Dysregulation of Complement and Coagulation Pathways: Emerging
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

MONONINE (“Difficulty ® Monoclonal Antibody Purified in Concentrating”; Subject Recovered)
CSL Behring IU/kg (n=38), 0.98 ± 0.45 K at doses >95-115 IU/kg (n=21), 0.70 ± 0.38 K at doses >115-135 IU/kg (n=2), 0.67 K at doses >135-155 IU/kg (n=1), and 0.73 ± 0.34 K at doses >155 IU/kg (n=5). Among the 36 subjects who received these high doses, only one (2.8%) Coagulation Factor IX (Human) reported an adverse experience with a possible relationship to MONONINE (“difficulty ® Monoclonal Antibody Purified in concentrating”; subject recovered). In no subjects were thrombo genic complications MONONINE observed or reported.4 only The manufacturing procedure for MONONINE includes multiple processing steps that DESCRIPTION have been designed to reduce the risk of virus transmission. Validation studies of the Coagulation Factor IX (Human), MONONINE® is a sterile, stable, lyophilized concentrate monoclonal antibody (MAb) immunoaffinity chromatography/chemical treatment step and of Factor IX prepared from pooled human plasma and is intended for use in therapy nanofiltration step used in the production of MONONINE doc ument the virus reduction of Factor IX deficiency, known as Hemophilia B or Christmas disease. MONONINE is capacity of the processes employed. These studies were conducted using the rel evant purified of extraneous plasma-derived proteins, including Factors II, VII and X, by use of enveloped and non-enveloped viruses. The results of these virus validation studies utilizing immunoaffinity chromatography. A murine monoclonal antibody to Factor IX is used as an a wide range of viruses with different physicochemical properties are summarized in Table affinity ligand to isolate Factor IX from the source material. -

How Macrophages Deal with Death
REVIEWS CELL DEATH AND IMMUNITY How macrophages deal with death Greg Lemke Abstract | Tissue macrophages rapidly recognize and engulf apoptotic cells. These events require the display of so- called eat-me signals on the apoptotic cell surface, the most fundamental of which is phosphatidylserine (PtdSer). Externalization of this phospholipid is catalysed by scramblase enzymes, several of which are activated by caspase cleavage. PtdSer is detected both by macrophage receptors that bind to this phospholipid directly and by receptors that bind to a soluble bridging protein that is independently bound to PtdSer. Prominent among the latter receptors are the MER and AXL receptor tyrosine kinases. Eat-me signals also trigger macrophages to engulf virus- infected or metabolically traumatized, but still living, cells, and this ‘murder by phagocytosis’ may be a common phenomenon. Finally , the localized presentation of PtdSer and other eat- me signals on delimited cell surface domains may enable the phagocytic pruning of these ‘locally dead’ domains by macrophages, most notably by microglia of the central nervous system. In long- lived organisms, abundant cell types are often process. Efferocytosis is a remarkably efficient business: short- lived. In the human body, for example, the macrophages can engulf apoptotic cells in less than lifespan of many white blood cells — including neutro- 10 minutes, and it is therefore difficult experimentally to phils, eosinophils and platelets — is less than 2 weeks. detect free apoptotic cells in vivo, even in tissues where For normal healthy humans, a direct consequence of large numbers are generated7. Many of the molecules this turnover is the routine generation of more than that macrophages and other phagocytes use to recognize 100 billion dead cells each and every day of life1,2. -

Complement Peptide C3a Receptor 1 Promotes Optic Nerve Degeneration in DBA/2J Mice Jeffrey M
Harder et al. Journal of Neuroinflammation (2020) 17:336 https://doi.org/10.1186/s12974-020-02011-z RESEARCH Open Access Complement peptide C3a receptor 1 promotes optic nerve degeneration in DBA/2J mice Jeffrey M. Harder1, Pete A. Williams1,2 , Catherine E. Braine1,3, Hongtian S. Yang1, Jocelyn M. Thomas1, Nicole E. Foxworth1, Simon W. M. John1,4,5* and Gareth R. Howell1,6,7* Abstract Background: The risk of glaucoma increases significantly with age and exposure to elevated intraocular pressure, two factors linked with neuroinflammation. The complement cascade is a complex immune process with many bioactive end-products, including mediators of inflammation. Complement cascade activation has been shown in glaucoma patients and models of glaucoma. However, the function of complement-mediated inflammation in glaucoma is largely untested. Here, the complement peptide C3a receptor 1 was genetically disrupted in DBA/2J mice, an ocular hypertensive model of glaucoma, to test its contribution to neurodegeneration. Methods: A null allele of C3ar1 was backcrossed into DBA/2J mice. Development of iris disease, ocular hypertension, optic nerve degeneration, retinal ganglion cell activity, loss of RGCs, and myeloid cell infiltration in C3ar1-deficient and sufficient DBA/2J mice were compared across multiple ages. RNA sequencing was performed on microglia from primary culture to determine global effects of C3ar1 on microglia gene expression. Results: Deficiency in C3ar1 lowered the risk of degeneration in ocular hypertensive mice without affecting intraocular pressure elevation at 10.5 months of age. Differences were found in the percentage of mice affected, but not in individual characteristics of disease progression. -

