Butisol Sodium Ciii
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Kava (Piper Methysticum) and Its Methysticin Constituents Protect Brain Tissue Against Ischemic Damage in Rodents
5 Refs: Arletti R et al, Stimulating property of Turnera diffusa and Pfaffia paniculata extracts on the sexual-behavior of male rats. Psychopharmacology 143(1), 15-19, 1999. Berger F, Handbuch der drogenkunde . Vol 2, Maudrich, Wien, 1950. Martinez M, Les plantas medicinales de Mexico . Cuarta Edicion Botas Mexico , p119, 1959. Tyler VE et al, Pharmacognosy , 9 th edition, Lea & Febiger, Philadelphia, 1988. KAVA ( Piper methysticum ) - A REVIEW The Kava plant (Piper methysticum) is a robust, well-branching and erect perennial shrub belonging to the pepper family (Piperaceae). The botanical origin remains unknown, although it is likely that early Polynesian explorers brought the plant with them from island to island. Numerous varieties of Kava exist, and today it is widely cultivated in several Pacific Island countries both for local use as well as the rapidly growing demand for pharmaceutical preparations. The dried rhizomes (roots) are normally used. The first description to the western world of the ceremonial use of an intoxicating beverage prepared from Kava was made by Captain James Cook following his Pacific voyage in 1768. The drink, prepared as an infusion in an elaborate manner after first chewing the root, is consumed on formal occasions or meetings of village elders and chiefs, as well as in reconciling with enemies and on a more social basis. It remains an important social custom in many Pacific Island countries today. Most of the islands of the Pacific possessed Kava prior to European contact, particularly those encompassed by Polynesia, Melanesia and Micronesia. After drinking the Kava beverage a pleasantly relaxed and sociable state develops, after which a deep and restful sleep occurs. -

Alternative Treatments for Depression and Anxiety
2019 PCB Conference: Strickland Benzodiazepines (BZDs), Herbal and Alternative Treatments for Anxiety & Depression BZD Learning Objectives • List at least three uses for benzodiazepines • Discuss at least two risk factors associated with benzodiazepine prescriptions Craig Strickland, PhD, Owner Biobehavioral Education and Consultation https://sites.google.com/site/bioedcon 1 2 BZD Pharmacokinetics Clinical Uses of BZDs Generic Name Trade Name Rapidity ½ Life Dose (mg) • Treat a variety of anxiety disorders alprazolam Xanax Intermediate Short 0.75-4 • Hypnotics • Muscle relaxants chlordiaze- Librium Intermediate Long 15-100 poxide • To produce anterograde amnesia clonazepam Klonopin Intermediate Long 0.5-4 • Alcohol & other CNS depressant withdrawal • Anti-convulsant therapy diazepam Valium Rapid Long 4-40 triazolam Halcion Intermediate Very short 0.125-0.5 temazepam Restoril Short Short 7.5-30 3 4 1 2019 PCB Conference: Strickland Issues with BZDs Herbal Medication and Alternative Therapies Used in the Treatment of Depression and Anxiety • Addictive potential • Confusion between “anti-anxiety” effects and the “warm-fuzzy) • Large dose ranges • Comparison of BZDs with medications like Buspar, etc. • They work, they work well and they work quickly 5 6 Alternative Tx. Learning Objectives Background Information on herbals: Natural does not necessarily mean “safe” • List several amino acid treatments for depression • Side-effects and adverse reactions • List at least three of the most common herbal – Herbal medications are “drugs” although -

Benzodiazepines: Uses and Risks Charlie Reznikoff, MD Hennepin Healthcare
