Official Committee Hansard
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Media De Presse
hockey GEE-GEES 2019-20 MEDIA uottawageegees www. .ca GUIDE geegees DE PRESSE contents / ith more than 41,000 students coming from more than 150 countries, the University of Ottawa is a vibrant, cosmopolitan table des matiÈres community that works, studies and celebrates in both English and RESULTS / RÉSULTATS 4 French. The University’s location in the heart of Canada’s capital city affords privileged access to a broad range of national ROSTER / ALIGNEMENT 5 institutions, resources and services. COACHES / ENTRAÎNEURS 6 PLAYERS / JOUEURS 8 Through a diverse offering of multi-disciplinary STATS AND STANDINGS / STATISTIQUES ET CLASSEMENTS 18 teaching and research programs, the University of Ottawa also plays an TEAM RECORDS AND HISTORY / RECORDS D’ÉQUIPE 19 increasingly influential role on the national and international stage. UNIVERSITY INFORMATION ORIGIN OF GEE-GEES NAME: FOUNDED: 1848 Founded in 1848, the University of Ottawa adopted its official colours Garnet ENROLLMENT: 41,754 and Grey, and like many nineteenth-century institutions, the athletics teams LOCATION: Ottawa, Ont. were known only by the school's colours. Eventually, a connection was made PRESIDENT: Jacques Frémont between the shorthand "GGs" and "Gee-Gee", the common British nickname for ATHLETIC DIRECTOR: Sue Hylland a racehorse. The unique Gee-Gees name and iconic logo known today is a result CONFERENCE: Ontario University Athletics (OUA) of 170 years of history in Ottawa. COLOURS: Garnet and Grey NICKNAME: Gee-Gees WEB SITE: www.geegees.ca Sports Information Contact: Spencer -
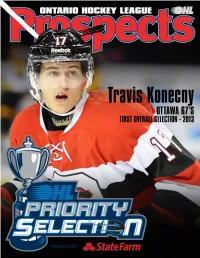
2014 Ohl Priority Selection Information Guide
2014 OHL PRIORITY SELECTION INFORMATION GUIDE 1 2 ONTARIO HOCKEY LEAGUE OHL PRIORITY SELECTION OHL Priority Selection Process In 2001, the Ontario Hockey League Selected Players in the OHL games with non-playoff teams select- Scouting Bureau with evaluations from conducted the annual Priority Selec- OHL Member Teams are permitted to ing ahead of playoff teams. their team scouting staffs to make their tion process by way of the Internet for register a maximum of four 16 year old player selections. the first time in league history. players selected in the OHL Priority Teams are permitted to trade draft Selection. Those 16 year old players choices, other than their first round The OHL Central Scouting Bureau The new process allowed for eligible that are allowed to be signed are the selection, during the trading period has been evaluating players since the players and their families, as well as first two 16 year old players selected from Monday March 31 to Thursday 1975-76 season. fans across the league to follow the and a maximum addition of two 16 April 3, 2014 at 3:00 p.m. process in real time online. year old wild carded players in any OHL Central Scouting Staff round of the OHL Priority Selection. OHL Central Scouting Chief Scout - Darrell Woodley The 2014 OHL Priority Selection pre- The Central Scouting Bureau of the GTA - Tim Cherry sented by State Farm will once again All other 16-year-old players selected Ontario Hockey League is an informa- Central Ontario - Kyle Branch be conducted online on Saturday April are eligible to be called up as an tion service and support organization Kingston and Area - John Finlay 5, 2014 beginning at 9:00 a.m. -
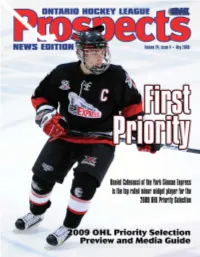
OHL Priority Selection Preview and Media Guide:OHL News.Qxd
OHL PRIORITY SELECTION OHL Priority Selection Process In 2001, the Ontario Hockey League Selected Players in the OHL with non-playoff teams selecting ahead Scouting Bureau with evaluations from conducted the annual Priority Selec- OHL Member Teams are permitted to of playoff teams. their team scouting staffs to make their tion process by way of the Internet for register a maximum of four 16 year old player selections. the first time in league history. players selected in the OHL Priority Teams are permitted to trade draft Selection. Those 16 year old players choices, other than their first round se- The OHL Central Scouting Bureau The new process allowed for eligible that are allowed to be signed are the lection, during the trading period from has been evaluating players since the players and their families, as well as fans first two 16 year old players selected Monday April 28 to Friday May 2, 1975-76 season. across the league to follow the process and a maximum addition of two 16 2008 at 3:00 p.m. in real time online. year old wild carded players in any OHL Central Scouting Staff round of the OHL Priority Selection. OHL Central Scouting Chief Scout - Robert Kitamura The 2008 OHL Priority Selection will The Central Scouting Bureau of the GTA - Tim Cherry once again be conducted online on All other 16-year-old players selected Ontario Hockey League is an informa- Central Ontario - Kyle Branch Saturday May 3, 2008 beginning at are eligible to be called up as an “affili- tion service and support organization Kingston and Area - John Finlay 9:00 a.m. -