WO 2016/147053 Al 22 September 2016 (22.09.2016) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2016/147053 Al 22 September 2016 (22.09.2016) P O P C T (51) International Patent Classification: (71) Applicant: RESVERLOGIX CORP. [CA/CA]; 300, A61K 31/551 (2006.01) A61P 37/02 (2006.01) 4820 Richard Road Sw, Calgary, AB, T3E 6L1 (CA). A61K 31/517 (2006.01) C07D 239/91 (2006.01) (72) Inventors: WASIAK, Sylwia; 431 Whispering Water (21) International Application Number: Trail, Calgary, AB, T3Z 3V1 (CA). KULIKOWSKI, PCT/IB20 16/000443 Ewelina, B.; 31100 Swift Creek Terrace, Calgary, AB, T3Z 0B7 (CA). HALLIDAY, Christopher, R.A.; 403 (22) International Filing Date: 138-18th Avenue SE, Calgary, AB, T2G 5P9 (CA). GIL- 10 March 2016 (10.03.2016) HAM, Dean; 249 Scenic View Close NW, Calgary, AB, (25) Filing Language: English T3L 1Y5 (CA). (26) Publication Language: English (81) Designated States (unless otherwise indicated, for every kind of national protection available): AE, AG, AL, AM, (30) Priority Data: AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, 62/132,572 13 March 2015 (13.03.2015) US BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, 62/264,768 8 December 2015 (08. 12.2015) US DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, [Continued on nextpage] (54) Title: COMPOSITIONS AND THERAPEUTIC METHODS FOR THE TREATMENT OF COMPLEMENT-ASSOCIATED DISEASES (57) Abstract: The invention comprises methods of modulating the complement cascade in a mammal and for treating and/or preventing diseases and disorders as sociated with the complement pathway by administering a compound of Formula I or Formula II, such as, for example, 2-(4-(2-hydroxyethoxy)-3,5-dimethylphenyl)- 5,7-dimethoxyquinazolin-4(3H)-one or a pharmaceutically acceptable salt thereof. -
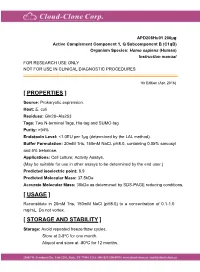
Active Complement Component 1, Q
APD208Hu01 200µg Active Complement Component 1, Q Subcomponent B (C1qB) Organism Species: Homo sapiens (Human) Instruction manual FOR RESEARCH USE ONLY NOT FOR USE IN CLINICAL DIAGNOSTIC PROCEDURES 1th Edition (Apr, 2016) [ PROPERTIES ] Source: Prokaryotic expression. Host: E. coli Residues: Gln28~Ala253 Tags: Two N-terminal Tags, His-tag and SUMO-tag Purity: >94% Endotoxin Level: <1.0EU per 1μg (determined by the LAL method). Buffer Formulation: 20mM Tris, 150mM NaCl, pH8.0, containing 0.05% sarcosyl and 5% trehalose. Applications: Cell culture; Activity Assays. (May be suitable for use in other assays to be determined by the end user.) Predicted isoelectric point: 8.9 Predicted Molecular Mass: 37.5kDa Accurate Molecular Mass: 38kDa as determined by SDS-PAGE reducing conditions. [ USAGE ] Reconstitute in 20mM Tris, 150mM NaCl (pH8.0) to a concentration of 0.1-1.0 mg/mL. Do not vortex. [ STORAGE AND STABILITY ] Storage: Avoid repeated freeze/thaw cycles. Store at 2-8oC for one month. Aliquot and store at -80oC for 12 months. Stability Test: The thermal stability is described by the loss rate. The loss rate was determined by accelerated thermal degradation test, that is, incubate the protein at 37oC for 48h, and no obvious degradation and precipitation were observed. The loss rate is less than 5% within the expiration date under appropriate storage condition. [ SEQUENCE ] [ ACTIVITY ] The complement component 1q (or simply C1q) is a protein complex involved in the complement system, which is part of the innate immune system. C1q together with C1r and C1s form the C1 complex. Antibodies of the adaptive immune system can bind antigen, forming an antigen-antibody complex. -