Benzodiazepines: Uses and Risks Charlie Reznikoff, MD Hennepin healthcare 4/22/2020 Overview benzodiazepines • Examples of benzos and benzo like drugs • Indications for benzos • Pharmacology of benzos • Side effects and contraindications • Benzo withdrawal • Benzo tapers 12/06/2018 Sedative/Hypnotics • Benzodiazepines • Alcohol • Z-drugs (Benzo-like sleeping aids) • Barbiturates • GHB • Propofol • Some inhalants • Gabapentin? Pregabalin? 12/06/2018 Examples of benzodiazepines • Midazolam (Versed) • Triazolam (Halcion) • Alprazolam (Xanax) • Lorazepam (Ativan) • Temazepam (Restoril) • Oxazepam (Serax) • Clonazepam (Klonopin) • Diazepam (Valium) • Chlordiazepoxide (Librium) 4/22/2020 Sedatives: gaba stimulating drugs have incomplete “cross tolerance” 12/06/2018 Effects from sedative (Benzo) use • Euphoria/bliss • Suppresses seizures • Amnesia • Muscle relaxation • Clumsiness, visio-spatial impairment • Sleep inducing • Respiratory suppression • Anxiolysis/disinhibition 12/06/2018 Tolerance to benzo effects? • Effects quickly diminish with repeated use (weeks) • Euphoria/bliss • Suppresses seizures • Effects incompletely diminish with repeated use • Amnesia • Muscle relaxation • Clumsiness, visio-spatial impairment • Seep inducing • Durable effects with repeated use • Respiratory suppression • Anxiolysis/disinhibition 12/06/2018 If you understand this pharmacology you can figure out the rest... • Potency • 1 mg diazepam <<< 1 mg alprazolam • Duration of action • Half life differences • Onset of action • Euphoria, clinical utility in acute -

Deliberate Self-Poisoning with a Lethal Dose of Pentobarbital: Survival with Supportive Care
Deliberate self-poisoning with a lethal dose of pentobarbital: Survival with supportive care. (1) (1,2) Santosh Gone , Andis Graudins (1) Clinical Toxicology Service, Program of Emergency Medicine, Monash Health (2) Monash Emergency Research Collaboration, Clinical Sciences at Monash Health, Monash University Abstract 84 INTRODUCTION CASE REPORT (continued) DISCUSSION Pentobarbital (Nembutal) is short acting In the ED: Pentobarbital has been a banned substance for barbiturate sedative-hypnotic, currently widely GCS: 3/15, fixed dilated pupils, apnoeic and human use in Australia since 1998. However, it can used in veterinary practice for anesthesia and ventilated. be procured overseas or bought on the internet. euthanasia. Pulse: 116 bpm sinus tachycardia BP: 115/60 on epinephrine infusion. Pentobarbital is recommended as an effective It is also commonly recommended as a VBG: pH 7.03 pCO2 77 mmHg Bicarb 19 mmol/L agent for use in euthanasia due to its apparently euthanasia drug for assisted suicide and it is Lactate 8.8 mmol/L peaceful transition to death. unlikely that any resuscitative measures will be Activated charcoal (50g) given via an NG tube. attempted in such cases. Course in the Intensive Care Department: In a case series of 150 assisted suicides in Day-1 post-OD: Sweden, a 100% success rate was seen with Intentional overdose results in depression of - Absent brain stem reflexes and fixed dilated pupils for ingestion of 9 grams. Cardiovascular collapse was brain stem function and rapid onset respiratory five days. seen within 15 minutes in 30% of patients. It is rare depression and apnoea. Hypotension also - Diabetes insipidus developed with urine output of to see survival after intentional ingestion for develops, followed by cardiovascular collapse 300ml/hour. -

And Calcium, Magnesium, Potassium and Sodium Oxybates (Xywav™)
Louisiana Medicaid Sodium Oxybate (Xyrem®) and Calcium, Magnesium, Potassium and Sodium Oxybates (Xywav™) The Louisiana Uniform Prescription Drug Prior Authorization Form should be utilized to request clinical authorization for sodium oxybate (Xyrem®) and calcium, magnesium, potassium and sodium oxybates (Xywav™). These agents have Black Box Warnings and are subject to Risk Evaluation and Mitigation Strategy (REMS) under FDA safety regulations. Please refer to individual prescribing information for details. Approval Criteria • The recipient is 7 years of age or older on date of request; AND • The recipient has a documented diagnosis of narcolepsy or cataplexy; AND • The prescribing provider is a Board-Certified Neurologist or a Board-Certified Sleep Medicine Physician; AND • By submitting the authorization request, the prescriber attests to the following: o The prescribing information for the requested medication has been thoroughly reviewed, including any Black Box Warning, Risk Evaluation and Mitigation Strategy (REMS), contraindications, minimum age requirements, recommended dosing, and prior treatment requirements; AND o All laboratory testing and clinical monitoring recommended in the product prescribing information have been completed as of the date of the request and will be repeated as recommended; AND o The recipient has no inappropriate concomitant drug therapies or disease states. Duration of initial authorization approval: 3 months Reauthorization Criteria • The recipient continues to meet all initial approval criteria; AND -

