'Burp' (1) Worsens Glottic View When Applied to the Cricoid
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hemodynamically Unstable/ Shocked Patient in OR. Challenge For
Journal of Anesthesia & Critical Care: Open Access Opinion Open Access Hemodynamically unstable/ shocked patient in OR challenge for teamwork efficacy when time is critical Volume 7 Issue 4 - 2017 Dimosthenis Petsas,1 Yasir Othman AT,1 Marton Hannus,1 Eljona Cumashi2 Opinion 1Anaesthetics Department, HMG Hospital, UAE 2OB/GYNAE Department, HMG Hospital, UAE In the present article we present a case report with comments/ suggestions about team dynamics. The emergency case report is only Correspondence: Dimosthenis Petsas, Anaesthetics used to highlight the importance of teamwork dynamics and many Department, HMG Hospital Dubai, Dubai Healthcare City, Building 57, UAE, PO BOX 505005, Tel 00306972008383, clinical details are not mentioned. Treating a hemodynamically Email unstable/shocked patient can be a challenging procedure and requires perfect teamwork to have the best possible outcome. Reviewing Received: March 10, 2017 | Published: March 15, 2017 the present case report we should always keep in mind that the organization is a private hospital with all the differences in resources compared to a large public hospital. A 33-year old female patient presented to ER department with signs of circulatory shock (low blood pressure, tachycardia, drowsiness and clumsy sweaty skin). Her vital signs were BP=75/35 mmHg, HR ranging from 120-135 bpm, temperature was 35.9 Celsius, pale skin and drowsiness. Initial resuscitation in ER included administration of Table 2 Intraoperative hemoglobin and coagulation 2 liters IV ringers lactate and oxygen through face mask at 5-6 lt/ min. There was temporary improvement of vital signs. Bloods were sent Investigation Value for complete blood count, coagulation, biochemistry. -

Femoral Nerve Block Versus Spinal Anesthesia for Lower Limb
Alexandria Journal of Anaesthesia and Intensive Care 44 Femoral Nerve Block versus Spinal Anesthesia for Lower Limb Peripheral Vascular Surgery By Ahmed Mansour, MD Assistant Professor of Anesthesia, Faculty of Medicine, Alexandria University. Abstract Perioperative cardiac complications occur in 4% to 6% of patients undergoing infrainguinal revascularization under general, spinal, or epidural anesthesia. The risk may be even greater in patients whose cardiac disease cannot be fully evaluated or treated before urgent limb salvage operations. Prompted by these considerations, we investigated the feasibility and results of using femoral nerve block with infiltration of the genito4femoral nerve branches in these high-risk patients. Methods: Forty peripheral vascular reconstruction of lower limbs were performed under either spinal anesthesia (20 patients) or femoral nerve block with infiltration of genito-femoral nerve branches supplemented with local infiltration at the site of dissection as needed (20 patients). All patients had arterial lines. Arterial blood pressure and electrocardiographic monitoring was continued during surgery, in PACU and in the intensive care units. Results: Operations included femoral-femoral, femoral-popliteal bypass grafting and thrombectomy. The intra-operative events showed that the mean time needed to perform the block and dose of analgesics and sedatives needed during surgery was greater in group I (FNB,) compared to group II [P=0.01*, P0.029* , P0.039*], however, the time needed to start surgery was shorter in group I than in group II [P=0. 039]. There were no block failures in either group, but local infiltration in the area of the dissection with 2 ml (range 1-5 ml) of 1% lidocaine was required in 4 (20%) patients in FNB group vs none in the spinal group. -
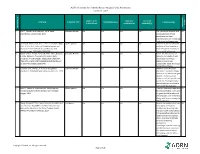
AORN Guideline for Patients Receiving Local-Only Anesthesia Evidence Table
AORN Guideline for Patients Receiving Local-Only Anesthesia Evidence Table SAMPLE SIZE/ CONTROL/ OUTCOME CITATION EVIDENCE TYPE INTERVENTION(S) CONCLUSION(S) POPULATION COMPARISON MEASURE(S) SCORE CONSENSUS REFERENCE # REFERENCE 1 Lirk P., Picardi S. and Hollmann, M. W. Local Literature Review n/a n/a n/a n/a The mechanism of action and VA anaesthetics: 10 essentials. 2014 access pathways of local anesthetics and their pharmokinetics are increasingly understood and appreciated. 2 Calatayud, Jesús, M.D.,D.D.S., Ph.D., González, Õngel, Expert Opinion n/a n/a n/a n/a A review of the discovery and VA M.D., D.D.S., Ph.D. History of the development and evolution of local anesthesia evolution of local anesthesia since the coca leaf. from the Spanish discovery of Anesthesiology. 2003;98(6):1503-1508. the coca leaf in America. 3 Gordh T, M.D., Gordh, Torsten E.,M.D., Ph.D., Lindqvist Literature Review n/a n/a n/a n/a Before the introduction of VA K, M.Sc. Lidocaine: The origin of a modern local lidocaine, the choice of local anesthetic. Anesthesiology. 2010;113(6):1433-1437. anesthetics was limited. https://doi.org/10.1097/ALN.0b013e3181fcef48. doi: Lidocaine's onset was 10.1097/ALN.0b013e3181fcef48. substantially faster and longer lasting than procaine. 4 Volcheck G.W., Mertes, P. M. Local and general Literature Review n/a n/a n/a n/a Whether to test the local VA anesthetics immediate hypersensitivity reactions. 2014 anesthetic causing the allergic reaction or an alternative agent depends on the expected future need of the specific local anesthetic. -