The Central Role of Fibrinolytic Response in COVID-19—A Hematologist’S Perspective
International Journal of Molecular Sciences Review The Central Role of Fibrinolytic Response in COVID-19—A Hematologist’s Perspective Hau C. Kwaan 1,* and Paul F. Lindholm 2 1 Division of Hematology/Oncology, Department of Medicine, Feinberg School of Medicine, Northwestern University, Chicago, IL 60611, USA 2 Department of Pathology, Feinberg School of Medicine, Northwestern University, Chicago, IL 60611, USA; [email protected] * Correspondence: [email protected] Abstract: The novel coronavirus disease (COVID-19) has many characteristics common to those in two other coronavirus acute respiratory diseases, severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS). They are all highly contagious and have severe pulmonary complications. Clinically, patients with COVID-19 run a rapidly progressive course of an acute respiratory tract infection with fever, sore throat, cough, headache and fatigue, complicated by severe pneumonia often leading to acute respiratory distress syndrome (ARDS). The infection also involves other organs throughout the body. In all three viral illnesses, the fibrinolytic system plays an active role in each phase of the pathogenesis. During transmission, the renin-aldosterone- angiotensin-system (RAAS) is involved with the spike protein of SARS-CoV-2, attaching to its natural receptor angiotensin-converting enzyme 2 (ACE 2) in host cells. Both tissue plasminogen activator (tPA) and plasminogen activator inhibitor 1 (PAI-1) are closely linked to the RAAS. In lesions in the lung, kidney and other organs, the two plasminogen activators urokinase-type plasminogen activator (uPA) and tissue plasminogen activator (tPA), along with their inhibitor, plasminogen activator 1 (PAI-1), are involved. The altered fibrinolytic balance enables the development of a hypercoagulable Citation: Kwaan, H.C.; Lindholm, state. -

Complement Component 4 Genes Contribute Sex-Specific Vulnerability in Diverse Illnesses
bioRxiv preprint doi: https://doi.org/10.1101/761718; this version posted September 9, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-ND 4.0 International license. Complement component 4 genes contribute sex-specific vulnerability in diverse illnesses Nolan Kamitaki1,2, Aswin Sekar1,2, Robert E. Handsaker1,2, Heather de Rivera1,2, Katherine Tooley1,2, David L. Morris3, Kimberly E. Taylor4, Christopher W. Whelan1,2, Philip Tombleson3, Loes M. Olde Loohuis5,6, Schizophrenia Working Group of the Psychiatric Genomics Consortium7, Michael Boehnke8, Robert P. Kimberly9, Kenneth M. Kaufman10, John B. Harley10, Carl D. Langefeld11, Christine E. Seidman1,12,13, Michele T. Pato14, Carlos N. Pato14, Roel A. Ophoff5,6, Robert R. Graham15, Lindsey A. Criswell4, Timothy J. Vyse3, Steven A. McCarroll1,2 1 Department of Genetics, Harvard Medical School, Boston, Massachusetts 02115, USA 2 Stanley Center for Psychiatric Research, Broad Institute of MIT and Harvard, Cambridge, Massachusetts 02142, USA 3 Department of Medical and Molecular Genetics, King’s College London, London WC2R 2LS, UK 4 Rosalind Russell / Ephraim P Engleman Rheumatology Research Center, Division of Rheumatology, UCSF School of Medicine, San Francisco, California 94143, USA 5 Department of Human Genetics, David Geffen School of Medicine, University of California, Los Angeles, California 90095, USA 6 Center for Neurobehavioral Genetics, Semel Institute for Neuroscience and Human Behavior, University of California, Los Angeles, California 90095, USA 7 A full list of collaborators is in Supplementary Information. -

