To safely and effectively use Oropharyngeal Airway (OPA). 2. POLICY 2.1 The Registered Nurse (RN), Registered Psychiatric Nurse (RPN), Licensed Practical Nurse (LPN), Graduate Nurse (GN), Graduate Psychiatric Nurse (GPN), Graduate Licensed Practical Nurse (GLPN) will insert, maintain, suction and remove an oropharyngeal airway (OPA). 2.2 The OPA may be inserted to establish and assist in maintaining a patent airway. 2.3 An OPA should only be used in patients with decreased level of consciousness or decreased gag reflex. 2.4 Patients with OPAs that have been inserted for airway protection should not be left unattended due to risk of aspiration if gag reflex returns unexpectedly. Page 1 of 4 Policies and Procedures: Airway – Oropharyngeal: Insertion; Maintenance; I.D. # 1159 Suction; Removal 3. PROCEDURE 3.1 Equipment: • Oropharyngeal airway of appropriate size • Tongue blade (optional) • Clean gloves • Optional: suction equipment, bag-valve-mask device 3.2 Estimate the appropriate size of airway by aligning the tube on the side of the patient’s face parallel to the teeth and choosing an airway that extends from the ear lobe to the corner of the mouth. -
Scope of Practice Statements
Scope of Practice Statements Emergency Medical Services Authority California Health and Human Services Agency EMSA # 300 November 2017 HOWARD BACKER, MD, MPH, FACEP DIRECTOR DANIEL R. SMILEY CHIEF DEPUTY DIRECTOR SEAN TRASK DIVISION CHIEF EMSA # 300 Released November 2017 EMSA #300 • Page 1 Table of Contents Introduction ........................................................................................................................................... 4 The EMS Authority ................................................................................................................................ 4 Local EMS Agencies ............................................................................................................................. 4 California EMS Personnel Levels .......................................................................................................... 4 Reading the Scope of Practice Pages .................................................................................................. 5 Airway and Breathing ............................................................................................................................ 6 Airway Suctioning .............................................................................................................................. 7 Automatic Transport Ventilator .......................................................................................................... 8 Bag Valve Mask – BVM .................................................................................................................... -

Airway Management for COVID 19
Airway Management in Critically Ill COVID-19 Patients KATHERINE HELLER, MD ASSISTANT PROFESSOR UNIVERSITY OF WASHINGTON SCHOOL OF MEDICINE DEPARTMENT OF ANESTHESIOLOGY MEDICAL DIRECTOR: UWMC SICU Disclosures (none) Outline Staff safety PPE Patient factors/ timing Adjuncts for oxygenation Intubation procedure Preparation Equipment/technique Unusual situations Difficult airways Tracheostomy Emergencies Opening Questions Please navigate to pollev.com/katherinehel603 Priorities Priority #1: Staff Safety Considerations for Staff Procedural planning Appropriate PPE takes time Avoid emergencies when able Consider rounding (remotely?) on known COVID patients PPE Any airway management is an Aerosol Generating Procedure (AGP) Need respirator level protections airborne + contact/droplet N95 vs PAPR N95 PAPR Pro Pro Easy to don Comfortable Fast Protect face, neck, head Allow use of stethoscope Reusable More readily available Con Con Allows contamination of Require power source face and neck Need assistance to don Less comfortable and doff May not fit everyone Noisy Fit can change Infection Control Choose what work for you and your institution More important to have clear protocols and expectations Minimize in room staff Have equipment easily available Filter in line on circuit Infection control Barrier Devices Not recommended Additional encumbrance to intubation without proven benefit Not a replacement for PPE May actually increase risk [11] Failed airway Breach of PPE FDA revoked EUA for barrier devices in -
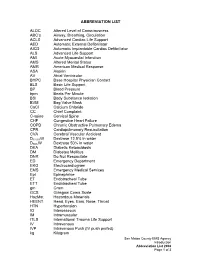
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC's Airway, Breathing, Circulation ACLS Advanced Cardiac Life Suppo