The Use of Buffering Solutions in the Pediatrics Local Anesthesia to Reduce the Pain of Minor Procedures
Volume 2- Issue 1 : 2018 DOI: 10.26717/BJSTR.2018.02.000695 Eduardo de Oliveira Duque-Estrada. Biomed J Sci & Tech Res ISSN: 2574-1241 Mini Review Open Access The Use of Buffering Solutions in the Pediatrics Local Anesthesia to Reduce the Pain of Minor Procedures Eduardo de Oliveira Duque-Estrada MD* Received: January 17, 2018; Published: January 25, 2018 *Corresponding author: Eduardo de Oliveira Duque-Estrada, Ex-Professor of Pediatrics and Pediatric Surgery, Teresópolis Schoolof Medicine, Rio de Janeiro, Rua Jose da Silva Ribeiro 119 apt 11 São Paulo, SP Brazil CEP: 05726-130, Email: Abstract The local anesthetics are widely u sed in minor pediatric surgical procedures. The major problem with their use is the resulted pain experienced by the patients at the time of injection. To discuss those situations in the light of the medical literature we present this mini-review. Key words: Local Injection; Pain; Buffer; pH; Lidocaine; Pediatric Surgery Procedure Introduction Table 1: Techniques for injection pain control*. a eutectic mixture of lidocaine and prilocaine (EMLA) cream [17] S.No Techniques for injection pain control before infiltration, and local external cooling (cryoanalgesia) have 1. Warming the anesthetic solution [18,19] (Table 1). also been used to reduce the pain of infiltration of local anesthetic 2. Buffering the anesthetic Buffering the Anesthetic 3. Injection technique 4. Distraction Local anesthesia is extremely useful either as the sole method the best results on the minor surgery in general [3,6]. Blocking 5. Combination anesthetic technique the pain pathway with local anesthetic solution will also reduce 6. Cooling of skin the family stress response to the surgical procedure. -