Prescription Drug Management
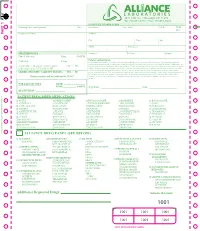
Check out our new site: www.acllaboratories.com Prescription Drug Management Non Adherence, Drug Misuse, Increased Healthcare Costs Reports from the Centers for DiseasePrescription Control and Prevention (CDC) say Drug deaths from Managementmedication overdose have risen for 11 straight years. In 2008 more than 36,000 people died from drug overdoses, and most of these deaths were caused by prescription Nondrugs. Adherence,1 Drug Misuse, Increased Healthcare Costs The CDC analysis found that nearly 40,000 drug overdose deaths were reported in 2010. Prescribed medication accounted for almost 60 percent of the fatalities—far more than deaths from illegal street drugs. Abuse of painkillers like ReportsOxyContin from and the VicodinCenters forwere Disease linked Control to the and majority Prevention of the (CDC) deaths, say deaths from according to the report.1 medication overdose have risen for 11 straight years. In 2008 more than 36,000 people died from drug overdoses, and most of these deaths were caused by prescription drugs. 1 A health economics study analyzed managed care claims of more than 18 million patients, finding that patients undergoing opioid therapyThe CDCfor chronic analysis pain found who that may nearly not 40,000 be following drug overdose their prescription deaths were regimenreported in 2010. Prescribed medication accounted for almost 60 percent of the fatalities—far more than deaths have significantly higher overall healthcare costs. from illegal street drugs. Abuse of painkillers like OxyContin and Vicodin were linked to the majority of the deaths, according to the report.1 ACL offers drug management testing to provide information that can aid clinicians in therapy and monitoring to help improve patientA health outcomes. -
Additional Requested Drugs
PART 1 PART PATIENT PRESCRIBED MEDICATIONS: o ACTIQ o DESIPRAMINE o HYDROCODONE o MORPHINE o ROXICODONE o ADDERALL o DIAZEPAM* o HYDROMORPHONE o MS CONTIN o SOMA o ALPRAZOLAM* o DILAUDID o IMIPRAMINE o NEURONTIN o SUBOXONE o AMBIEN o DURAGESIC o KADIAN o NORCO o TEMAZEPAM o AMITRIPTYLINE o ELAVIL o KETAMINE o NORTRIPTYLINE o TRAMADOL* o ATIVAN o EMBEDA o KLONOPIN o NUCYNTA o TYLENOL #3 o AVINZA o ENDOCET o LORAZEPAM o OPANA o ULTRAM o BUPRENEX o FENTANYL* o LORTAB o OXYCODONE o VALIUM o BUPRENORPHINE o FIORICET o LORCET o OXYCONTIN o VICODIN o BUTRANS o GABAPENTIN o LYRICA o PERCOCET o XANAX o CLONAZEPAM* o GRALISE o METHADONE o RESTORIL TO RE-ORDER CALL RITE-PRINT 718/384-4288 RITE-PRINT CALL TO RE-ORDER ALLIANCE DRUG PANEL (SEE BELOW) o ALCOHOL o BARBITURATES o ILLICITS o MUSCLE RELAXANTS o OPIODS (SYN) ETHANOL PHENOBARBITAL 6-MAM (HEROIN)* CARISPRODOL FENTANYL* BUTABARBITAL a-PVP MEPROBAMATE MEPERIDINE o AMPHETAMINES SECOBARBITAL BENZOYLECGONINE NALOXONE AMPHETAMINE PENTOBARBITAL LSD o OPIODS (NATURAL) METHADONE* METHAMPHETAMINE BUTALBITAL MDA CODEINE METHYLPHENEDATE MDEA MORPHINE o NON-OPIOID o BENZODIAZEPINES MDMA ANALGESICS o OPIODS (SEMI-SYN) o ANTICONVULSIVES ALPRAZOLAM* MDPV TRAMADOL BUPRENORPHINE* GABAPENTIN CLONAZEPAM* MEPHEDRONE TAPENTADOL DIHROCODEINE PREGABALIN DIAZEPAM METHCATHINONE DESOMORPHINE o NON-BENZODIAZEPINE FLUNITRAZEPAM* METHYLONE HYDROCODONE HYPNOTIC o ANTIDEPRESSANTS FLURAZEPAM* PCP HYDROMORPHONE ZOLPIDEM* AMITRIPTYLINE LORAZEPAM THC* OXYCODONE DOXEPIN OXAZEPAM CBD ° OXYMORPHONE o MISCELLANEOUS DRUGS IMIPRIMINE -

Pharmacology on Your Palms CLASSIFICATION of the DRUGS