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC’s Airway, Breathing, Circulation ACLS Advanced Cardiac Life Support AED Automatic External Defibrillator AICD Automatic Implantable Cardiac Defibrillator ALS Advanced Life Support AMI Acute Myocardial Infarction AMS Altered Mental Status AMR American Medical Response ASA Aspirin AV Atrial Ventricular BHPC Base Hospital Physician Contact BLS Basic Life Support BP Blood Pressure bpm Beats Per Minute BSI Body Substance Isolation BVM Bag Valve Mask CaCl Calcium Chloride CC Chief Complaint C-spine Cervical Spine CHF Congestive Heart Failure COPD Chronic Obstructive Pulmonary Edema CPR Cardiopulmonary Resuscitation CVA Cerebral Vascular Accident D12.5%W Dextrose 12.5% in water D50%W Dextrose 50% in water DKA Diabetic Ketoacidosis DM Diabetes Mellitus DNR Do Not Resuscitate ED Emergency Department EKG Electrocardiogram EMS Emergency Medical Services Epi Epinephrine ET Endotracheal Tube ETT Endotracheal Tube gm Gram GCS Glasgow Coma Scale HazMat Hazardous Materials HEENT Head, Eyes, Ears, Nose, Throat HTN Hypertension IO Interosseous IM Intramuscular ITLS International Trauma Life Support IV Intravenous IVP Intravenous Push (IV push prefed) kg Kilogram San Mateo County EMS Agency Introduction Abbreviation List 2008 Page 1 of 3 J Joule LOC Loss of Consciousness Max Maximum mcg Microgram meds Medication mEq Milliequivalent min Minute mg Milligram MI Myocardial Infarction mL Milliliter MVC Motor Vehicle Collision NPA Nasopharyngeal Airway NPO Nothing Per Mouth NS Normal Saline NT Nasal Tube NTG Nitroglycerine NS Normal Saline O2 Oxygen OB Obstetrical OD Overdose OPA Oropharyngeal Airway OPQRST Onset, Provoked, Quality, Region and Radiation, Severity, Time OTC Over the Counter PAC Premature Atrial Contraction PALS Pediatric Advanced Life Support PEA Pulseless Electrical Activity PHTLS Prehospital Trauma Life Support PID Pelvic Inflammatory Disease PO By Mouth Pt. -

Developing an Airway Management Bundle to Standardize Emergent
It Takes A Village: Developing an Airway Management Bundle to Standardize Emergent Intubation Processes in the Emergency Department James Sacca, MD, Daniel Casey Kim, MD, Dimitri Papanagnou, MD, MPH, EdD(c) Department of Emergency Medicine, Thomas Jefferson University Hospital 1. Crash Airway Pre-medicate: Glycopyrrolate: 0.2 mg RSI TIME OUT If patient arrives without airway device present Ondansetron: 4 mg Pre-oxygenate and prepare for immediate intubation Nebulized or atomized Lidocaine: Patient Name__________________________________ If patient arrives with supraglottic device present 4 ml of 4% or 8 ml of 2% Needs Assessment Strategy #2 TJUH AIRWAY BUNDLE Problem Definition If able to oxygenate and ventilate, delay intubation Sedation: Code status permits intubation: Y or N or Unknown If patient arrives with ETT present Ketamine: 1 mg/kg bolus NPO since__________________ Confirm ETT placement (see 5.) Consider paralytic once successful Unconscious, Consider visualization with laryngoscopy Allergies______________________________ or NKDA Unreactive, D. Delayed sequence intubation 2. RSI Patient delirious/agitated so can’t pre-oxygenate We performed a FMEA to uncover latent threats through in situ Height___________________ Near death? Pre-medicate: Mallampati score_____________ Pretreatment: Glycopyrrolate: 0.2 mg Yes No For reactive airway disease: Lidocaine 1.5 mg/kg IV Ondansetron: 4 mg [ ] dentures removed Yes Airway management is at the core of emergent patient care. Emergent 1 For cardiovascular disease: Fentanyl 3 mcg/kg Sedation: simulation, as well as real patient intubations. A in situ simulation of Crash airway Difficult airway? For elevated ICP: both of the above meds/doses Ketamine: 1.5 mg/kg IBW bolus Personnel Pre-oxygenate No Induction: Paralyze intubations in the Emergency Department (ED) at Thomas Jefferson 1. -

Best Airway and Ventilation Strategy During CPR and After Resuscitation
Best airway and ventilation strategy during CPR and after resuscitation After cardiac arrest a combination of basic and advanced airway and ventilation techniques are used during cardiopulmonary resuscitation (CPR) and after a return of spontaneous circulation (ROSC). Current guidelines are based predominantly on evidence from observational studies and expert consensus; thus, the optimal combination of airway techniques and oxygen and ventilation targets during CPR and after ROSC is uncertain, according to a review article in the journal Critical Care. Current evidence supports a stepwise approach to airway management based on patient factors, rescuer skills and the stage of resuscitation. Observational data suggest that early lay-bystander compression-only CPR can improve survival after sudden cardiac arrest. Chest compressions are easy to learn and do for most rescuers and do not require special equipment. Studies show that lay rescuer compression-only CPR is better than no CPR. During CPR, airway interventions range from compression-only CPR with or without airway opening, mouth-to-mouth ventilation, mouth-to-mask ventilation, bag-mask ventilation (with or without an oropharyngeal airway) or advanced airways (supraglottic airways [SGAs] and tracheal intubation using direct or video laryngoscopy). On arrival of trained rescuers, bag-mask ventilation with supplemental oxygen is the most common initial approach and can be aided with an oropharyngeal or nasopharyngeal airway. During CPR, the bag-mask is used to give two breaths after every 30 compressions. A pre-specified per-protocol analysis reported a significantly higher survival to discharge among those who actually received conventional CPR (30:2) compared with those who received continuous compressions. -

Importance of Validation Risk Prediction Tools