2012-13 RIT Men's Ice Hockey
2012-13 RIT Men’s Ice Hockey RIT at American International Friday, November 2, 2012 (Olympia Ice Center, West Springfield, Mass. - 1,200) - 7:05 p.m. EST Saturday, November 3, 2012 (Olympia Ice Center, West Springfield, Mass. - 1,200) - 7:05 p.m. EST Radio Sports Information - 51 Lomb Memorial Drive - Clark Gym A261 - Rochester, NY 14623 Both Friday and Saturday’s games can be heard on WITR 89.7, with Chris Lerch and Nick Phelan Phone: (585) 475-6154 or (585) 475-5598 - Fax: (585) 475-2617 - Website: www.ritathletics.com bringing you all the action from the Olympia Ice Center. Fans can listen online at http://witr.rit.edu/ Joe Venniro: Director - [email protected] – Stephen Jaynes: Director - [email protected] Television About This Weekend/Looking to Get Back on Track... This Last 10 Meetings Between All 2012-13 RIT regular season and postseason RIT and AIC home games will be aired by Time Warner Cable weekend, the Tigers travel East on I-90, as they go to Atlantic Sports channel 26 or 1026 for HD Subscribers. Hockey Association rival American International to play a pair Date Place Score Gene Battaglia and John DiTullio bring you all the of games on Friday and Saturday against the Yellowjackets at 1/16/09 Ritter Arena W, 5-3 action from Ritter Arena. 1/17/09 Ritter Arena W, 6-1 7:05 p.m. The Tigers enter the weekend having lost four straight 1/22/10 at AIC W, 5-3 Video/Streaming Television games and look to avoid their first five-game losing streak since 1/23/10 at AIC W, 4-0 All RIT home games and selected road contests will October, 2009. -
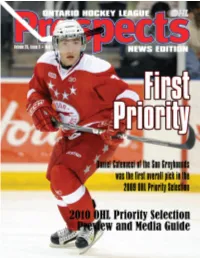
OHL Priority Selection Process
OHL PRIORITY SELECTION OHL Priority Selection Process In 2001, the Ontario Hockey League Selected Players in the OHL with non-playoff teams selecting ahead Scouting Bureau with evaluations from conducted the annual Priority Selec- OHL Member Teams are permitted to of playoff teams. their team scouting staffs to make their tion process by way of the Internet for register a maximum of four 16 year old player selections. the first time in league history. players selected in the OHL Priority Teams are permitted to trade draft Selection. Those 16 year old players choices, other than their first round se- The OHL Central Scouting Bureau The new process allowed for eligible that are allowed to be signed are the lection, during the trading period from has been evaluating players since the players and their families, as well as fans first two 16 year old players selected Monday April 26 to Friday April 30, 1975-76 season. across the league to follow the process and a maximum addition of two 16 2010 at 3:00 p.m. in real time online. year old wild carded players in any OHL Central Scouting Staff round of the OHL Priority Selection. OHL Central Scouting Chief Scout - Robert Kitamura The 2010 OHL Priority Selection will The Central Scouting Bureau of the GTA - Tim Cherry once again be conducted online on All other 16-year-old players selected Ontario Hockey League is an informa- Central Ontario - Kyle Branch Saturday May 1, 2010 beginning at are eligible to be called up as an “affili- tion service and support organization Kingston and Area - John Finlay 9:00 a.m. -

2012-13 RIT Men's Ice Hockey
2012-13 RIT Men’s Ice Hockey RIT vs. Mercyhurst; RIT vs. Canisius Friday, November 9, 2012 (Ritter Arena, Rochester, N.Y. - 2,100) - 7:05 p.m. EST Saturday, November 10, 2012 (Ritter Arena, Rochester, N.Y. - 2,100) - 7:05 p.m. EST Radio Sports Information - 51 Lomb Memorial Drive - Clark Gym A261 - Rochester, NY 14623 Both weekend games can be heard on WITR 89.7, with Chris Lerch, Scott Biggar. and Ed Trefzger Phone: (585) 475-6154 or (585) 475-5598 - Fax: (585) 475-2617 - Website: www.ritathletics.com bringing you all the action from Ritter Arena. Fans can listen online at http://witr.rit.edu/ Joe Venniro: Director - [email protected] – Stephen Jaynes: Director - [email protected] Television About This Weekend/Tigers Host Two Big Conference Last 10 Meetings Between All 2012-13 RIT regular season and postseason Contests... This The RIT men’s hockey team is back in action RIT and Mercyhurst home games will be aired by Time Warner Cable Date Place Score Sports channel 26 or 1026 for HD Subscribers. with a pair of early season Atlantic Hockey Association 12/13/08 Ritter Arena W, 5-3 Gene Battaglia and John DiTullio bring you all the games this weekend. On Friday, the Tigers host Mercyhurst at 3/20/09 % Blue Cross Arena L, 4-5 (OT) action from Ritter Arena. 7:05 p.m., then battle Canisius on Saturday night at 7:05 p.m. 11/13/09 at Mercyhurst W, 2-1 T.C. Riley’s and Park Point are Friday’s game sponsors, while Video/Streaming Television 11/14/09 at Mercyhurst W, 3-2 All RIT home games and selected road contests will Bugaboo Creek Steakhouse is Saturday’s sponsor.