Annual Medical Student Abstract Journal
Medicine of the Highest Order 2015 Annual Medical Student Abstract Journal Sponsored by: Center for Advocacy, Community Health, Education and Diversity Offices for Medical Education Medical Student Research Faculty Advisory Committee Community Outreach Faculty Advisory Committee International Medicine Faculty Advisory Committee Medical Humanities Faculty Advisory Committee Basic Science, Clinical & Translational Research Aaserude, Eric & Hong, Steven Preceptor: Beau Abar, Ph.D. University of Rochester School of Medicine and Dentistry Department of Emergency Medicine Access to care and depression among emergency department patients Introduction: Major depressive disorder is a serious, common public health concern that is characterized by a series of symptoms including depressed mood and diminished interest or pleasure in most activities of the day (DSM-V). The prevalence of depression during a lifetime is 16.2% and the 12-month prevalence is 6.6%. 1 In particular, several studies have shown that among patients in the Emergency Department (ED), the prevalence of depression is even higher than in the general population.2-3 One study showed that the prevalence of a positive depression screen is approximately 33%, and using a 33% positive predictive value, an estimated 10.5% would met the diagnostic criteria for major depressive disorder.2 Because of the high concentration of patients with depression, the ED may serve as an important forum for the identification of depression and the intervention in the disease process.4 Concomitant to identification of potential concerns regarding depression is the issue of patient access to appropriate care. Many patients lack the ability to affordably receive efficacious treatment due to insurance-related barriers.5 Furthermore, other individuals may be unaware of their level of access for primary and behavioral health services, and this lack of awareness will lead to patients in need not receiving the care appropriate to their concerns. -

Basic Function of the Anesthetic Machine, Part II Some Vaporizers Are Filled with Liquid Agent by Using a Pin Fill Device
Vetamac Vapors (800)334-1583 www.vetamac.com Vol I, Issue 2 Welcome to the second quarterly edition of "Vetamac Vapors". The purpose of this newsletter is to educate your staff with a goal of the best possible patient care. We also would like to inform you of services and products that Vetamac has to offer and to provide support for all of your anesthesia needs. Future editions will cover topics on machines as well as different techniques. Please send comments to the e-mail link at www.vetamac.com. Basic Function of the Anesthetic Machine, Part II Some vaporizers are filled with liquid agent by using a pin fill device. There is an agent specific spout that replaces the cap on the The anesthetic machine must deliver vaporized anesthetic agent bottle. There is a keyed pin that fits into the fill manifold on the agent to the breathing circuit in concentrations that are optimal for the vaporizer. It is locked into place and the vaporizer is filled to the de- sired level on the window. Most vaporizers used in the U.S. have a desired effect. Since the liquid agent is in a closed system, a carrier funnel fill device and the liquid agent is simply poured into the vapor- gas must be present to deliver the vaporized agent to the breathing izer. Care must be exercised to avoid spillage. Anti-Spil™ adapters circuit. The gas used to accomplish this is the fresh gas flow of oxy- are available that replace the cap on the agent bottle and minimize the gen. -