Investigation of Candidate Genes and Mechanisms Underlying Obesity
Prashanth et al. BMC Endocrine Disorders (2021) 21:80 https://doi.org/10.1186/s12902-021-00718-5 RESEARCH ARTICLE Open Access Investigation of candidate genes and mechanisms underlying obesity associated type 2 diabetes mellitus using bioinformatics analysis and screening of small drug molecules G. Prashanth1 , Basavaraj Vastrad2 , Anandkumar Tengli3 , Chanabasayya Vastrad4* and Iranna Kotturshetti5 Abstract Background: Obesity associated type 2 diabetes mellitus is a metabolic disorder ; however, the etiology of obesity associated type 2 diabetes mellitus remains largely unknown. There is an urgent need to further broaden the understanding of the molecular mechanism associated in obesity associated type 2 diabetes mellitus. Methods: To screen the differentially expressed genes (DEGs) that might play essential roles in obesity associated type 2 diabetes mellitus, the publicly available expression profiling by high throughput sequencing data (GSE143319) was downloaded and screened for DEGs. Then, Gene Ontology (GO) and REACTOME pathway enrichment analysis were performed. The protein - protein interaction network, miRNA - target genes regulatory network and TF-target gene regulatory network were constructed and analyzed for identification of hub and target genes. The hub genes were validated by receiver operating characteristic (ROC) curve analysis and RT- PCR analysis. Finally, a molecular docking study was performed on over expressed proteins to predict the target small drug molecules. Results: A total of 820 DEGs were identified between -

Assembly of an Integrated Human Lung Cell Atlas Reveals That
medRxiv preprint doi: https://doi.org/10.1101/2020.06.02.20120634; this version posted June 4, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. It is made available under a CC-BY-NC-ND 4.0 International license . Assembly of an integrated human lung cell atlas reveals that SARS-CoV-2 receptor is co-expressed with key elements of the kinin-kallikrein, renin-angiotensin and coagulation systems in alveolar cells Davi Sidarta-Oliveira1,2, Carlos Poblete Jara1,3, Adriano J. Ferruzzi4, Munir S. Skaf4, William H. Velander5, Eliana P. Araujo1,3, Licio A. Velloso1 1Laboratory of Cell Signaling, Obesity and Comorbidities Research Center, University of Campinas, Brazil 2 Physician-Scientist Graduate Program, School of Medical Sciences, University of Campinas, Brazil 3Nursing School, University of Campinas, Brazil 4Institute of Chemistry and Center for Computing in Engineering and Sciences University of Campinas, Brazil 5Department of Chemical and Biomolecular Engineering, University of Nebraska, Lincoln, USA Correspondence: Licio A. Velloso Laboratory of Cell Signaling, Obesity and Comorbidities Research Center, University of Campinas, Campinas, Brazil Address: Rua Carl Von Lineaus s/n, Instituto de Biologia - Bloco Z. Campus Universitário Zeferino Vaz - Barão Geraldo, Campinas - SP, 13083-864 Phone: +55 19 3521-0025 E-mail: [email protected] Abstract SARS-CoV-2, the pathogenic agent of COVID-19, employs angiotensin converting enzyme-2 (ACE2) as its cell entry receptor. Clinical data reveal that in severe COVID- 19, SARS-CoV-2 infects the lung, leading to a frequently lethal triad of respiratory insufficiency, acute cardiovascular failure, and coagulopathy. -

The Potential Role of Recombinant Activated FVII in the Management of Critical Hemato-Oncological Bleeding: a Systematic Review
Bone Marrow Transplantation (2007) 39, 729–735 & 2007 Nature Publishing Group All rights reserved 0268-3369/07 $30.00 www.nature.com/bmt REVIEW The potential role of recombinant activated FVII in the management of critical hemato-oncological bleeding: a systematic review M Franchini1, D Veneri2 and G Lippi3 1Servizio di Immunoematologia e Trasfusione – Centro Emofilia, Azienda Ospedaliera di Verona, Verona, Italy; 2Dipartimento di Medicina Clinica e Sperimentale, Sezione di Ematologia, Universita` di Verona, Verona, Italy and 3Dipartimento di Scienze Biomediche e Morfologiche, Istituto di Chimica e Microscopia Clinica, Universita` di Verona, Verona, Italy Recombinant activated factor VII (rFVIIa) is an hemo- situations unresponsive to conventional therapy to control static agent that was originally developed for the excessive bleeding and reduce exposure to allogeneic blood. treatment of hemorrhage in patients with hemophilia and These include intracerebral hemorrhage, oral anticoagu- inhibitors.However, in the last few years rFVIIa has been lant-induced hemorrhage, thrombocytopenia, bleeding employed with success in a broad spectrum of congenital associated with hepatic failure, major surgery, trauma and acquired bleeding conditions.In this systematic review and life-threatening obstetrical, and gynecologic hemor- we present the current knowledge on the use of this drug in rhagic complications.5–9 patients suffering from hemato-oncological disorders, In this systematic review we have collected the available which are quite commonly complicated by severe hemor- data from the literature on the use of rFVIIa in hemato- rhage.On the whole, data in the literature suggest a oncological patients with severe bleeding, unresponsive to potential role for rFVIIa in the management of bleeding standard therapy. -