Pharmacology on your palms CLASSIFICATION OF THE DRUGS DRUGS FROM DRUGS AFFECTING THE ORGANS CHEMOTHERAPEUTIC DIFFERENT DRUGS AFFECTING THE NERVOUS SYSTEM AND TISSUES DRUGS PHARMACOLOGICAL GROUPS Drugs affecting peripheral Antitumor drugs Drugs affecting the cardiovascular Antimicrobial, antiviral, Drugs affecting the nervous system Antiallergic drugs system antiparasitic drugs central nervous system Drugs affecting the sensory Antidotes nerve endings Cardiac glycosides Antibiotics CNS DEPRESSANTS (AFFECTING THE Antihypertensive drugs Sulfonamides Analgesics (opioid, AFFERENT INNERVATION) Antianginal drugs Antituberculous drugs analgesics-antipyretics, Antiarrhythmic drugs Antihelminthic drugs NSAIDs) Local anaesthetics Antihyperlipidemic drugs Antifungal drugs Sedative and hypnotic Coating drugs Spasmolytics Antiviral drugs drugs Adsorbents Drugs affecting the excretory system Antimalarial drugs Tranquilizers Astringents Diuretics Antisyphilitic drugs Neuroleptics Expectorants Drugs affecting the hemopoietic system Antiseptics Anticonvulsants Irritant drugs Drugs affecting blood coagulation Disinfectants Antiparkinsonian drugs Drugs affecting peripheral Drugs affecting erythro- and leukopoiesis General anaesthetics neurotransmitter processes Drugs affecting the digestive system CNS STIMULANTS (AFFECTING THE Anorectic drugs Psychomotor stimulants EFFERENT PART OF THE Bitter stuffs. Drugs for replacement therapy Analeptics NERVOUS SYSTEM) Antiacid drugs Antidepressants Direct-acting-cholinomimetics Antiulcer drugs Nootropics (Cognitive -

Choice of Drugs in the Treatment of Rheumatoid Arthritis
RHEUMATOLOGY IN GENERAL PRACTICE 7 Those with predominant but never exclusive involvement of the terminal finger joint, usually associated with changes in the nail of the same finger; they are serologically negative. There may be a swollen finger with loss of the skin markings-a sort of dactylitis, again serologically negative. (2) Those with a much more severe process which produces loss of movement in the spine and changes in the sacroiliac joints much the same as those in ankylosing spondylitis; unlike ankylosing spondylitis, it produces severe deformity often with ankylosis in peripheral joints. Many of the finger joints become deformed and ankylosed. (3) Those cases indistinguishable from rheumatoid arthritis although the majority are sero-negative. The Stevens Johnson syndrome produces acute effusions, particularly in large joints. It is sometimes associated with the rash of erythema multiforme, always with ulceration in the mouth and genital tract; the mouth ulcers are accompanied by sloughing, unlike those of Beh9et's syndrome which we come to next. BehCet's syndrome, originally described as a combination of orogenital ulceration with relapsing iritis, is now expanded to include skin lesions, other eye lesions, lesions of the central nervous system, thrombophlebitis migrans, and arthropathy (occurring in 64 per cent). The onset is acute, often affecting only a single joint and settling without residual trouble. Choice of drugs in the treatment of rheumatoid arthritis Dr Dudley Hart, M.D., F.R.C.P. (Consultant physician, Westminster Hospital and Medical School) There are many potential drugs for the treatment of rheumatoid disease, but what are we treating in this disorder? Pain in rheumatoid arthritis is but one of the symp- toms. -

Substance Abuse
MODULE \ Substance Abuse For the Ethiopian Health Center Team Yigzaw Kebede, Tefera Abula, Belete Ayele, Amsalu Feleke, Getu Degu, Abera Kifle, Zeleke Alebachew, Endris Mekonnen, and Belay Tessema University of Gondar In collaboration with the Ethiopia Public Health Training Initiative, The Carter Center, the Ethiopia Ministry of Health, and the Ethiopia Ministry of Education April 2005 Funded under USAID Cooperative Agreement No. 663-A-00-00-0358-00. Produced in collaboration with the Ethiopia Public Health Training Initiative, The Carter Center, the Ethiopia Ministry of Health, and the Ethiopia Ministry of Education. Important Guidelines for Printing and Photocopying Limited permission is granted free of charge to print or photocopy all pages of this publication for educational, not-for-profit use by health care workers, students or faculty. All copies must retain all author credits and copyright notices included in the original document. Under no circumstances is it permissible