Veterinary Anesthetic and Analgesic Formulary 3Rd Edition, Version G
Veterinary Anesthetic and Analgesic Formulary 3rd Edition, Version G I. Introduction and Use of the UC‐Denver Veterinary Formulary II. Anesthetic and Analgesic Considerations III. Species Specific Veterinary Formulary 1. Mouse 2. Rat 3. Neonatal Rodent 4. Guinea Pig 5. Chinchilla 6. Gerbil 7. Rabbit 8. Dog 9. Pig 10. Sheep 11. Non‐Pharmaceutical Grade Anesthetics IV. References I. Introduction and Use of the UC‐Denver Formulary Basic Definitions: Anesthesia: central nervous system depression that provides amnesia, unconsciousness and immobility in response to a painful stimulation. Drugs that produce anesthesia may or may not provide analgesia (1, 2). Analgesia: The absence of pain in response to stimulation that would normally be painful. An analgesic drug can provide analgesia by acting at the level of the central nervous system or at the site of inflammation to diminish or block pain signals (1, 2). Sedation: A state of mental calmness, decreased response to environmental stimuli, and muscle relaxation. This state is characterized by suppression of spontaneous movement with maintenance of spinal reflexes (1). Animal anesthesia and analgesia are crucial components of an animal use protocol. This document is provided to aid in the design of an anesthetic and analgesic plan to prevent animal pain whenever possible. However, this document should not be perceived to replace consultation with the university’s veterinary staff. As required by law, the veterinary staff should be consulted to assist in the planning of procedures where anesthetics and analgesics will be used to avoid or minimize discomfort, distress and pain in animals (3, 4). Prior to administration, all use of anesthetics and analgesic are to be approved by the Institutional Animal Care and Use Committee (IACUC). -
Local Anesthesia for Carpal Tunnel Surgery
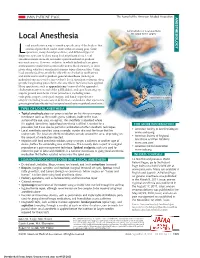
JAMA PATIENT PAGE The Journal of the American Medical Association ANESTHESIOLOGY Administration of local anesthetic Local Anesthesia for carpal tunnel surgery ocal anesthesia is a way to numb a specific area of the body so that a medical procedure can be done without causing pain. Some Loperations, many dental procedures, and different types of diagnostic tests can be done using local anesthesia alone. Local anesthesia medications do not make a person sedated or produce unconsciousness. However, sedation, in which individuals are given medications to make them comfortable and to block memory, is often given along with local anesthesia for many types of procedures. Using local anesthesia alone avoids the side effects of sedation medications and medications used to produce general anesthesia (making an individual unconscious for a procedure). Local anesthetic solutions often provide long-lasting pain relief to the area where they have been applied. Many operations, such as appendectomy (removal of the appendix), cholecystectomy (removal of the gallbladder), and open heart surgery, require general anesthesia. Other procedures, including some orthopedic surgery, urological surgery, and female reproductive Carpal tunnel surgery surgery (including most cesarean deliveries), can be done after a person is given regional anesthesia (such as spinal anesthesia or epidural anesthesia). TYPES OF LOCAL ANESTHESIA • Topical anesthesia places or sprays a solution on the skin or a mucous membrane (such as the mouth, gums, eardrum, inside of the nose, surface of the eye, anus, or vagina). The anesthetic is absorbed where it is applied. Sometimes topical local anesthesia is all that is needed for a FOR MORE INFORMATION procedure, but it can also be part of a combination of other anesthetic techniques. -

Veterinary Anesthesia and Pain Management Secrets / Edited by Stephen A
Publisher: HANLEY & BELFUS, INC. Medical Publishers 210 South 13th Street Philadelphia, PA 19107 (215) 546-7293; 800-962-1892 FAX (215) 790-9330 Web site: http://www.hanleyandbelfus.com Note to the reader Although the information in this book has been carefully reviewed for cor rectness of dosage and indications, neither the authors nor the editor nor the publisher can accept any legal responsibility for any errors or omissions that may be made. Neither the publisher nor the editor makes any warranty, expressed or implied, with respect to the material contained herein. Before prescribing any drug. the reader must review the manu facturer's correct product information (package inserts) for accepted indications, absolute dosage recommendations. and other information pertinent to the safe and effective use of the product described. This is especially important when drugs are given in combination or as an adjunct to other forms of therapy Library of Congress Cataloging-in-Publication Data Veterinary anesthesia and pain management secrets / edited by Stephen A. Greene. p. em. - (The Secrets Series®) Includes bibliographical references (p.). ISBN 1-56053-442-7 (alk paper) I. Veterinary anesthesia-Examinations, questions. etc. 2. Pain in animals Treatment-Examinations, questions, etc. I. Greene, Stephen A., 1956-11. Series. SF914.V48 2002 636 089' 796'076--dc2 I 2001039966 VETERINARY ANESTHESIA AND PAIN MANAGEMENT SECRETS ISBN 1-56053-442-7 © 2002 by Hanley & Belfus, Inc. All rights reserved. No part of this book may be repro duced, reused, republished. or transmitted in any form, or stored in a database or retrieval system, without written permission of the publisher Last digit is the print number: 9 8 7 6 5 4 3 2 CONTRIBUTORS G. -