Are Complement Deficiencies Really Rare?
G Model MIMM-4432; No. of Pages 8 ARTICLE IN PRESS Molecular Immunology xxx (2014) xxx–xxx Contents lists available at ScienceDirect Molecular Immunology j ournal homepage: www.elsevier.com/locate/molimm Review Are complement deficiencies really rare? Overview on prevalence, ଝ clinical importance and modern diagnostic approach a,∗ b Anete Sevciovic Grumach , Michael Kirschfink a Faculty of Medicine ABC, Santo Andre, SP, Brazil b Institute of Immunology, University of Heidelberg, Heidelberg, Germany a r a t b i c s t l e i n f o r a c t Article history: Complement deficiencies comprise between 1 and 10% of all primary immunodeficiencies (PIDs) accord- Received 29 May 2014 ing to national and supranational registries. They are still considered rare and even of less clinical Received in revised form 18 June 2014 importance. This not only reflects (as in all PIDs) a great lack of awareness among clinicians and gen- Accepted 23 June 2014 eral practitioners but is also due to the fact that only few centers worldwide provide a comprehensive Available online xxx laboratory complement analysis. To enable early identification, our aim is to present warning signs for complement deficiencies and recommendations for diagnostic approach. The genetic deficiency of any Keywords: early component of the classical pathway (C1q, C1r/s, C2, C4) is often associated with autoimmune dis- Complement deficiencies eases whereas individuals, deficient of properdin or of the terminal pathway components (C5 to C9), are Warning signs Prevalence highly susceptible to meningococcal disease. Deficiency of C1 Inhibitor (hereditary angioedema, HAE) Meningitis results in episodic angioedema, which in a considerable number of patients with identical symptoms Infections also occurs in factor XII mutations. -

Recent Developments in the Understanding and Management of Paroxysmal Nocturnal Haemoglobinuria
review Recent developments in the understanding and management of paroxysmal nocturnal haemoglobinuria Anita Hill, Stephen J. Richards and Peter Hillmen Department of Haematology, Leeds Teaching Hospitals NHS Trust, Great George Street, Leeds, UK Summary only one G6PD variant enzyme was present in the PNH red cells whereas both variants were present in the residual normal red Paroxysmal nocturnal haemoglobinuria (PNH) has been rec- cells, provided conclusive evidence of the clonal nature of PNH ognised as a discrete disease entity since 1882. Approximately a (Oni et al, 1970). It was clear by the 1980s that PNH cells were half of patients will eventually die as a result of having PNH. deficient in a large number of cell surface proteins, but it was Many of the symptoms of PNH, including recurrent abdominal unclear how this related to either the monoclonal nature of PNH pain, dysphagia, severe lethargy and erectile dysfunction, result or the haemolysis. The development of immortalised cell lines from intravascular haemolysis with absorption of nitric oxide with the PNH abnormality (both B- and T-cells lines) facilitated by free haemoglobin from the plasma. These symptoms, as well the rapid elucidation of the defect (Schubert et al, 1990; Hillmen as the occurrence of thrombosis and aplasia, significantly affect et al,1992;Nakakumaet al,1994).Itbecameclearthatavarietyof patients’ quality of life; thrombosis is the leading cause of proteins normally attached to the cell membrane by a glycolipid premature mortality. The syndrome of haemolytic-anaemia- structure, were found to be abnormal, and that this was due to a associated pulmonary hypertension has been further identified disruption in the glycosylphosphatidylinositol (GPI) biosyn- in PNH patients.