Art: toc Input-citi 22:40 12/2/7 12؍balt6/z7i-anesth/z7i-anesth/z7i00812/contents panickes S ON THE COVER: David Mackey, M.D., has organized a fascinating series of commentaries by national leaders In this issue of ANESTHESIOLOGY, two original research articles and three editorial views examine in the construction and use of clinical data registries by regulatory agencies and physician the use of data in clinical decision making. practices, the first two of which appear in this month’s issue: ● Kheterpal et al.: Impact of a Novel Multiparameter Decision Support System on Intraoperative ● Mackey: Can We Finally Conquer the Problem of Medical Quality? The Systems-based Processes of Care and Postoperative Outcomes, p. 272 Opportunities of Data Registries and Medical Teamwork, p. 225 ● Liu et al.: Defining the Intrinsic Cardiac Risks of Operations to Improve Preoperative Cardiac ● Jain et al.: A Public-Private Strategy to Advance the Use of Clinical Registries, p. 227 Risk Assessments, p. 283 Downloaded from http://pubs.asahq.org/anesthesiology/article-pdf/128/2/A1/364553/20180200_0-00001.pdf by guest on 01 October 2021 ● Sessler: Decision Support Alerts: Importance of Validation, p. 241 ● Glance et al.: Risk Prediction Tools: The Need for Greater Transparency, p. 244 ● Javitt: Regulatory Landscape for Clinical Decision Support Technology, p. 247 ᭛ THIS MONTH IN ANESTHESIOLOGY 9A ᭛◆ THISEDITORIAL MONTH VIEWS IN ANESTHESIOLOGY 1A . Can We Finally Conquer the Problem of Medical Quality? The Systems-based ◼ SCIENCE, MEDICINE, AND THE ANESTHESIOLOGIST 15A Opportunities of Data Registries and Medical Teamwork 225 David C. Mackey ◼ INFOGRAPHICS IN ANESTHESIOLOGY 19A . A Public-Private Strategy to Advance the Use of Clinical Registries 227 Sachin H. -
RN to EMT-Basic Transition Course
State of Wisconsin Registered Nurse to EMT-Basic Transition Course November 2010 Wisconsin EMS Section State of Wisconsin RN to EMT-Basic Transition Course TABLE OF CONTENTS Introduction .....................................................................................................iv List of Appendices...........................................................................................vi Module 1 – Preparatory 1-1 Introduction to Emergency Care .................................................. 1-1 1-2 Well-Being of the EMT Basic ....................................................... 1-6 1-3 Medical/Legal and Ethical Issues............................................... 1-12 1-5 Lifting and Moving Patients........................................................ 1-16 1-6 Evaluation .................................................................................. 1-25 Module 2 - Patient Assessment 2-1 Scene Size-up ............................................................................. 2-1 2-2 Initial Assessment........................................................................ 2-6 2-3 Baseline Vital Signs, SAMPLE History and the Use of Pulse Oximetry .......................................................................... 2-11 2-4 Focused History and Physical Exam: Trauma ........................... 2-16 2-5 Focused History and Physical Exam: Medical ........................... 2-22 2-6 Detailed Physical Exam ............................................................. 2-27 2-7 On-Going Assessment.............................................................. -
Brevital Sodium Methohexital Sodium for Injection
BREVITAL® SODIUM METHOHEXITAL SODIUM FOR INJECTION, USP For Intravenous Use in Adults For Rectal and Intramuscular Use Only in Pediatric Patients WARNING Brevital should be used only in hospital or ambulatory care settings that provide for continuous monitoring of respiratory (e.g. pulse oximetry) and cardiac function. Immediate availability of resuscitative drugs and age- and size-appropriate equipment for bag/valve/mask ventilation and intubation and personnel trained in their use and skilled in airway management should be assured. For deeply sedated patients, a designated individual other than the practitioner performing the procedure should be present to continuously monitor the patient. (See WARNINGS) DESCRIPTION Brevital® Sodium (Methohexital Sodium for Injection, USP) is 2,4,6 (1H, 3H, 5H)- Pyrimidinetrione, 1-methyl-5-(1-methyl-2-pentynyl)-5-(2-propenyl)-, (±)-, monosodium salt and has the empirical formula C14H17N2NaO3. Its molecular weight is 284.29. The structural formula is as follows: Methohexital sodium is a rapid, ultrashort-acting barbiturate anesthetic. Methohexital sodium for injection is a freeze-dried, sterile, nonpyrogenic mixture of methohexital sodium with 6% anhydrous sodium carbonate added as a buffer. It contains not less than 90% and not more than 110% of the labeled amount of methohexital sodium. It occurs as a white, freeze-dried plug that is freely soluble in water. This product is oxygen sensitive. The pH of the 1% solution is between 10 and 11; the pH of the 0.2% solution in 5% dextrose is between 9.5 and 10.5. Methohexital sodium may be administered by direct intravenous injection or continuous intravenous drip, intramuscular or rectal routes (see PRECAUTIONS—Pediatric Use).