to sell or distribute on a commercial basis, or to claim authorship of, copies of material reproduced from this publication. ©2005 by Yigzaw Kebede, Tefera Abula, Belete Ayele, Amsalu Feleke, Getu Degu, Abera Kifle, Zeleke Alebachew, Endris Mekonnen, and Belay Tessema All rights reserved. Except as expressly provided above, no part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without written permission of the author or authors. This material is intended for educational use only by practicing health care workers or students and faculty in a health care field. ACKNOWLEDGMENTS The preparation and development of this module on Substance Abuse has the contribution of many teaching staffs of the Gondar University College. -
Foundations Week 2.Pdf
Foundations of Addictions Week 2 Glenn Maynard LPC Overview of Addictions • Debate in US continues on whether addiction is a disease, poor behavioral decision making or a moral failing • Prior to Prohibition, Temperance Movement placed the cause in the substance and then in the user • AA- moved the cause to the user and formed the basis of the disease model and behavioral model Addictions Counseling • Full cycle from mental health orientation to separate field and back to mental health under the name behavioral health • Long history of people in recovery working as lay counselors • Standards for addictions counselors began to evolve in the 1970’s Addictions Certification • 1972 JCAH developed accreditation standards that brought addictions into the mainstream • NIDA and NIAAA developed standards for training including 2 years recovery; one year counseling experience and written examination • Current certifications- CADC, NCADC, MAC Reuniting Addictions and Mental Health • Increased Federal and State interest in dual dx • Behavioral health includes addictions as a focus of interest • Administrative for AOD acknowledge licensed professionals as providers Brickman Schema Is the person responsible for changing the Addictive Behavior? Is the person responsible for the development of the Addictive Behavior? Yes No Yes Moral Model (War on Spiritual Model (AA and Drugs) 12-Step) Lack of willpower Loss of contact with higher power No Compensatory Model Disease Model (Heredity (Cognitive) and Physiology) Errors in judgement Activation of disease -
![Nembutal [Pentobarbital] Injection and Seconal [Secobarbital] Capsules](https://docslib.b-cdn.net/cover/6349/nembutal-pentobarbital-injection-and-seconal-secobarbital-capsules-686349.webp)
Nembutal [Pentobarbital] Injection and Seconal [Secobarbital] Capsules
Pharmacy Benefit Coverage Criteria Effective Date .......................................... 12/1/2020 Next Review Date… ................................... 12/1/2021 Coverage Policy Number ................................ P0095 Nembutal [pentobarbital] injection and Seconal [secobarbital] capsules Table of Contents Related Coverage Resources Overview .............................................................. 1 Coverage Policy ................................................... 1 FDA Summary ..................................................... 1 General Background ............................................ 2 References .......................................................... 2 INSTRUCTIONS FOR USE The following Coverage Policy applies to health benefit plans administered by Cigna Companies. Certain Cigna Companies and/or lines of business only provide utilization review services to clients and do not make coverage determinations. References to standard benefit plan language and coverage determinations do not apply to those clients. Coverage Policies are intended to provide guidance in interpreting certain standard benefit plans administered by Cigna Companies. Please note, the terms of a customer’s particular benefit plan document [Group Service Agreement, Evidence of Coverage, Certificate of Coverage, Summary Plan Description (SPD) or similar plan document] may differ significantly from the standard benefit plans upon which these Coverage Policies are based. For example, a customer’s benefit plan document may contain a specific