A Comparison Between the I-Gel® and Air-Q® Supraglottic Airway Devices
Hindawi BioMed Research International Volume 2018, Article ID 5202957, 7 pages https://doi.org/10.1155/2018/5202957 Research Article A Comparison between the i-gelD and air-QD Supraglottic Airway Devices Used for the Patients Undergoing General Anesthesia with Muscle Relaxation Nilofar Massoudi ,1 Mohammad Fathi,1 Navid Nooraei ,2 and Alireza Salehi1 Clinical Research and Development Unit at Shahid Modarres Hospital, Department of Anaesthesiology, Shahid Beheshti University of Medical Sciences, Tehran, Iran Anesthesiology Research Center, Department of Anesthesiology, Shahid Beheshti University of Medical Sciences, Tehran, Iran Correspondence should be addressed to Navid Nooraei; [email protected] Received 14 February 2018; Revised 30 April 2018; Accepted 17 May 2018; Published 18 November 2018 Academic Editor: Yukio Hayashi Copyright © 2018 Nilofar Massoudi et al. Tis is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Objectives. Te aim of the present study was to compare two supraglottic airway (SGA) devices (i.e., the i-gel5 ©IntersurgicalLtd and air-Q5 (Reusable) Cookgas company) in terms of the insertion time, amount of leak during ventilation with maximum positive pressure, and postoperative complications in patients referring to Modarres Hospital in Tehran. Method. Te present double-blind clinical trial was performed on 60 patients undergoing elective surgeries that required general anesthesia with muscle relaxation. Patients were randomly assigned to either i-gel5 (n =30)orAir-Q5 (n =30)groups.Results. Te mean age, body mass index, duration of surgery, duration of anesthesia, and gender ratio were not signifcantly diferent between the two groups. -

Total Solutions for Anesthesia & Surgery
total solutions for Anesthesia & Surgery Ventilation Anesthesia Animal Surgery Temperature Control Physiological Monitoring NEW Catalogs Other Catalogs from Harvard Apparatus 2010 BTX Electroporation Catalog BTX offers a comprehensive line of instruments and accessories for both electroporation and electrofusion of mammalian, bacterial, yeast, fungi, insect and plant cells and tissues. BTX specializes in providing research tools for novel cutting edge applications such as adherent cell electroporation, high- throughput cloning, in vivo gene delivery, in ovo gene delivery, and in & ex utero gene delivery. 2009 Warner 2010 Animal, Organ & Cell Physiology Electrophysiology and This catalog features a broad range of products, including our Cell Biology Catalog legendary line of infusion and perfusion pumps, ventilators and anesthesia systems, surgical instruments and equipment for small For the electrophysiological, cellular, and to larger animals, and isolated organ and tissue systems for all neurological sciences. Our extensive levels of research and education. These products are designed to product line includes voltage and current help you achieve better research results in less time. clamp amplifiers for whole-cell and patch applications. Bessel filters, chambers for imaging and recording systems, perfusion control systems and steppers, 2010 Molecular solution heating systems, microscope translation tables, microelectrodes and holders, and glass capillary tubing, plus Sample Preparation now includes electroporation and transfection systems -

HEYER Pasithec
Anesthesia System Operator’s Manual Rev. 0.2 Draft – 12/09 INNOVATION IN DESIGN AND TECHNOLOGY HEYER Pasithec Contents 1 Statement .......................................................................................................................................................................... 5 1.1 Manufacturer Responsibility...................................................................................................................................... 5 1.2 Security, Reliability and Operating Conditions........................................................................................................... 5 1.3 Return ...................................................................................................................................................................... 6 1.4 Details of the Manufacturer....................................................................................................................................... 6 2 Introduction........................................................................................................................................................................ 7 2.1 Intended Use............................................................................................................................................................ 7 2.1.1 Range of Use .................................................................................................................................................. 7 2.1.2 Contraindication .............................................................................................................................................